
Don’t forget the pelvis: accounting for pelvic rotation in the preoperative assessment of adolescent idiopathic scoliosis
Introduction
Adolescent idiopathic scoliosis (AIS) causes three-dimensional (3D) deformity in the coronal, sagittal, and axial planes. Although cosmetic deformities are most noticeable in the thoracic region, causing shoulder imbalance and rib asymmetry, malalignment extends down to the pelvis. The altered pelvic position in AIS can be equally concerning to patients and also alters gait kinematics (1,2). In order to keep the trunk centered over the pelvis, the pelvis often rotates to the convex side of the major curve (1). Anatomic studies have confirmed unequal ilium widths between the convex and concave sides in untreated AIS patients, indicating significant pelvic rotation (3,4).
Despite the 3D abnormality of AIS, preoperative assessment is restricted to the two-dimensional (2D) plane. These 2D measurements form the basis of surgical decision making. However, it has been shown that the pelvic rotation in AIS may compromise a surgeon’s ability to obtain reliable radiographic assessments (5,6). Pelvic rotation can lead to patients being malpositioned in the X-ray scanner, thus shifting preoperative measurements (5,6). Prior studies have shown that these measurement errors may be more pronounced as curves become more severe (4,6). However, little is known about which measurements—sagittal, coronal, or rotational—are most affected and the magnitude of such error (5).
Given the 3D deformity seen in AIS, further study of how pelvic rotation impacts radiographic measurements is needed. In a group of Lenke Type 1/2 AIS patients, we conducted a pilot study to assess the study question of how pelvic rotation (i.e., the patient’s position in the X-ray scanner) affected the surgeon’s ability to record sagittal, coronal and rotational measurements. We hypothesized that the patient’s degree of pelvic rotation (i.e., the amount of rotation in the X-ray scanner), would significantly affect all radiographic measurements. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-675).
Methods
Study design and patient population
A retrospective, pilot, cross-sectional study of patients undergoing AIS surgery from 2017–2018 was undertaken. All patients carried a diagnosis of AIS, had a Type 1/2 curve, and had complete, full-length preoperative X-rays. Patients were excluded if they had Types 3-6 curves or did not have the requisite imaging. Though all patients underwent surgery, only preoperative imaging was used for the current study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional/regional/national ethics/committee/ethics board of Columbia University (No.: AAAQ18122) and individual consent for this retrospective analysis was waived.
Data collection
Basic demographic information was obtained for all patients from electronic medical records. Though only preoperative radiographic information was analyzed, the upper instrumented vertebrae (UIV), lower instrumented vertebrae (LIV), and levels fused were recorded to show that each patient had severe enough scoliosis to warrant surgical correction. All imaging was obtained with SterEOS technology (EOS imaging, Paris, France). From the low-dose, 2D, standing radiographs, surgeons and EOS technicians identified anatomical landmarks (both femoral heads and T1/L5 superior/inferior endplates) to render 3D images of the spine and pelvis (7,8). No custom code is required, and the only measuring required is to identify the aforementioned landmarks, and from these landmarks, all radiographic measurements can be obtained. The generated 3D image can then be adjusted for shape of the curve and width of the vertebral bodies. EOS generated 3D reconstructions have been shown to be accurate in comparison to the gold standard of computed tomography (CT) rendered 3D images (9,10).
Radiographic measurements
All patients underwent full-length imaging under the same protocol, being told to stand straight in the scanner as they would, in a normal, comfortable posture. Measurements were taken in one of two scenarios, both in the 3D plane: (I) the radio plane and (II) the patient plane. Measurements in the radio plane were obtained based on the patient’s natural position in the scanner, without accounting for any malposition or asymmetry Conversely, the patient plane was obtained after identifying key anatomical landmarks and rotating the patient from their original position in the scanner to a plane perpendicular to the transverse plane. The patient plane is the actual source of all radiographic information used for clinical care. In summary, evaluating the difference between these two planes allowed us to determine the impact of pelvic rotation on subsequent radiographic measurements (i.e., how much the patient’s position in the X-ray scanner altered measurements) (6).
In both planes, several radiographic measurements were collected. The pelvic orientation measurements were: pelvic obliquity (millimeters) and pelvis axial rotation. The sagittal plane measurements were: thoracic kyphosis (TK) and lumbar lordosis (LL). The coronal plane measurements were: coronal cobb angles of main thoracic (MT) and thoracolumbar/lumbar (TL/L) curves, and apical vertebral rotation (AVR) in the proximal thoracic (PT-AVR), main thoracic (MT-AVR), thoracolumbar/lumbar (TL/L-AVR) regions. Of note, two subsets of TK (T1-12/T4-12) and LL (L1-5, L1-S1) were assessed.
Due to the fact that a validated computer algorithm produced all measurements after identification of anatomical landmarks, and previous studies have shown excellent reliability and accuracy of 3D EOS measurements compared to both 2D and CT measurements (9,11-14), we did not feel an internal reliability or accuracy assessment was necessary.
Statistical analysis
Continuous data was presented as the mean ± standard deviation, and count data as n (%). Paired student’s t-tests were used to assess the differences in each radiographic outcome between the radiographic and patient plane. A Shapiro-wilk test was performed for the AVR, and given that P=0.372, the null hypothesis of a normally distributed sample was not rejected, and normality was assumed. Despite the small sample, given the normal distribution, t-tests were deemed appropriate. All statistical analyses were performed in STATA version 14 (StataCorp LP, College Station, Texas).
Results
Demographics
A total of 15 patients were included in the current pilot study with an average age of 15.7±1.2 years and 66.7% were female. The preoperative mean (standard deviation) pelvic obliquity was 4.0 mm (3.8) (Figure 1) and pelvic rotation was 5.1° (3.3) (Figure 2). Though no postoperative measurements were used for the current study, all patients had severe enough scoliosis that required surgical intervention with the most common UIV of T3 (60.0%), the most common LIV of L1 (53.3%), and mean levels fused was 10.5 (Table 1).
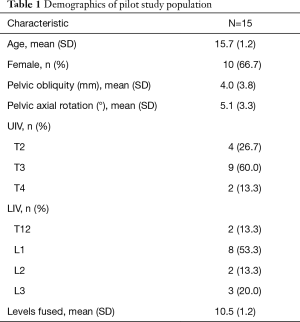
Full table
Radiographic outcomes (Table 2, Figures 1,2)
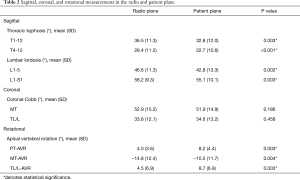
Full table
When comparing the radio and patient plane, significant differences were seen in sagittal and rotational measurements but not coronal measurements (Table 2). Both measures of TK (T1-12/T4-12) and LL (L1-5/L1-S1) values were significantly different between planes. TK differed in both subsets: T1-12: 36.5° vs. 32.8° (P=0.003); T4-12: 28.4° vs. 22.7° (P<0.001). Similarly, LL differed in both subsets: L1-5: 46.6° vs. 42.8°, (P=0.002); L1-S1: 58.2° vs. 55.1° (P=0.003). All three measurements of AVR differed significantly between planes: PT-AVR: 4.0° vs. 8.2°, (P=0.003); MT-AVR: −14.8° vs. −10.5°, (P=0.004); TL/L-AVR: 4.5° vs. 8.7°, (P=0.003). No significant differences were seen in either of the coronal cobb angles. Absolute values of TK/LL in the radio and patient plane are seen (Figures 3,4), whereas change values (difference between radio and patient plane) are seen for three rotational measures of PT-AVR, MT-AVR, TL/L-AVR (Figure 5).
Discussion
Despite AIS deformity occurring in three planes, the preoperative and postoperative assessment of AIS remains rooted in 2D. To maintain accurate and valid measurements, it is imperative that 2D assessments account for the unique 3D characteristics each AIS patient. The current analysis revealed that an average of 5.1° of pelvic rotation occurred in each AIS patient before correction to the patient plane. Sagittal and rotational parameters of TK, LL, and AVR were significantly altered due to the pelvic rotation (i.e., the patient’s position in the X-ray scanner), whereas coronal measurements were not significantly impacted. These results have implications for obtaining accurate measurements in the treatment of AIS, surgical decision-making, postoperative monitoring, and surgeon-to-surgeon communication.
Pelvic rotation is routinely encountered in AIS. Gum et al. (15) studied 239 AIS Type 1-6 patients and found that the ratio of left to right iliac widths was 0.95, meaning that pelvic rotation was present (ratio≠1 indicated asymmetry). The authors postulated that pelvic rotation was compensatory, but regardless of the true etiology, clinically significant pelvic rotation occurred in their large AIS cohort. Additional anatomic studies have confirmed asymmetric ilia width in 42 female AIS patients (3). Pelvic rotation also manifests as abnormal gait in AIS patients (2). Nishida and colleagues (1) studied gait kinematics in 18 AIS patients and found that preoperative pelvic orientation deviated 4.0° to the convex side and trunk rotation was negatively correlated with pelvic rotation (R=−0.64, P≤0.01), indicating the pelvis rotated to the opposite side of the major curve in order for the spine to maintain balanced over the pelvis. All pelvic rotation abnormalities improved significantly after surgery, further highlighting the importance of noticing this abnormality in the preoperative setting (1).
Our results show that sagittal and rotational radiographic measurements were significantly altered when pelvic rotation is corrected for. Pasha and colleagues (5) similarly found altered sagittal measurements in 36 AIS patients, where the radio vs. patient plane measurements for TK were 35.9° and 33.6°, respectively, and LL was 59.5° and 57.5°, respectively, which are almost identical to our results (5). Additionally, correcting for the patient’s alignment in the X-ray scanner improved correlation between 2D and 3D measurements (5). Also similar to the current findings, coronal measurement were not affected. Several authors have also shown that the impact of pelvic rotation on sagittal measurements is more pronounced in more severe curves. A second study by Pasha et al. (6) showed that in 73 AIS patients, the amount of pelvic rotation present was stronger when TK was greater than 40° and LL was greater than 60°. Stylianides and colleagues (4) compared controls, moderate AIS patients, and severe AIS patients and found that iliac spine geometry was significantly altered in the severe AIS group compared to the control and moderate AIS groups. The authors hypothesized that asymmetrical bone growth may have contributed to the pelvic rotation seen in AIS (4). Our study offers additional insight that rotational assessments are also impacted by pelvic rotation. Pelvic rotation not only impacted AVR in the principle, and instrumented MT curve, but also the less pronounced and uninstrumented PT and TL/L curves. These results and prior studies reinforce the same conclusions—pelvic rotation has implications for both the sagittal and rotational measurements (5).
Future studies can use the results of our pilot analysis to correlate both the 3D radio and patient plane measurements to more traditional 2D assessments. Knowing how more accurate 3D images compares to 2D assessment can aid surgeons in surgical planning and postoperative monitoring. Moreover, additional analyses should be considered in other scoliosis settings such as Type 3-6 AIS curves, early onset scoliosis, neuromuscular scoliosis, and adult degenerative scoliosis, each of which may have more clinically significant pelvic rotation. It is also unclear how pelvic rotation affects pelvic parameters such as pelvic tilt, sacral slope, and sagittal vertical axis, though more relevant to an adult scoliosis population. As 3D software continues to be utilized, and may eventually become standard of care, comparison of the radio and patient plane is important to ensure uniformity and accuracy when treating patients and communicating amongst surgeons. Though the current study did not include postoperative information, all patients underwent surgical correction. One important factor to consider when pelvic obliquity is present, in either a rigid or flexible spine, is the presence of leg-length discrepancy. Though more common in older populations, shoe lifts can be recommended to improve ambulation and reduce disability in any patient with scoliosis. Moreover, the presence a fixed pelvic obliquity must be taken note of intraoperatively after any deformity correction to ensure the spine is straight against a neutral pelvis, or else coronal malalignment may occur. For centers without EOS technology, these results can be used to educate X-ray technicians and patients to be sure the patient gives as best effort as possible to stand straight and orthogonal in the X-ray scanner. Perhaps specific lines and techniques can be used to ensure consistency and repeat X-rays in the orthogonal plane for all patients.
Though this was intended to be a pilot study, a limitation is the small sample size of 15 patients. Similar imaging studies have used small sample sizes (5), the results of this preliminary analysis are exploratory in nature and should be interpreted with caution. Second, all radiographic measurements were generated by EOS imaging software and not measured by individual surgeons. Moreover, no internal reliability or validity assessment was performed. One prior study correlated radiographic measurements between 2D and EOS generated 3D images and found excellent correlation between coronal measurements (r=0.950) and thoracic kyphosis (r=0.893) (9). A similar study found substantial interobserver and excellent intraobserver agreement on multiple radiographic measurements with 3D EOS imaging, with less than 4° difference found between two raters on AVR (11). In a study of severe AIS curves >50°, a third study reported intraclass correlation (ICC) values among 3 raters of 0.97 using 3D AIS images. Based on the prior literature supporting the reliability and accuracy of 3D EOS imaging, no internal reliability or accuracy assessments were performed. That said, multiple prior studies have shown that 3D images produced excellent reliability and accuracy compared to 2D and CT measurements (9,11-14). Third, though our results yielded statistical significance in the sagittal and rotational planes, it is unknown if this translates to clinical significance. The expected measurement error in sagittal and coronal 2D radiographic measurements has been estimated to be 1.8°–3.0° (16,17), compared to our approximate differences 3°–6°. Thus, we caution against overextrapolation of our findings. Nonetheless, our average preoperative Cobb angle was 51.9°±14.9°, and these variations may become more pronounced with more severe curves, as prior studies have suggested (4,6).
Overall, in light of the small sample and previous studies showing the importance of pelvic rotation, it is our hope these results can add to the growing evidence that the patient’s position in the scanner must be taken into account when using EOS images. If spinal alignment is examined in absence of accounting for pelvic rotation, operative plans may be designed incorrectly, with potentially postoperative coronal or sagittal malalignment requiring revision surgery. Given the potential iatrogenic complications of not accounting for a patient’s rotated pelvis, we believe these results can be of use to all practicing spinal deformity surgeons.
Conclusions
An average of 5.1° of pelvic rotation occurred in each AIS patient prior to correction to the perpendicular, patient plane. Pelvic rotation (i.e., the patient’s position in the X-ray scanner) impacted sagittal and rotational measurements, whereas coronal measurements were not affected. These results have implications for measurement accuracy, surgical decision-making and postoperative monitoring.
Acknowledgements
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-675
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-675
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-675
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-675). SLZ serves as an unpaid editorial board member of Journal of Spine Surgery from Oct 2019 to Sep 2021. LGL serves as an unpaid editorial board member of Journal of Spine Surgery from Oct 2019 to Oct 2021. LGL reports personal fees from Medtronic, grants and personal fees from DePuy-Synthes Spine, personal fees from K2M, non-financial support from Broadwater, non-financial support from Seattle Science Foundation, grants and non-financial support from Scoliosis Research Society, non-financial support from Stryker Spine, non-financial support from The Spinal Research Foundation, grants from EOS, grants from Setting Scoliosis Straight Foundation, personal fees from Fox Rothschild, LLC, personal fees from Quality Medical Publishing, other from Evans Family Donation, other from Fox Family Foundation, grants and non-financial support from AOSpine, outside the submitted work; LGL reports personal fees from Medtronic, grants and personal fees from DePuy-Synthes Spine, personal fees from K2M, non-financial support from Broadwater, non-financial support from Seattle Science Foundation, grants and non-financial support from Scoliosis Research Society, non-financial support from Stryker Spine, non-financial support from The Spinal Research Foundation, grants from EOS, grants from Setting Scoliosis Straight Foundation, personal fees from Fox Rothschild, LLC, personal fees from Quality Medical Publishing, other from Evans Family Donation, other from Fox Family Foundation, grants and non-financial support from AOSpine, outside the submitted work. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional/regional/national ethics/committee/ethics board of Columbia University (No.: AAAQ8122) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nishida M, Nagura T, Fujita N, et al. Spinal correction surgery improves asymmetrical trunk kinematics during gait in adolescent idiopathic scoliosis with thoracic major curve. Eur Spine J 2019;28:619-26. [Crossref] [PubMed]
- Patel A, Pivec R, Shah NV, et al. Motion analysis in the axial plane after realignment surgery for adolescent idiopathic scoliosis. Gait Posture 2018;66:181-8. [Crossref] [PubMed]
- Qiu XS, Zhang JJ, Yang SW, et al. Anatomical study of the pelvis in patients with adolescent idiopathic scoliosis. J Anat 2012;220:173-8. [Crossref] [PubMed]
- Stylianides GA, Beaulieu M, Dalleau G, et al. Iliac crest orientation and geometry in able-bodied and non-treated adolescent idiopathic scoliosis girls with moderate and severe spinal deformity. Eur Spine J 2012;21:725-32. [Crossref] [PubMed]
- Pasha S, Cahill PJ, Dormans JP, et al. Characterizing the differences between the 2D and 3D measurements of spine in adolescent idiopathic scoliosis. Eur Spine J 2016;25:3137-45. [Crossref] [PubMed]
- Pasha S, Ecker M, Deeney V. Considerations in sagittal evaluation of the scoliotic spine. Eur J Orthop Surg Traumatol 2018;28:1039-45. [Crossref] [PubMed]
- Humbert L, De Guise JA, Aubert B, et al. 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 2009;31:681-7. [Crossref] [PubMed]
- Gille O, Champain N, Benchikh-El-Fegoun A, et al. Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine (Phila Pa 1976) 2007;32:568-73. [Crossref] [PubMed]
- Al-Aubaidi Z, Lebel D, Oudjhane K, et al. Three-dimensional imaging of the spine using the EOS system: is it reliable? A comparative study using computed tomography imaging. J Pediatr Orthop B 2013;22:409-12. [Crossref] [PubMed]
- Glaser DA, Doan J, Newton PO. Comparison of 3-dimensional spinal reconstruction accuracy: biplanar radiographs with EOS versus computed tomography. Spine (Phila Pa 1976) 2012;37:1391-7. [Crossref] [PubMed]
- Bagheri A, Liu XC, Tassone C, et al. Reliability of Three-Dimensional Spinal Modeling of Patients With Idiopathic Scoliosis Using EOS System. Spine Deform 2018;6:207-12. [Crossref] [PubMed]
- Carreau JH, Bastrom T, Petcharaporn M, et al. Computer-Generated, Three-Dimensional Spine Model From Biplanar Radiographs: A Validity Study in Idiopathic Scoliosis Curves Greater Than 50 Degrees. Spine Deform 2014;2:81-8. [Crossref] [PubMed]
- Illes T, Somoskeoy S. Comparison of scoliosis measurements based on three-dimensional vertebra vectors and conventional two-dimensional measurements: advantages in evaluation of prognosis and surgical results. Eur Spine J 2013;22:1255-63. [Crossref] [PubMed]
- Rehm J, Germann T, Akbar M, et al. 3D-modeling of the spine using EOS imaging system: Inter-reader reproducibility and reliability. PLoS One 2017;12:e0171258 [Crossref] [PubMed]
- Gum JL, Asher MA, Burton DC, et al. Transverse plane pelvic rotation in adolescent idiopathic scoliosis: primary or compensatory? Eur Spine J 2007;16:1579-86. [Crossref] [PubMed]
- Wang J, Zhang J, Xu R, et al. Measurement of scoliosis Cobb angle by end vertebra tilt angle method. J Orthop Surg Res 2018;13:223. [Crossref] [PubMed]
- Ylikoski M, Tallroth K. Measurement variations in scoliotic angle, vertebral rotation, vertebral body height, and intervertebral disc space height. J Spinal Disord 1990;3:387-91. [PubMed]







