
Single position, prone oblique lateral interbody fusion (OLIF)—case illustration and technical considerations
Highlight box
Surgical highlights
• With the patient in prone position throughout the surgery, we performed two levels oblique lateral interbody fusion (OLIF) procedure, direct neural decompression and long segment instrumentation.
What is conventional and what is novel/modified?
• Traditionally, the lateral lumbar interbody fusion is performed with the patient in lateral position and subsequently turned prone for posterior decompression and instrumentation. However, this process of patient repositioning and re-draping is tedious and prolongs anesthetic time.
• We describe performing the OLIF with posterior decompression and instrumentation in a single prone position.
What is the implication, and what should change now?
• This approach is not meant to replace other techniques or be used in all patients. Instead, it adds to our armamentarium for the management of spine fusion.
Introduction
The oblique lateral interbody fusion (OLIF) is a powerful minimally invasive spine fusion technique and is effective in managing degenerative and deformity cases. Compared to posterior approach, the lateral approach has the advantage of being able to insert a larger interbody cage for stability and fusion rates. It also helps with deformity correction, both in the sagittal and coronal plane. Further, the hallmark of the lateral approach is the ability to perform indirect decompression, avoiding the need to enter the spinal canal and therefore reducing the risk of cerebrospinal fluid (CSF) leaks, traction injury, post-op hematoma formation and cage extrusion from a posterior interbody procedure.
Traditionally, the lateral lumbar interbody fusion is performed with the patient in lateral position and subsequently turned prone for posterior decompression and instrumentation. However, this process of patient repositioning and re-draping is tedious and prolongs anesthetic time.
In recent years, surgeons have explored the option of single position surgery in a bid to shorten surgical time and cut costs. Literature reveals that single position lateral surgery (SPS-L) achieved shorter operative times and similar clinical/radiological outcomes compared to conventional dual (lateral then turned prone) position surgery (1). However, various problems were associated with this technique including a limitation to the number of levels that could be operated on, technically challenging pedicle screws insertion in lateral position, and difficulty performing posterior decompression if indicated.
More recently, authors have described a novel approach of performing the lateral lumbar interbody fusion in a single position prone surgery (SPS-P) (2). This approach was found to be effective at allowing the surgeon circumferential access to the spine without the need to reposition or re-drape the patient. At the same time, it was associated with benefits over the single lateral position approach including allowing multiple levels of disease to be addressed, able to achieve better lumbar lordosis from the positioning, more familiarity during pedicle screw insertion and direct posterior decompression if indicated (3).
The drawback for this, however, is the need to utilize a transpsoas approach which may be associated with more psoas related complications. Here, we explore the feasibility of performing the OLIF with posterior decompression and instrumentation in a single prone position. We aim to describe and explore the technical tips and nuances of this approach. We present this article in accordance with the SUPER reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-95/rc).
Case presentation
Our patient is a 75-year-old female who has medical history of hypertension, hyperlipidemia and diabetes. She also has history of spinal stenosis for which she underwent lumbar 3 to lumbar 5 decompression laminectomy 11 years prior to the writing of this report. She presented to us in clinic with symptoms of increasing unsteadiness of gait, associated with numbness over bilateral shins and ankles. On examination, motor power over bilateral L4 and L5 myotomes were Medical Research Council (MRC) grade 1. She mentioned this had been chronic since the previous decompression laminectomy. She was unable to ambulate over the past few months and was dependent on a wheelchair for mobilization.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this surgical technique and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. National Healthcare Group Domain Specific Review Board (NHG DSRB) approval was not required for this study (2023/00454).
Preoperative preparations and requirements
Index lumbar spine X-rays taken showed lumbar spondylosis with narrowing of intervertebral disc spaces, worst at L2/3 level. There was also grade 1 spondylolisthesis over L4/5. Flexion-extension views did not demonstrate any dynamic instability (Figure 1).

For further evaluation of her symptoms, magnetic resonance imaging (MRI) scan of her thoracolumbar spine was performed, which showed multilevel degeneration, worst at L2/3 causing significant canal stenosis and compression of the cauda equina. The scan also revealed that she had degeneration at T11/T12 level with compression of the spinal cord, possibly explaining her gait instability.
She was counselled and consented for surgery—OLIF of L2/3 and L3/4, posterior decompression of T11/12 and L2/3, and posterior instrumented fusion from T10–L4. She underwent the above surgery in a single prone position for both the OLIF and posterior decompression and instrumentation procedures at our tertiary spine center.
Step-by-step description
The patient was positioned prone on the Jackson table with cushion support over the patient’s chest, anterior superior iliac spine (ASIS) and thighs. Fluoroscopic images were taken to ensure the patient was placed in as true an anterior-posterior and lateral position as possible for X-ray intra-op. Placement of hip pads at the level of the posterior-superior iliac spine or slightly below can allow for better establishment of lumbar lordosis. Placement of a contralateral hip pad was also helpful in keeping the patient stable during discectomy (Figure 2A).

Localization was performed with a metal wire, marking out the direction of the disc space of interest—in this case, L2/3 and L3/4. This helped to determine the incision site and orientates the radiographer for accurate angulation of the fluoroscopy during the operation. The incision was localized approximately 3 to 5 cm along the midportion of the anteroposterior diameter of the disc space. A 5 cm incision was made centered upon the 2 target disc spaces to be treated (Figure 2B).
The patient was then draped widely to allow sterile access to both the lateral incision for OLIF and posterior incision for subsequent posterior decompression and instrumentation (Figure 2C). The lateral incision was then made, and the external oblique fascia was opened with electrocautery. Blunt dissection was performed with Langenbeck retractors through the external oblique, internal oblique and transverse abdominis muscles along the direction of their muscle fibers. The retroperitoneal space was accessed via blunt dissection with a gauze swab on a stick and the peritoneal contents were mobilized anteriorly (Figure 3A). Upon entering the retroperitoneal space, the peritoneum was swept anteriorly exposing the psoas muscle (Figure 3B). The psoas muscle was identified and retracted posteriorly by an assistant standing on the opposite site of the operating table.

Once the psoas muscle was retracted posteriorly, the disc space could be visualized and palpated. A wire was inserted through the disc space and fluoroscopic images obtained to confirm the surgical level (Figure 4A). If navigation technology is used, the navigated MAST dilator (Medtronic, Minneapolis, MN, USA) can also be used for similar effect. Sequential dilators are placed through the wire to displace the surrounding tissues. A pair of bladed retractors were placed over the dilators and held in place by flex arms anchored to the operating table (Figure 4B). It is important to ensure stability of the retractor system, avoiding slipping or loosening throughout the operation to prevent loss of visualization.

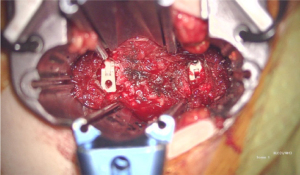
Upon visualization of the disc space (Figure 5) and confirmation with fluoroscopy, annulotomy was performed and discectomy achieved in the usual fashion with the surgeon in a seated position on the patient’s lateral side (Figure 6). The vertebral end plates were prepared and the contralateral annulus was released. Sequential trials were used to distract and open up the disc space, applying appropriate tension to the disc space to achieve indirect decompression. The correspondingly sized cage was then loaded with bone graft and impacted into position under fluoroscopic guidance via a press fit fashion. The similar process was repeated for the other target disc level (Figure 7).
Layered closure was then performed to the abdominal muscle planes sequentially. Subcutaneous and subcuticular closure can be performed by the assisting surgeon, while the main surgeon can proceed to begin with exposure for the posterior decompression and instrumentation subsequently. The intra-operative fluoroscopic and post-operative X-ray images are presented in Figure 8.
Postoperative considerations and tasks
Post-operatively the patient experienced pain over the left anterior thigh which was well managed on analgesia. There was mild weakness of left hip flexion of MRC grade 4, but weakness resolved on discharge. She was discharged home on post-op day 10. Her mJOA (Modified Japanese Orthopaedic Association) score improved from 12 preoperatively to 15 postoperatively.
Tips and pearls
We summarize the tips and pearls learnt while performing this case.
Firstly, when positioning the patient in prone, it is helpful to place hip pads at the level of the posterior superior iliac spine or slightly more inferior. This aids to better establish the lumbar lordosis as discussed. They also serve to ensure stability of the patient during the surgery especially during discectomy and cage implantation subsequently.
After bladed retractors are placed and held in place by the flex arms fixed to the operating table, stability can be improved by ensuring that the hinge of the flex arms rest firmly supported by green towels. The retractors can also be fixed to the vertebral body using a pin. The pin should be placed near the endplates of the vertebral body to avoid injury to the segmental vessels located midbody.
Finally, after cage implantation is complete, simultaneous closure of the lateral wound and exposure for the posterior decompression and instrumentation can be performed, making the surgical process more time efficient.
Discussion
SPS-P has been described as an alternative approach to the single position lateral approach. While most cases describe a transpsoas prone lateral approach, this case report describes a novel approach of performing the OLIF surgery with the patient in a prone position in contrary to the conventional lateral position.
There are several advantages of prone lateral surgery. As a single position approach, the need to reposition the patient is eliminated, saving costs of surgical drapes and conserves surgical time. The prone position also offers ample space for surgeons to work simultaneously in terms of exposure, instrumentation, decompression and closure. This approach was recently described by Lamartina and Berjano with a comparison between the single position lateral versus prone surgery, demonstrating a shorter set up and positioning time with similar success rates in implantation across the two groups of patients (2).
Prone position surgery also allows for better achievement of positional lordosis of the lumbar spine (4). By placement of hip pads at the level of the posterior-superior iliac spine or slightly below, most significant lumbar lordosis can be achieved through positional effect for superior deformity correction (4,5). In our patient, post-operative computerized tomography scan demonstrated a mild improvement of lumbar lordosis from 32.7 degrees preoperatively to 40.6 degrees post-operatively (Figure 9).

The prone lateral approach is especially useful when multiple levels of degeneration need to be addressed, as it allows for simultaneous posterior and lateral approaches to the spine in a single position. It is also useful for simultaneous manipulation whereby posterior releases and decompression can be performed whilst a lateral cage can be inserted followed by sagittal realignment with posterior instrumentation.
Subsequently, it is also much more surgeon friendly to insert pedicle screws with the patient in prone rather than lateral (6). This allows the surgeon to target more levels compared to lateral position. At the same time, having the patient in prone also offers the surgeon the option of direct posterior decompression if required.
Also, studies have demonstrated that extension of the thigh with the patient in prone position effectively draws the femoral neve within the lumbar plexus being positioned more posteriorly, making the approach safer to perform. Through cadaveric studies, the femoral nerve position was found to be relatively more posterior in the prone position (18% from the posterior edge of the L4–L5 disc space) compared to the lateral decubitus position (28%) (7).
If navigation is to be used, we have found that the prone position is more stable compared to the lateral position as there is less toggle and movement as the patient is secured firmly on a Jackson table by hip pads in the prone position, rather than held in position by straps and tape in the lateral position. Navigation also reduces the amount of radiation to the surgical team especially in the setting of lateral surgery, where locating the disc space and screw placement may require multiple fluoroscopy images.
Despite its benefits, we also recognized various challenges during the surgery. Firstly, gravity forces the retractor downwards and therefore retractor placement and stability through the surgery is crucial. To avoid this issue, it is important to ensure the flex arms hinge is resting firmly supported by surgical towels as previously mentioned, and the use of a pin to fix the retractor system to the vertebral body.
Lower lumbar and lumbosacral levels may be hard to access via the lateral approach due to the larger psoas bulk and iliac crest anatomy. Maneuvering of instruments would also be challenging. It is important to review pre-op MRI scans and identify patients with large psoas bulk or rising psoas sign to identify cases where the lateral approach would be challenging with a higher risk of nerve injury (8). For L5/S1 pathology, it is not possible to insert a large interbody cage from the side due to anatomical challenges from the iliac crest. As such, if a surgeon needs to address L5/S1 pathology, alternative options would include performing an ALIF followed by a prone-lateral, a prone-lateral with a L5/S1 transforaminal lumbar interbody fusion (TLIF), or dual position lateral and posterior surgery to address all segments involved.
We also observe in obese patients with larger abdominal girth, the abdominal soft tissue tends to splay outwards when positioned prone. As such, deeper and longer retractors are required to reach the disc space. This compromises visualization, makes ergonomics for discectomy less efficient as instruments are much longer, and there is a greater propensity for retractor loosening (9).
The relative advantages and disadvantages of the single position prone lateral approach versus the standard lateral approach is summarized in Table 1.
Table 1
| Approach | Prone lateral | Standard lateral |
|---|---|---|
| Lumbar lordosis | Advantage (3) | Disadvantage |
| Direct decompression | Advantage (2,3) | Disadvantage |
| Pedicle screw insertion | Advantage (5) | Disadvantage |
| Navigation stability | Advantage (1) | Disadvantage |
| Lower lumbar levels | Disadvantage (5) | Advantage |
| Patient obesity | Disadvantage (9) | Advantage |
We feel that the prone lateral or prone OLIF procedure might be particularly useful to manage upper lumbar pathology, compared to the lower levels where a bulky psoas, large habitus and iliac crest might make instrumentation more challenging. The ideal candidate will be a patient with a previous L4–S1 spinal fusion but now presents with adjacent segment degeneration. With this procedure, interbody cages can be inserted using an OLIF approach, while performing simultaneous instrumentation posteriorly.
Conclusions
Single position prone lateral surgery is a powerful approach which offers many advantages over alternatives such as dual position surgery and single lateral position surgery. However, there are unique challenges for this approach that needs to be taken into consideration prior to surgery.
Hence, we believe that single position prone lateral approach does not necessarily replace other conventional approaches due to the limitations described above. Careful patient selection is important to identify the most suitable candidates is important to harness to reap the full benefits of this approach.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-95/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-95/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-23-95/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this surgical technique and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. National Healthcare Group Domain Specific Review Board (NHG DSRB) approval was not required for this study (2023/00454).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ouchida J, Kanemura T, Satake K, et al. Simultaneous single-position lateral interbody fusion and percutaneous pedicle screw fixation using O-arm-based navigation reduces the occupancy time of the operating room. Eur Spine J 2020;29:1277-86. [Crossref] [PubMed]
- Lamartina C, Berjano P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): preliminary results. Eur Spine J 2020;29:6-13. [Crossref] [PubMed]
- Ziino C, Konopka JA, Ajiboye RM, et al. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg 2018;4:717-24. [Crossref] [PubMed]
- Soliman MAR, Aguirre AO, Ruggiero N, et al. Comparison of prone transpsoas lateral lumbar interbody fusion and transforaminal lumbar interbody fusion for degenerative lumbar spine disease: A retrospective radiographic propensity score-matched analysis. Clin Neurol Neurosurg 2022;213:107105. [Crossref] [PubMed]
- Mills ES, Treloar J, Idowu O, et al. Single position lumbar fusion: a systematic review and meta-analysis. Spine J 2022;22:429-43. [Crossref] [PubMed]
- Blizzard DJ, Thomas JA. MIS Single-position Lateral and Oblique Lateral Lumbar Interbody Fusion and Bilateral Pedicle Screw Fixation: Feasibility and Perioperative Results. Spine (Phila Pa 1976) 2018;43:440-6. [Crossref] [PubMed]
- Alluri R, Clark N, Sheha E, et al. Location of the Femoral Nerve in the Lateral Decubitus Versus Prone Position. Global Spine J 2023;13:1765-70. [Crossref] [PubMed]
- Ng JP, Kaliya-Perumal AK, Tandon AA, et al. The Oblique Corridor at L4-L5: A Radiographic-Anatomical Study Into the Feasibility for Lateral Interbody Fusion. Spine (Phila Pa 1976) 2020;45:E552-9. [Crossref] [PubMed]
- Godzik J, Ohiorhenuan IE, Xu DS, et al. Single-position prone lateral approach: cadaveric feasibility study and early clinical experience. Neurosurg Focus 2020;49:E15. [Crossref] [PubMed]





