
CT guided percutaneous vertebroplasty of C2 osteolytic lesion: a case report and technical note
Introduction
Spine metastases are found in up to 30% of patients with malignant tumors. Cervical spine is the least affected, accounting for only 10% to 15% of spinal secondary localizations (1). Metastatic lesions of C2 are rare, found in only 2% of spinal metastasis (2).
Treatment is usually conservative, with the main goal of pain control and vertebral stability. It includes medical pain management, immobilization using cervical hard collar and radiation therapy (1). In cases of refractory pain, neurological involvement or spinal instability, surgical stabilization and vertebroplasty are used as palliative options (2,3). While surgical options, including anterior cervical corpectomy and posterior laminectomy and fusion, allow neural decompression and vertebral stabilization, they are associated with high rates of morbidity and complications (4).
Vertebroplasty is a minimally invasive technique widely used in the treatment of vertebral osteolytic lesion and compression fractures. It can provide rapid and durable pain relief in up to 85% of cases (2,5), as well as vertebral stabilization. Compared to open surgical approaches, vertebroplasty requires shorter surgical and anesthesia time with less blood loss, and lower complication rates (6,7). In a previous report, we described the surgical technique for C2 vertebroplasty using an anterolateral approach, with satisfactory results (8). Few studies reported percutaneous CT guided vertebroplasty using transoral(9,10), anterolateral (11) and direct lateral (12) approaches. Excellent results were obtained in all the reported series, with low complication rates. However, most cases were done under general anesthesia and required patients’ hospitalization. In this paper, we present a new direct percutaneous anterolateral C2 vertebroplasty approach, that can be done under conscious sedation, as an ambulatory/outpatient procedure. We present the following case in accordance with the CARE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-21-97/rc).
Case presentation
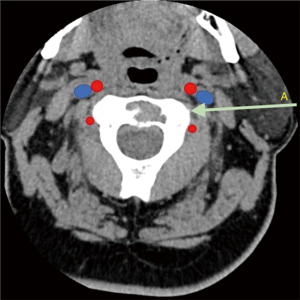
We present the case of a 65-year-old male patient, with a known history of a hepatic cholangiocarcinoma treated surgically. He has a past medical history of hypertension, cirrhosis, atrial flutter and pleural effusion. During a follow-up PET scan, a unique hypermetabolic C2 lesion was identified. The patient was neurologically intact, with mild neck pain. A cervical CT scan showed a solitary lytic lesion involving the C2 vertebral body, without fracture (Figure 1). After consultation with the multidisciplinary team and the patient, we opted for a treatment with a mini-invasive CT guided percutaneous biopsy and vertebroplasty. Since the patient had a single osteoarticular lesion, and the primary tumor was a cholangiocarcinoma, a tumor that is rarely responsible of spinal metastasis, a biopsy was essential to obtain histologic confirmation of the diagnosis. Vertebroplasty was done to control pain and prevent vertebral body collapse. “All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).” Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Intervention technique
The regional anatomy was revised days prior to the procedure, both with computed-tomography (CT-scan) and magnetic resonance imaging (MRI) to identify vascular structures and find a safe trajectory (Figure 2).
The patient was premedicated intravenously with 1 mg of midazolam and 75 μg of fentanyl and received 2 g of intravenous cefazolin 1 hour prior to the procedure.
With the patient in dorsal decubitus on the CT table, a first pass was obtained, without contrast, to identify the path of the needle and mark the skin.
The usual disinfection and sterile draping technique for vertebroplasty was performed.
Local anesthesia using approximately 10 mL of lidocaine 1% was delivered in the skin, soft tissues and to the periosteum of C2.
After a scalpel incision of less than a centimeter, a 11-G MadisonTM bone biopsy needle was introduced laterally, through the parotid and between the carotid artery and vertebral artery. The needle was advanced using CT guidance.
The entry point on C2 was right under the lateral mass of C1 and anterolaterally to the vertebral vascular foramen (Figure 3A).
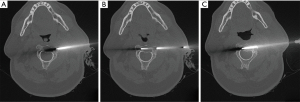
With the help of a hammer, the needle was advanced to the border of the lesion and three bone sampling were taken and sent to pathology for analysis (Figure 3B). The needle was then further advanced to the other side of the lesion in order to come in contact with normal bone (Figure 3C).
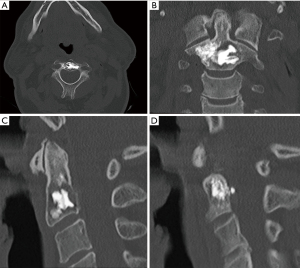
A PCD mixer and delivery system (Stryker Corp., USA) was used to deliver, under intermittent CT guidance, 3 mL of cement inside the bone lesion with extension to surrounding normal bone.
A small leakage was identified through the posterior cortex and cement injection was stopped immediately by inverting the rotation of the delivery system to release injection pressure.
The procedure was well tolerated by the patient. No neurological changes were noted per-operatively.
A last CT was obtained to assess the final result (Figure 4A-4D).
Patient was observed on a stretcher for 2 hours with nursing supervision before being discharged home.
At 1 month follow-up, the patient reported a very satisfactory pain control, with occasional neck pain (2/10 on the visual analog scale) treated with muscle relaxants, with no limitations in neck flexibility.
Discussion
Vertebroplasty is a well-established treatment option for spinal metastasis. It provides pain control in up to 80% of cases, prevents vertebral body collapse yielding spinal stability and improves patients’ quality of life while avoiding the more complex surgeries and their high rates of complications and preserving motion in the upper cervical spine (4,13,14). Contraindications for this technique include posterior wall defect (relative contraindication?), spinal cord compression and presence of neurological symptoms (8,11).
We previously published the largest prospective study in literature of patients with cervical spine metastasis treated with vertebroplasty. Forty-five percent of these patients presented with C2 osteolytic lesions. While 82% of patients reported excellent improvement, with 56% of reduction in opioid use, 18% developed major respiratory complications (pulmonary embolism and recurrent episodes of desaturation in a patient with known history of emphysema). The mean length of hospitalization in the complication-free cases was 3.9 days (8).
Percutaneous route is a less invasive alternative to approach the cervical spine. The first percutaneous vertebroplasty of C2 was described in 1984 for the treatment of an aggressive hemangioma (15). The most straightforward trajectory to access the C2 vertebra is the transoral approach. The main disadvantage of this technique is the relatively high risk of infection by the oropharyngeal flora (9,10). Mont’Alverne et al. (11) reported a series of 12 patients treated with percutaneous vertebroplasty for C2 metastatic lesions using an anterolateral approach. The procedures were performed under conscious sedation, with non-invasive sedation. The approach requires head extension to allow access to the space below the angle of the mandibula. The needle is then advanced through the parapharyngeal, retropharyngeal and prevertebral spaces to access the inferior lateral aspect of the C2 vertebral body. Pain improvement was noted in 80% of cases. Reported complications rate was 16.7%, with one case of transient occipital neuralgia secondary to cement leak to C1–C2 joint and another case of cerebellar and occipital infarction. The duration of hospital stay was not reported in this study.
Guo et al. reported a case series of 15 patients (including 9 cases of C2 lesions) treated with translateral percutaneous vertebroplasty for upper cervical spine lesions (hemangiomas and metastasis) after failure of conservative treatment (12). As in our case, pain was the main goal of treatment, with all patients presenting with no neurological deficit. The CT guided procedures were performed in the operating room, with patients in lateral decubitus position, with the neck slightly overextended. The space between the carotid sheath and vertebral artery was accessed percutaneously under local anesthesia. Excellent pain control was achieved in all patients, with no reported short- or long-term complications. Asymptomatic cement leakage was noted in 5 cases. The hospital stay duration was not reported in this study.
In our described approach, the patient was in dorsal decubitus position, with the neck in neutral position without the need of hyperextension to access the space between the carotid and vertebral artery. This can be particularly helpful in cases of upper cervical metastasis with important vertebral body collapse where neck extension is to be avoided.
One consideration with this technique, however, is the potential for a facial nerve injury, which cannot be identified on CT or MRI at this level (intraparotid). This should be disclosed to the patient as a potential complication. For the best of our knowledge, this is the first paper to describe a percutaneous upper cervical vertebroplasty performed as a day procedure. We found this to be safe considering the low complication rates reported in previous studies (2,6,11,12).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-21-97/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-21-97/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. “All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).” Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sciubba DM, Gokaslan ZL, Suk I, et al. Positive and negative prognostic variables for patients undergoing spine surgery for metastatic breast disease. Eur Spine J 2007;16:1659-67. [Crossref] [PubMed]
- Barragán-Campos HM, Vallée JN, Lo D, et al. Percutaneous vertebroplasty for spinal metastases: complications. Radiology 2006;238:354-62. [Crossref] [PubMed]
- Rodriguez-Catarino M, Blimark C, Willén J, et al. Percutaneous vertebroplasty at C2: case report of a patient with multiple myeloma and a literature review. Eur Spine J 2007;16:242-9. [Crossref] [PubMed]
- Sayama CM, Schmidt MH, Bisson EF. Cervical spine metastases: techniques for anterior reconstruction and stabilization. Neurosurg Rev 2012;35:463-74; discussion 475. [Crossref] [PubMed]
- Guglielmi G, Andreula C, Muto M, et al. Percutaneous vertebroplasty: indications, contraindications, technique, and complications. Acta Radiol 2005;46:256-68. [Crossref] [PubMed]
- Weill A, Chiras J, Simon JM, et al. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology 1996;199:241-7. [Crossref] [PubMed]
- Pilitsis JG, Rengachary SS. The role of vertebroplasty in metastatic spinal disease. Neurosurg Focus 2001;11:e9. [Crossref] [PubMed]
- Sebaaly A, Najjar A, Wang Z, et al. Anterolateral cervical kyphoplasty for metastatic cervical spine lesions. Asian Spine J 2018;12:823-9. [Crossref] [PubMed]
- Martin JB, Gailloud P, Dietrich PY, et al. Direct transoral approach to C2 for percutaneous vertebroplasty. Cardiovasc Intervent Radiol 2002;25:517-9. [Crossref] [PubMed]
- Gailloud P, Martin JB, Olivi A, et al. Transoral vertebroplasty for a fractured C2 aneurysmal bone cyst. J Vasc Interv Radiol 2002;13:340-1. [Crossref] [PubMed]
- Mont’Alverne F, Vallée JN, Cormier E, et al. Percutaneous vertebroplasty for metastatic involvement of the axis. AJNR Am J Neuroradiol 2005;26:1641-5. [PubMed]
- Guo WH, Meng MB, You X, et al. CT-guided percutaneous vertebroplasty of the upper cervical spine via a translateral approach. Pain Physician 2012;15:e733-41. [PubMed]
- Tian QH, Sun XQ, Lu YY, et al. Percutaneous vertebroplasty for palliative treatment of painful osteoblastic spinal metastases: a single-center experience. J Vasc Interv Radiol 2016;27:1420-4. [Crossref] [PubMed]
- Rhiew R, Manjila S, Dezure A, et al. Minimally invasive anterior vertebroplasty for C-2 metastatic lesions. Neurosurg Focus 2008;25:e4. [Crossref] [PubMed]
- Galibert P, Deramond H, Rosat P, et al. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987;33:166-8. [PubMed]



