
One surgeon’s learning curve with single position lateral lumbar interbody fusion: perioperative outcomes and complications
Introduction
Lateral transpsoas lumbar interbody fusion (LLIF) is a minimally invasive procedure that has proven to be an effective treatment for a variety of spine pathologies (1-3). Compared to other approaches, LLIF offers the advantage of avoiding manipulation of the great vessels and posterior neural structures, spares significant dissection of paraspinal musculature, and allows for placement of a larger interbody device and bone graft (4).
LLIF typically involves lateral decubitus positioning for interbody placement followed by prone positioning for percutaneous pedicle screw fixation (PPSF). Recently, lateral-only positioning LLIF with PPSF has been described and popularized in both primary and revision fusion settings (5,6). All-lateral positioning decreases surgical time and avoids the risks associated with prolonged prone surgery without negatively impacting complication rate, patient outcomes, or post-operative lordosis (7-10).
Single position (SP) LLIF with PPSF is an attractive option given the potential time and cost savings. However, the learning curve has not yet been described and would be beneficial to surgeons considering implementing the technique. Therefore, the purpose of this study was to describe the operative time and outcomes as a function of case number for a single surgeon adopting SP LLIF.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jss-21-13).
Methods
This was a retrospective case series conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of Stanford University (protocol #7935) and individual consent for this retrospective analysis was waived. All patients undergoing LLIF with the senior author from January 2013 through October 2019 were identified using an institutional chart extraction tool. Prior to starting SP LLIF, the senior author had five years of dual positioning (DP) LLIF experience and did not participate in any formal SP LLIF technique course.
Patient population and data collection
Patients over 18 years of age who underwent SP LLIF with PPSF were included. Involvement of a co-surgeon resulted in exclusion. Revision cases, multilevel LLIF procedures, or adjacent non-LLIF procedures did not exclude the patient, but these factors were noted. All indications for surgery were included. This review identified the senior author’s first 161 patients undergoing the procedure for inclusion. The primary outcome was operative time, measured from the time of incision to skin closure. Secondary outcomes included intraoperative fluid administration; estimated blood loss; length of hospital stay; fusion at 1 year; and preoperative to postoperative change in hematocrit, LL, and Oswestry Disability Index (ODI). Postoperative ODI was measured 6 weeks after surgery. Long-term ODI scores were missing for most patients and thus were not analyzed. We also collected baseline patient characteristics including age, body mass index (BMI), sex, smoking status, American Society of Anesthesiologists (ASA) classification, Charlson Comorbidity Index (CCI), whether the patient had a prior lumbar fusion, and preoperative diagnosis. Surgical details collected included LLIF levels, adjacent procedures, and whether a 22 modifier was used. Pedicle screw placement at L4 and above was evaluated by the method of Kim et al. (11). Given that the Kim method is not validated at L5 and may overestimate lateral breech, screw placement at L5 was deemed laterally out if the screw tip did not cross the lateral border of the pedicle. Medical and surgical complications within 90 days of surgery were also evaluated. Surgical complications were defined as iatrogenic fracture, reoperation, and new lower extremity radiculopathy or weakness. Transient hip flexor weakness or thigh paresthesias were not counted as complications given they are expected side effects of the transpsoas approach (12). Moreover, suboptimally placed pedicle screws were not defined as a complication unless symptomatic. Instead, screw position was analyzed separately from complications.
Surgical technique
Patients were placed in the lateral decubitus position for the lateral approach, discectomy, endplate preparation, interbody placement, and fluoroscopically guided PPSF. A minimal table break was utilized for the LLIF portion to allow for better clearance of the iliac crest. Significant table angulation was avoided to prevent overtensioning of the femoral nerve. The table was returned flat for placement of the PPSF.
Statistical methods
Preliminary data visualization was performed by plotting operative time and other outcomes versus case number and stratifying by number of levels, whether adjacent procedures were performed, and whether Modifier 22 was noted on the case. To obtain the most homogenous cohort, the primary analysis focused on single level cases with no adjacent level procedures. Secondary analyses included 1−3 level cases with no adjacent level procedures. Cases with more levels and cases with adjacent level procedures were included in the case count but were not included in the analyses. For the secondary analysis, operative time for 2 and 3 level cases was normalized to that of single level cases in the manner of Lee et al. (13). Descriptive statistics are presented as frequencies and percentages for categorical variables. Continuous variables are presented as means and 95% confidence intervals (CI) if normally distributed and medians and interquartile ranges (IQR) if non-normally distributed. All available data were analyzed.
The learning curve was assessed with both linear and logarithmic regression. R2 values and data visualization were used to select the most appropriate model to fit the data. Other continuous outcomes were assessed similarly. Mann Whitney U tests were used to determine whether complications occurred more frequently in earlier versus later cases. All analyses were performed with SAS version 9.4 (Cary, NC, USA) with a two-sided level of significance of α=0.05.
Results
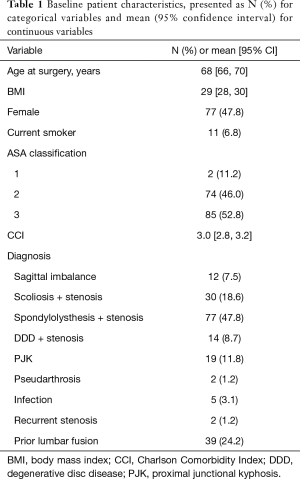
The cohort included 161 patients; 77 (48%) were female, and the average age was 68 years (95% CI, 66–70 years) (Table 1). The average body mass index (BMI) was 29 (95% CI, 28–30), 11 (7%) patients were active smokers at the time of surgery, and the average Charlson comorbidity index (CCI) was 3 (95% CI, 2.8–3.2). The most common operative indication was spondylolisthesis (48%).
Full table
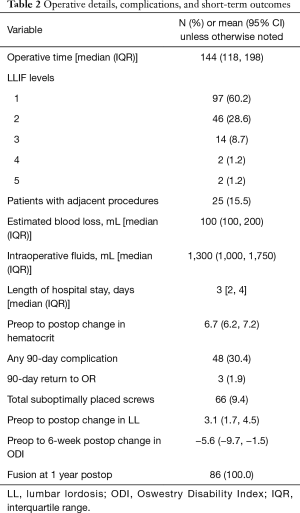
Most patients (60%) underwent single level LLIF. Representative pre- and postoperative images are shown in Figure 1. Average operative time was 144 minutes (IQR, 118–198 minutes) (Table 2). There were 18 patients (11.1%) with 90-day medical complications, including 4 patients with post-operative ileus, 4 patients with urinary tract infection, 9 patients with urinary retention, and 1 patient each with acute liver injury, pneumonia, acute kidney injury, myocardial infarction, hyperglycemia requiring emergency department care, atrial fibrillation with rapid ventricular response, persistent orthostatic hypotension, pneumothorax, and fluid overload. Five patients (3%) had 90-day surgical complications including 1 patient each of iatrogenic vertebral body fracture, transient tibialis anterior weakness, femoral nerve palsy improving 2 months after surgery, symptomatic prominent screw that had pulled out requiring removal, and radiculopathy due to a suboptimally placed screw requiring revision with subsequent symptom resolution. Sixty-six (9.4%) screws were deemed to be out of the pedicle based on X-rays in a total of 55 (34.4%) patients. Fifty-seven screws were out laterally, 3 were out medially, 5 were out anteriorly, and 1 was out inferiorly. Thirty-nine (59.1%) suboptimally placed screws were on the downside while 27 (40.9%) were on the upside. Only two screws required reoperation as described above. All patients with 1-year follow-up available had successful fusion (n=86).

Full table
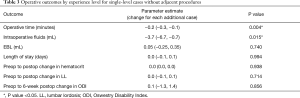
Preliminary data visualization demonstrated that the number of levels and whether or not adjacent level procedures were performed influenced outcomes, whereas Modifier 22 did not. Thus, subsequent analyses were performed by level, and cases with adjacent level procedures were included in the case count but not in the analyses. For single level surgeries without adjacent procedures (n=87), operative time decreased 0.2 (95% CI, 0.1–0.3) minutes for each consecutive case (P<0.001), for a total decrease of 28.7 (95% CI, 9.6–47.9) minutes over the 161 cases examined (Figure 2). For 1-3 level cases with no adjacent procedures (n=131), normalized operative time decreased by 23.1 (95% CI, 7.6–38.6) minutes (P<0.001, Figure 3). These relationships gave no evidence of non-linearity and the simple linear regression was a best fit to the data based on the R2 values. For single level surgeries without adjacent procedures, there were no significant changes in estimated blood loss, postoperative change in hematocrit, length of hospital stays, postoperative change in lordosis, and the 6-week pre- to post-operative change in the ODI (available in a subset of n=30 patients) as case number increased (Table 3). Intraoperative fluids decreased 3.7 mL (95% CI, 0.7–6.7) per case.
Full table
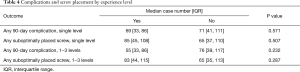
Cases with 90-day complications and cases with suboptimally placed screws did not occur earlier in the learning curve than those without these issues (Table 4). This finding was true for single level surgeries without adjacent procedures (P=0.311 and 0.507, respectively) and for 1−3 level cases without adjacent procedures (P=0.142 and 0.217, respectively).
Full table
Discussion
SP LLIF has been shown to reduce operative time by 45 minutes compared to dual positioning, without compromising outcomes (10). Increased operative time is an independent risk factor for medical and surgical complications (14) and has greater cost (15), which makes SP LLIF an attractive option in an increasingly value-based healthcare setting. However, minimally invasive fusion techniques are technically challenging and surgeons may experience increased operative time and complications early in the learning curve (16).
In this study, we describe the learning curve of one surgeon adopting the SP LLIF technique. Operative time for single-level fusions decreased by an average of 12 seconds per case for total decrease of nearly 30 minutes over the course of 161 cases. Similarly, intraoperative fluids decreased by an average of 3.7 mL per case, which is intuitive given as case time shortens, time for fluid delivery decreases. There was no evidence that short-term outcomes or complications were any more common earlier in the learning curve.
Several studies have described the learning curve of other minimally invasive surgical (MIS) techniques for lumbar fusion. Lee et al. reported on the learning curve of a single surgeon performing MIS transforaminal interbody fusion (13). Operative time initially decreased and then stabilized after approximately 30 cases. Comparing the first 30 cases to the subsequent 56 cases, the early group had increased intraoperative blood loss, but there were no differences in complications between groups. Ng et al. reported on 32 consecutive patients who underwent LLIF of 47 levels showing that operative time for the interbody graft insertion stabilized after 22 operative levels (17). There were no differences in complication rates between early and late groups. A systematic review of minimally invasive spine surgery learning curves further supports that operative times tend to stabilize after 20 to 30 cases (16). Blizzard and Thomas reported on the first 72 patients undergoing SP LLIF or oblique lateral interbody fusion (OLIF) and PPSF with a single surgeon and state that there was no significant learning curve, but did not give specific data. They suggest that lack of a typical learning curve was due to the surgeon’s prior experience with DP LLIF that translates more easily to SP. We did not observe a typical logarithmic learning curve. Instead, our operative time decreased gradually and linearly with time over the series. Similarly to Blizzard and Thomas, the operating surgeon in our cohort had extensive prior experience with DP LLIF, likely contributing to this finding. Surgeons without prior experience with DP LLIF may experience a more typical learning curve.
Complication rates observed in our cohort are similar to historical reports. A systematic review by Hijji et al. of LLIF-related complications including 6,819 patients revealed average risk of cardiac, pulmonary, urinary (GU), and gastrointestinal (GI) complication to be 1.86%, 1.47%, 0.93%, and 1.38%, respectively (12). Our rates of cardiac, pulmonary, and GI complication were similar at 1.86%, 1.86%, and 3.1%, respectively. Our GU complication rate was slightly higher at 6.2% driven mostly by cases of transient urinary retention. Our rate of vertebral body fracture was similar at less than 1% and our reoperation rate was lower at 1.24% compared to their reported 3.9%.
Repositioning prone does not contribute significantly to correction of lumbar lordosis (LL) (7,10). In our cohort, LL increased by an average of 3.1° postoperatively, which is consistent with previous reports (7,18). Experience level did not influence LL correction. Since most LL correction comes from interbody cage and graft insertion, it is not surprising that surgeons switching from DP to SP LLIF would not experience early compromise in LL correction. Emphasis has also been placed on the ability to accurately place pedicle screws in the lateral position, especially on the downside given the more challenging angle. Breach rate as evaluated by computed tomography (CT) in the SP LLIF series by Blizzard and Thomas was 5.1%. We observed a breech rate of 9.4% — within the range of 3.2% to 14.3% reported previously for PPSF (5). Additionally, only two screws in our series required revision highlighting that suboptimal screw placement was rarely clinically significant. Experience level did not appear to affect screw accuracy. This finding may be due to the fact that the general radiographic technique for screw placement is the same whether in the lateral or prone position, so extensive prior experience with PPSF in DP LLIF likely translates well to SP LLIF.
Limitations of our study include that cases were from a single surgeon at a single academic institution and as such may not be generalizable. The surgeon also had prior experience with DP LLIF, so our results are likely not applicable to surgeons adopting SP LLIF without prior LLIF experience. Additionally, postoperative CT scans were not available in the majority of our patients, requiring use of plain radiographs to evaluate pedicle screw placement. While CT is the gold standard, the method of Kim et al. has an accuracy of 0.98 and is more likely to overestimate breach rate, which supports the validity of our results (11).
In sum, case number correlated with decreased operative time in SP LLIF with PPSF. The linear rather than logarithmic nature of this relationship is likely due to the surgeon’s extensive prior experience with dual position LLIF. Surgeons making a similar transition will likely experience a similar learning curve, whereas surgeons adopting SP LLIF with minimal prior LLIF experience may experience a steeper curve.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jss-21-13
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-21-13
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-21-13). IC reports personal royalty fees from NuVasive, Globus Medical, Spine Wave, and SpineCraft; personal consulting fees from NuVasive and Symgery; and personal stock ownership of Cytonics, SpinalCyte, Notogen, and Spine Innovations. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board of Stanford University (protocol #7935) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43. [Crossref] [PubMed]
- Sharma AK, Kepler CK, Girardi FP, et al. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech 2011;24:242-50. [Crossref] [PubMed]
- Phillips FM, Isaacs RE, Rodgers WB, et al. Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up. Spine (Phila Pa 1976) 2013;38:1853-61. [Crossref] [PubMed]
- Kwon B, Kim DH. Lateral Lumbar Interbody Fusion: Indications, Outcomes, and Complications. J Am Acad Orthop Surg 2016;24:96-105. [Crossref] [PubMed]
- Blizzard DJ, Thomas JA. MIS Single-position Lateral and Oblique Lateral Lumbar Interbody Fusion and Bilateral Pedicle Screw Fixation: Feasibility and Perioperative Results. Spine (Phila Pa 1976) 2018;43:440-6. [Crossref] [PubMed]
- Ziino C, Arzeno A, Cheng I. Analysis of single-position for revision surgery using lateral interbody fusion and pedicle screw fixation: feasibility and perioperative results. J Spine Surg 2019;5:201-6. [Crossref] [PubMed]
- Yson SC, Sembrano JN, Santos ER, et al. Does prone repositioning before posterior fixation produce greater lordosis in lateral lumbar interbody fusion (LLIF)? J Spinal Disord Tech 2014;27:364-9. [Crossref] [PubMed]
- Drazin D, Kim TT, Johnson JP. Simultaneous Lateral Interbody Fusion and Posterior Percutaneous Instrumentation: Early Experience and Technical Considerations. Biomed Res Int 2015;2015:458284 [Crossref] [PubMed]
- Kwee MM, Ho YH, Rozen WM. The prone position during surgery and its complications: a systematic review and evidence-based guidelines. Int Surg 2015;100:292-303. [Crossref] [PubMed]
- Ziino C, Konopka JA, Ajiboye RM, et al. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg 2018;4:717-24. [Crossref] [PubMed]
- Kim YJ, Lenke LG, Cheh G, et al. Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine (Phila Pa 1976) 2005;30:2084-8. [Crossref] [PubMed]
- Hijji FY, Narain AS, Bohl DD, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J 2017;17:1412-9. [Crossref] [PubMed]
- Lee JC, Jang HD, Shin BJ. Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: our experience in 86 consecutive cases. Spine (Phila Pa 1976) 2012;37:1548-57. [Crossref] [PubMed]
- Kim BD, Hsu WK, De Oliveira GS Jr, et al. Operative duration as an independent risk factor for postoperative complications in single-level lumbar fusion: an analysis of 4588 surgical cases. Spine (Phila Pa 1976) 2014;39:510-20. [Crossref] [PubMed]
- Childers CP, Maggard-Gibbons M. Understanding Costs of Care in the Operating Room. JAMA Surg 2018;153:e176233 [Crossref] [PubMed]
- Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res 2014;472:1711-7. [Crossref] [PubMed]
- Ng CL, Pang BC, Medina PJ, et al. The learning curve of lateral access lumbar interbody fusion in an Asian population: a prospective study. Eur Spine J 2015;24:361-8. [Crossref] [PubMed]
- Saadeh YS, Joseph JR, Smith BW, et al. Comparison of Segmental Lordosis and Global Spinopelvic Alignment After Single-Level Lateral Lumbar Interbody Fusion or Transforaminal Lumbar Interbody Fusion. World Neurosurg 2019;126:e1374-8. [Crossref] [PubMed]




