Cervical sagittal parameters in degenerative cervical spondylolisthesis versus degenerative cervical kyphosis with myeloradiculopathy treated by anterior cervical discectomy and fusion
Highlight box
Key findings
• Anterior cervical discectomy and fusion (ACDF) provides significant improvement in C2-C7 angle in degenerative cervical kyphosis.
• After surgery, degenerative cervical spondylolisthesis group has no significantly different parameters compare to before surgery.
• Postoperative cervical sagittal parameters of all patients in the study are within the normal thresholds (T1 slope minus C2-C7 lordosis <15° and C2-C7 sagittal vertical axis <40 mm.
What is known and what is new?
• The mismatch between T1 slope and cervical lordosis more than 15 degrees caused poorer health-related quality-of-life scores including neck pain and disability.
• T1 slopes in both groups are similar, but neck tilt angle and thoracic inlet angle show difference between two groups.
What is the implication, and what should change now?
• Segment-by-segment ACDF surgery may be more effective than a single long anterior construct reconstruction in correcting abnormal regional cervical sagittal parameters.
Introduction
Adult spinal deformity, especially sagittal imbalance, is affecting the health-related quality-of-life (HRQOL) scores (1,2). In the past, the common parameters used to define sagittal profile include the C7 sagittal vertical axis (C7 SVA) that was the most reliable predictor of HRQOL scores, regional Cobb angle, pelvic tilt, sacral slope and pelvic incidence (2). During the last decade, the cervical sagittal parameters include C0-C2 angle, C1-C2 angle, C2-C7 angle, C2-C7 SVA and T1 slope became highlighted which related to the HRQOL scores and surgical outcome as well as thoracolumbar sagittal alignment (3).
The cervical sagittal malalignment, particularly cervical kyphosis, has been associated with myelopathy even without central stenosis from increasing the longitudinal cord tension (4). There are many classifications of sagittal deformity such as Ames-International Spine Study Group (ISSG), Kim-ISSG that focus on the location of cervical deformity (cranio-vertebral junction, focal cervical spine, cervico-thoracic junction, thoracic spine) and Cervical Spine Research Society (CSRS)-Europe which focus on regional and global balance to guide the plan of surgical treatment (5).There are limited amounts of the study focusing on degenerative sagittal cervical characters especially degenerative cervical spondylolisthesis which may be different to degenerative cervical kyphosis.
The aim of the study is to determine the preoperative and postoperative cervical sagittal parameters in patients with degenerative cervical spondylolisthesis and degenerative cervical kyphosis with myeloradiculopathy and to identify the different cervical sagittal parameters that may concern and guide for surgical planning due to the cervical sagittal profiles that affect to functionality, surgical outcome and global spine sagittal balance (3,4,6,7). We present this article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-23-107/rc).
Methods
Study design
This is retrospective cohort study that included 30 adult patients (more than 18-year-old). Fifteen patients with degenerative cervical spondylolisthesis and 15 patients with degenerative cervical kyphosis have been performed anterior cervical discectomy and fusion (ACDF) at Department of Orthopaedics, Faculty of Medicine, Chiang Mai University during January 2010 and December 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Faculty of Medicine, Chiang Mai University (Ethics Approval No. ORT-2565-09160) and informed consent was obtained from all individual participants. All patient information and imaging data were extracted from medical records. The inclusion criteria were the patients suffering moderate-to-severe cervical myeloradiculopathy (average Nurick’s disability score =3.9 and JOA score =7.7) from degenerative cervical spondylolisthesis and degenerative cervical kyphosis. The exclusion criteria were as follows: spinal trauma, neoplasms, infections, history of cervical spine or neck surgery and concomitant thoracic and lumbar symptoms. Artificial Intelligence (AI) tools were not applied in the writing of a manuscript, production of the images or graphical elements of the paper, or in the collection and analysis of data.
Pre-operative and post-operative patient’s information measurements
All demographic data [age, gender, body mass index (BMI), underlying disease(s), smoking, Nurick’s disability score, Japanese Orthopaedic Association (JOA) score (8), levels of pathology and levels of ACDF] were recorded at pre-operative and post-operative periods of 6 to 24 months.
Surgical techniques & postoperative immobilization
We used the standard Smith-Robinson techniques. Surgical tactics to correct cervical spondylolisthesis were performing one-by-one, segment-by-segment anterior cervical discectomy and release, bilateral partial uncinatectomies and posterior longitudinal ligament (PLL) resection. During anterior plate fixation, we reduced the olisthesis vertebrae by placing the screws and pulled them toward the contoured plate (Figure 1).
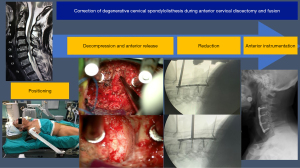
In kyphotic patients, we positioned the patient’s neck in slightly extended position and intentionally placed the vertebral distraction pins in divergent position. After performing anterior discectomies and releases, we carefully fashioned and placed the grafts (or cages) in lordotic position. Finally, we manually bent the plate and placed it in very low-profile manner (Figure 2).

After surgery, we placed the patients in postoperative bracing for 2–3 months until achieving the bony union.
Pre-operative and post-operative radiographic cervical sagittal parameter measurements
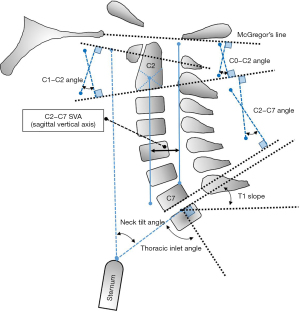
Lateral cervical standing or an upright radiographic study of each patient was performed before surgery and 6 to 24 months after surgery and recorded on picture archiving and communication system of Faculty of Medicine, Chiang Mai University. The spinal parameters were assessed: (I) C0-C2 lordosis angle, (II) C1-C2 lordosis angle, (III) C2-C7 lordosis angle, (IV) C2-C7 SVA, (V) T1 slope, (VI) neck tilt angle, (VII) thoracic inlet angle (Figure 3) and measured on pre-operative and post-operative films (Figure 4).
Cervical sagittal parameters
C0-C2 lordosis angle was defined as the angle between McGregor’s line that refer to occipital baseline and lower endplate of C2 (9). The increasing of C0-2 angle occurs in patients with subaxial cervical spine kyphosis. C1-C2 lordosis angle was defined as the angle between line of central axis of C1 (line between the centers of anterior and posterior arch of C1) and lower endplate of C2 which reflects lordosis of upper cervical spine. C2-C7 lordosis angle was defined as the angle between lower endplate of C2 and C7. C2-C7 SVA measurement was performed by using the horizontal distance between a plumb line of center of the C2 and the superior-posterior aspect of the C7. T1 slope was measured by using the angle from the parallel line to the superior end plate of the T1 and the horizontal line of the center of the superior end plate of the T1. The relationship between C2-C7 lordosis and the T1 slope is similar to the relationship between pelvic incidence and lumbar lordosis (4). Neck tilt angle was defined as angle between line from center of superior endplate of the T1 to the upper endplate of sternum and vertical line. Thoracic inlet angle was calculated by using angle between perpendicular line of the superior endplate of the T1 and line from center of superior endplate of the T1 to the upper endplate of sternum. The thoracic inlet angle equals neck tilt angle plus T1 slope that similar to pelvic incidence equals the pelvic tilt plus the sacral slope in the lumbar spine (10).
Statistical analysis
All statistical analyses were conducted using R version 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria). Normally distributed data were analyzed with the Kolmogorov-Smirnov test. The data of both the degenerative cervical spondylolisthesis group and the degenerative cervical kyphosis group were normally distributed. Comparisons of group means, and variances were carried out using a student’s t-test. The level of statistical significance was set at 0.05.
Results
This retrospective cohort study included 30 adult patients. Fifteen patients were degenerative cervical spondylolisthesis, ten males and five females. The average age of spondylolisthesis group was 66.64±9.86 years, and the average BMI was 20.47±1.91 kg/m2. Fifteen patients were degenerative cervical kyphosis, nine males and six females. The average age of kyphosis group was 65.22±9.39 years, and the average BMI was 20.87±2.21 kg/m2. All of these patients had severe cervical myelopathy that pre-operative Nurick scale and JOA score were 3.87±1.13 and 7.93±2.46 for degenerative cervical spondylolisthesis group and 3.93±1.33 and 7.50±2.44 for degenerative cervical kyphosis group. General information and clinical presentation of cervical myelopathy before surgery between two groups were not significant difference. Patients with degenerative cervical spondylolisthesis have been performed 2.6±0.986 levels of ACDF while patients with degenerative cervical kyphosis have been performed 3.4±0.986 levels of ACDF. However, there was no significant difference post-operative JOA score between patients with degenerative cervical spondylolisthesis (10±2.16) and patients with degenerative cervical kyphosis (9.71±2.23) that improved compare with before surgery (Table 1).
Table 1
| Characteristics | Degenerative cervical spondylolisthesis group (n=15) |
Degenerative cervical kyphosis group (n=15) |
P value |
|---|---|---|---|
| General information | |||
| Age (years) | 66.64±9.86 | 65.22±9.39 | 0.756 |
| Male | 10 (66.67) | 9 (60.00) | – |
| Female | 5 (33.33) | 6 (40.00) | – |
| Weight (kg) | 52.18±6.52 | 50.17±6.24 | 0.555 |
| Height (cm) | 159.5±6.17 | 155±5.51 | 0.152 |
| BMI (kg/m2) | 20.47±1.91 | 20.87±2.21 | 0.682 |
| Underlying diseases | |||
| Cardiovascular disease | 7 (46.67) | 4 (26.67) | – |
| Diabetes mellitus | 0 (0) | 1 (6.67) | |
| Cardiovascular disease with diabetes mellitus | 1 (6.67) | 1 (6.67) | |
| No underlying disease | 7 (46.67) | 9 (60.00) | – |
| Smokers | 7 (46.67) | 5 (33.33) | – |
| Non-smokers | 8 (53.33) | 10 (66.67) | – |
| Preoperative clinical measures | |||
| Cervical myelopathy | 15 (100.00) | 15 (100.00) | – |
| Level of pathology (level) | 2.4±0.737 | 3.07±0.704 | 0.011* |
| Nurick Scale (grade) | 3.87±1.13 | 3.93±1.33 | 0.809 |
| JOA score (points) | 7.93±2.46 | 7.50±2.44 | 0.677 |
| Operative procedures | |||
| ACDF (level) | 2.6±0.986 | 3.4±0.986 | 0.025* |
| ACDF 1-level | 2 (13.33) | 0 (0) | – |
| ACDF 2-level | 5 (33.33) | 3 (20.00) | – |
| ACDF 3-level | 5 (33.33) | 5 (33.33) | – |
| ACDF 4-level | 3 (20.00) | 5 (33.33) | – |
| ACDF 5-level | 0 (0) | 2 (13.33) | – |
| Final follow-up clinical measures | |||
| Nurick Scale (grade) | 3.0±1.10 | 2.85±1.41 | 0.841 |
| JOA score (points) | 10.0±2.16 | 9.71±2.23 | 0.783 |
| Follow-up duration (months) | 24.50±1.50 | 24.80±2.50 | 0.325 |
*, P<0.05. BMI, body mass index; JOA score, Japanese Orthopaedic Association Score; ACDF, anterior cervical discectomy and fusion; SD, standard deviation.
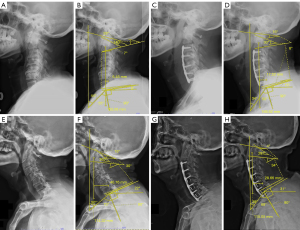
Comparison of cervical sagittal alignment between before and after surgery
No significant differences were found in the comparison of preoperative and postoperative cervical sagittal parameters in patients with degenerative cervical spondylolisthesis that include C0-C2 lordosis angle, C1-C2 lordosis angle, C2-C7 lordosis angle, C2-C7 SVA, T1 slope, neck tilt angle and thoracic inlet angle. There was significant increase of C2-C7 lordosis angle in the patients with degenerative cervical kyphosis group comparing before (−14.88±7.32) and after surgery (4.10±11.80). There was also a significant difference in the C0-C2 lordosis angle before (31.13±7.68) and after surgery (17.43±12.70). The C1-C2 lordosis angle was also significantly reduced in this group when comparing before (37.88±5.08) and after surgery (23.30±11.60). All of comparison of cervical sagittal alignment between before and after surgery showed in Tables 2,3.
Table 2
| Degenerative cervical spondylolisthesis group |
Preoperative measurement (n=15) |
Postoperative measurement at 2 years (n=15) |
P value |
|---|---|---|---|
| Sagittal alignment parameters | |||
| C0-C2 angle (degree) | 13.00±10.20 | 14.43±8.83 | 0.778 |
| C1-C2 angle (degree) | 24.60±10.70 | 23.57±8.46 | 0.857 |
| C2-C7 angle (degree) | 9.60±13.60 | 17.40±10.00 | 0.242 |
| C2-C7 SVA (mm) | 33.22±13.92 | 27.80±9.86 | 0.425 |
| T1 slope (degree) | 17.20±10.5 | 22.17±8.38 | 0.418 |
| Neck tilt angle (degree) | 57.71±8.75 | 51.71±6.63 | 0.179 |
| Thoracic inlet angle (degree) | 75.10±14.20 | 74.57±5.41 | 0.930 |
SVA, sagittal vertical axis; SD, standard deviation.
Table 3
| Degenerative cervical kyphosis group | Preoperative measurement (n=15) |
Postoperative measurement at 2 years (n=15) |
P value |
|---|---|---|---|
| Sagittal alignment parameters | |||
| C0-C2 angle (degree) | 31.13±7.68 | 17.43±12.70 | 0.035* |
| C1-C2 angle (degree) | 37.88±5.08 | 23.30±11.60 | 0.015* |
| C2-C7 angle (degree) | −14.88±7.32 | 4.10±11.80 | 0.005* |
| C2-C7 SVA (mm) | 13.70±13.60 | 17.05±6.40 | 0.569 |
| T1 slope (degree) | 10.13±5.08 | 16.57±7.32 | 0.077 |
| Neck tilt angle (degree) | 46.75±7.09 | 45.29±9.81 | 0.758 |
| Thoracic inlet angle (degree) | 57.63±8.38 | 62.43±6.90 | 0.242 |
*, P<0.05. SVA, sagittal vertical axis; SD, standard deviation.
Comparison of cervical sagittal alignment between degenerative cervical spondylolisthesis and degenerative cervical kyphosis
With pre-operative measurement, patients with degenerative cervical kyphosis had C2-C7 lordosis angle (−14.88±7.32) less than patients with degenerative cervical spondylolisthesis (9.60±13.60) (P<0.05) while T1 slope was not significant difference in both groups, causing the mismatch between T1 slope and C2-C7 lordosis angle of kyphosis group more than spondylolisthesis group. Hypolordosis or kyphosis of C2-C7 angle led to hyperlordosis of C0-C2 angle and C1-C2 angle in patients with degenerative cervical kyphosis (31.13±7.68, 37.88±5.08) comparing with spondylolisthesis group (13±10.20, 24.60±10.70) (P<0.05). Whereas patients with degenerative cervical spondylolisthesis had C2-C7 SVA (33.22±13.92) more than kyphosis group (13.70±13.60) (P<0.05). Patients with degenerative cervical kyphosis exhibited a lower C2-C7 lordosis angle after surgery than patients with degenerative cervical spondylolisthesis (4.10±11.80, 17.40±10.0) (P<0.05). As same as the C2-C7 angle, patients with degenerative cervical kyphosis exhibited a lower C2-C7 SVA (17.05±6.40, 27.80±9.86) (P<0.05) after surgery than patients with degenerative cervical spondylolisthesis. All cervical parameters were shown in Table 4.
Table 4
| Sagittal alignment parameter | Preoperative measurement | Postoperative measurement at 2 years | |||||
|---|---|---|---|---|---|---|---|
| Degenerative cervical spondylolisthesis (n=15) | Degenerative cervical kyphosis (n=15) | P value | Degenerative cervical spondylolisthesis (n=15) | Degenerative cervical kyphosis (n=15) | P value | ||
| C0-C2 angle (degree) | 13.00±10.20 | 31.13±7.68 | 0.003* | 14.43±8.83 | 17.43±12.70 | 0.613 | |
| C1-C2 angle (degree) | 24.60±10.70 | 37.88±5.08 | 0.017* | 23.57±8.46 | 23.30±11.60 | 0.966 | |
| C2-C7 angle (degree) | 9.60±13.60 | −14.88±7.32 | 0.003* | 17.40±10.0 | 4.10±11.80 | 0.044* | |
| C2-C7 SVA (mm) | 33.22±13.92 | 13.70±13.60 | 0.021* | 27.80±9.86 | 17.05±6.40 | 0.037* | |
| T1 slope (degree) | 17.20±10.50 | 10.13±5.08 | 0.090 | 22.17±8.38 | 16.57±7.32 | 0.219 | |
| Neck tilt angle (degree) | 57.71±8.75 | 46.75±7.09 | 0.023* | 51.71±6.63 | 45.29±9.81 | 0.184 | |
| Thoracic inlet angle (degree) | 75.10±14.20 | 57.63±8.38 | 0.019* | 74.57±5.41 | 62.43±6.90 | 0.004* | |
*, P<0.05. SVA, sagittal vertical axis; SD, standard deviation.
Discussion
Cervical sagittal malalignment is related to HRQOL score similar to thoracolumbar sagittal malalignment. There are many sagittal cervical parameters that correlate with patient’s quality of life. In 2012, Tang et al. (3) reported positive C2-C7 SVA more than 40 mm was the most significant correlation with neck disability index (NDI) (3). Lee et al. (10) proposed the relationship between T1 slope and C2-C7 lordosis angle that a high T1 slope required a high magnitude of cervical lordosis to balance the head over the thoracic inlet and trunk (10). The mismatch between T1 slope and cervical lordosis more than 15 degrees caused poorer HRQOL including neck pain and disability (4).
The common cervical deformity which is described in former studies is cervical kyphosis but does not mention to other deformity such as spondylolisthesis that can cause cervical sagittal imbalance, neck pain, radiculopathy and myelopathy (11). This study focuses on cervical sagittal parameters between the patients having degenerative cervical spondylolisthesis and degenerative cervical kyphosis with severe myeloradiculopathy. Patients with degenerative cervical kyphosis have hypolordosis or kyphosis of C2-C7 angle and increase the mismatch between T1 slope and C2-C7 angle that cause increasing the longitudinal cord tension due to the cervical spinal cord being tethered by the dentate ligaments and cervical nerve roots (7).
Although Hardacker et al. (12) found that the majority of cervical lordosis, the natural inward curvature of the cervical spine, was concentrated at the uppermost levels (C1-C2) when individuals were in a standing position. Conversely, only a small percentage (15%) of cervical lordosis was observed at the lower three cervical levels (C4-C7). Furthermore, the study highlighted an inverse correlation between alterations in cervical lordosis and changes in thoracic alignment. This indicated that changes in the curvature of the cervical spine were related to changes in the alignment of the thoracic (mid-back) region (12). The conclusion underscored craniovertebral junction (CVJ) deformity as a challenging condition leading to progressive deformity, myelopathy, severe neck pain, and functional limitations like difficulty swallowing. Surgical management of this deformity is complicated due to intricate anatomical relationships with surrounding neurovascular structures and complex biochemical considerations, making access to this region challenging (13).
The main sagittal imbalance of patients with degenerative cervical spondylolisthesis is C2-C7 SVA that is greater than kyphotic group and there is severe myelopathy even though the C2-C7 SVA less than predicted threshold (≥40 mm) as reported by Tang et al. (3). Also, the predicted threshold of C2-C7 SVA of patients with degenerative cervical spondylolisthesis may be less than the previous studies.
Disabling cervical myeloradiculopathy in all 30 patients has clinically improved while comparing before and after surgery in time of follow-up. All patients were performed ACDF. This surgical procedure directly decompresses the neural structures, restores cervical lordosis and corrects deformity. Gillis et al. (14) demonstrated that single-level ACDF improved the segmental cervical lordosis by 6.45° and the overall C2-C7 cervical lordosis by 3.46° at one year (14). In addition, the authors further stated that multi-level ACDF was more effective than a single long corpectomy construct in restoring lordosis, as multi-level cervical discectomy provided multiple distraction points (15). In our study, the cervical sagittal parameters, especially C2-C7 angle, in patients with degenerative cervical kyphosis significantly improve compared to before surgery while the parameters of patients with degenerative cervical spondylolisthesis are not significantly different compared before and after surgery. This may be caused by divergent placement of the vertebral distraction pins, lordotic preparation of disc spaces and applying of lordotic cages and/or grafts segment-by-segment which has been intentionally performed in kyphosis more than in spondylolisthesis. Moreover, the numbers of operative level of ACDF in patients with degenerative cervical kyphosis are higher than patients with degenerative cervical spondylolisthesis that may improve the overall corrective parameters. However, the postoperative cervical sagittal parameters of all patients in this study are within the normal thresholds (T1 Slope minus C2-C7 lordosis <15° and C2-C7 SVA <40 mm) (4).
Nevertheless, we have indicated some difference of sagittal parameters between the spondylolisthesis and kyphosis. T1 slopes are both similar but neck tilt angle and thoracic inlet angle show difference between two groups. It may draw a discussion that the large thoracic inlet angle can be an underlying factor to progress toward cervical spondylolisthesis and future treatment planning.
Limitations of this study includes the followings. First, the sagittal balance depends on local, regional and global parameters. We are not able to perform standing full-length whole spine radiographs in all patients because of profound cervical myelopathy involving residual lower extremity weakness. Second, we think that surgical treatment in patients with moderate-to-severe degenerative cervical myeloradiculopathy is mainly neural decompression and stabilization. Sagittal imbalance correction may be the second prioritized importance, so we focus our primary concentration in removing degenerative disc diseases and impinging osteophytes. Lastly, it is a retrospective design and has a smaller number of patients.
Conclusions
The study demonstrates the difference of sagittal parameters between degenerative cervical spondylolisthesis and kyphosis before and after surgery. ACDF not only provides neural decompressive procedure, but also corrects the regional cervical sagittal parameters.
Acknowledgments
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-23-107/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-107/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-23-107/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form available at https://jss.amegroups.com/article/view/10.21037/jss-23-107/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Faculty of Medicine, Chiang Mai University (Ethics Approval No. ORT-2565-09160) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Djurasovic M, Glassman SD. Correlation of radiographic and clinical findings in spinal deformities. Neurosurg Clin N Am 2007;18:223-7. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012;71:662-9; discussion 669. [Crossref] [PubMed]
- Scheer JK, Lau D, Smith JS, et al. Alignment, Classification, Clinical Evaluation, and Surgical Treatment for Adult Cervical Deformity: A Complete Guide. Neurosurgery 2021;88:864-83. [Crossref] [PubMed]
- Sivaganesan A, Smith JS, Kim HJ. Cervical Deformity: Evaluation, Classification, and Surgical Planning. Neurospine 2020;17:833-42. [Crossref] [PubMed]
- Han K, Lu C, Li J, et al. Surgical treatment of cervical kyphosis. Eur Spine J 2011;20:523-36. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Oshima Y, Takeshita K, Kato S, et al. Comparison Between the Japanese Orthopaedic Association (JOA) Score and Patient-Reported JOA (PRO-JOA) Score to Evaluate Surgical Outcomes of Degenerative Cervical Myelopathy. Global Spine J 2022;12:795-800. [Crossref] [PubMed]
- Dohzono S, Toyoda H, Takahashi S, et al. Restrictions of cervical flexion after laminoplasty increase in the mechanical stress at the occipitocervical junction in non-rheumatoid arthritis patients. J Clin Neurosci 2017;45:187-92. [Crossref] [PubMed]
- Lee SH, Kim KT, Seo EM, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 2012;25:E41-7. [Crossref] [PubMed]
- Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop 2011;35:869-75. [Crossref] [PubMed]
- Hardacker JW, Shuford RF, Capicotto PN, et al. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 1997;22:1472-80; discussion 1480. [Crossref] [PubMed]
- Hong JT, Kim IS, Lee HJ, et al. Evaluation and Surgical Planning for Craniovertebral Junction Deformity. Neurospine 2020;17:554-67. [Crossref] [PubMed]
- Gillis CC, Kaszuba MC, Traynelis VC. Cervical radiographic parameters in 1- and 2-level anterior cervical discectomy and fusion. J Neurosurg Spine 2016;25:421-9. [Crossref] [PubMed]
- Ogura Y, Dimar JR, Djurasovic M, et al. Etiology and treatment of cervical kyphosis: state of the art review-a narrative review. J Spine Surg 2021;7:422-33. [Crossref] [PubMed]