A novel anterior decompression technique for kyphosis line (K-line) ossification of posterior longitudinal ligament (OPLL): vertebral body sliding osteotomy
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is one of the major disorders of cervical compressive myelopathy (1-3). Surgical treatment would be considered for patients with moderate or severe myelopathic symptoms and significant cord compression on magnetic resonance images. Surgical options include anterior decompression such as corpectomy and fusion and posterior decompression including laminoplasty or laminectomy/fusion (1,2,4).
Anterior cervical corpectomy and fusion (ACCF) leads to better neurological outcomes than posterior decompression surgery for patients with more significant canal compromise (canal occupying ratio ≥60%) or reduced cervical lordosis in terms of the direct resection of the OPLL masses (5-9).
Lateral radiograph images are used to assess the relationship of the OPLL to the kyphosis line (K-line), which is defined as a line that connects the midpoints of the spinal canal at C2 and C7. The K-line assesses the size of OPLL mass and cervical sagittal alignment together. A large OPLL mass or loss of cervical lordosis causes the OPLL to exceed the K-line (referred to as K-line negative) and is a predictive factor for worse outcomes from laminoplasty (10,11).
Some surgeons prefer anterior decompression over posterior decompression to achieve a better neurologic outcome, if the OPLL mass is huge (involving 50–60% of the spinal canal), if global cervical kyphosis is >10 degrees, or if K-line is negative. However, ACCF surgery is technically demanding and may cause unexpected surgery-related complications, including cerebrospinal fluid (CSF) leakage, graft dislodgement, and pseudarthrosis (6,8,12,13). In addition, risk of dural tearing during ACCF increases in cases when the OPLL mass has penetrated the dura mater or if dural ossification has occurred. A “double-layer sign” is more predictive of dural ossification, whereas a diffuse dural defect is useful for indicating CSF leakage (4,14,15).
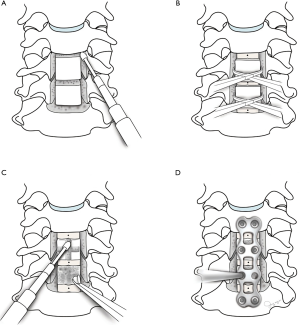
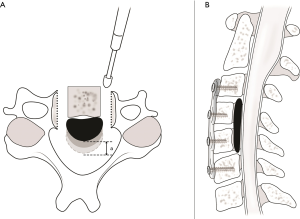
To reduce these complications and to achieve adequate decompression for the patients with severely protruding OPLL mass that is adhered to the posterior longitudinal ligament (PLL), we introduce a new anterior cervical decompression method, vertebral body sliding osteotomy (VBSO) (16). Its basic principle is to expand the spinal canal by anteriorly translating the involved vertebral bodies with any ossified masses (Figure 1). Here, we describe the VBSO technique and evaluate the long-term surgical outcomes of patients who underwent this procedure to correct severe OPLL.
Methods
The present study was a case series with minimum 2-year follow-up to assess the novel anterior decompression technique (VBSO) for cervical myelopathy due to OPLL. Twenty-four patients (16 men, 8 women) with cervical myelopathy caused by OPLL who underwent VBSO surgery between February 2012 and November 2015 at Asan Medical Center (Seoul, Korea) were included. Indication for surgery included myelopathy with more than moderate gait impairment of Nurick grade >3 and an OPLL mass-caused prominent cord compression (1,2). K-line negative patients who have a large OPLL mass or kyphotic cervical alignment were selected. Patients who had undergone any previous cervical spine surgery, OPLL lesions above the C2 level, or extremely lateral-deviated OPLL lesions were excluded.
Data on the operating time, the number of levels of surgery, estimated blood loss, and perioperative complications were collected from medical records. Preoperative and postoperative neurologic status was evaluated according to the Japanese Orthopaedic Association score for cervical myelopathy (C-JOA score), and the surgical outcomes were calculated using Hirabayashi method.
Recovery rate = (postoperative JOA score − preoperative JOA score)/(17− preoperative JOA score) ×100
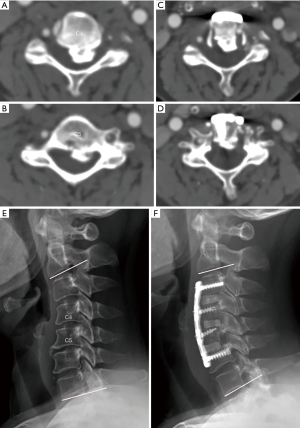
Various radiographic parameters such as the preoperative canal occupying ratio, postoperative canal widening, and preoperative and postoperative cervical lordosis angle were measured. The anteroposterior diameter of the spinal canal was measured at the level of the most prominent OPLL mass identified through axial computed tomography (CT) to measure the preoperative canal occupying ratio. The distance of anterior sliding was defined as the difference between the anteroposterior canal diameter of the preoperative and postoperative axial CT images at the same level (Figure 1). Postoperative flexion-extension radiographs were evaluated at 3, 6, and 12 months to assess the fusion status. For diagnosing pseudarthrosis, we first used the dynamic lateral flexion-extension cervical spine films under 1.5× magnification. Interspinous motion <1 mm and superjacent interspinous motion ≥4 mm in the dynamic films indicated solid fusion. In ambiguous cases, we confirmed fusion status by the reconstructed multiaxial CT scans to evaluate the extra-graft bridging bone between adjacent vertebral bodies (17,18). Cervical sagittal alignment was assessed through measurement of the angle of the inferior margin of the C2 and C7 preoperatively and postoperatively.
All analyses were performed using SPSS version 21.0 (IBM Corp., Armonk, NY, USA). Preoperative and follow-up data were compared using the Wilcoxon signed-rank test for continuous variables and discrete variables. A P value of <0.05 was considered significant. We obtained the appropriate approvals from our institutional ethical committee.
VBSO surgical procedure (Figure 2)
Multilevel discectomy and uncinate process resection
The cervical spine is approached via a standard anterior transverse or oblique incision. Initially, a multilevel discectomy is performed at the superior and inferior levels of all involved vertebral bodies. The involved levels are defined as the one-disc space cranial and one-disc caudal to the OPLL mass. After complete discectomy, resection of the uncinate processes is performed. Removing the uncinate process makes the width of mobile fragment of vertebral bodies wider and decompresses the foramina.
Resect PLL at most cranial and caudal disc level
PLLs that limit anterior translation of vertebral bodies are meticulously released at disc level above and below the involved vertebral body using a microdissector and Kerrison punch. However, the PLLs between the involve level which will be translated do not need to be released.
Mobilizing vertebral body fragments
The vertebral body is then detached from its side walls, and then a 2−3-mm high-speed burr is used to make two parallel longitudinal slits along the bilateral borders of the uncinate processes (Figure 2A). Subsequently, the posterior wall of the vertebral body is deepened to make the vertebral body a mobile segment. After the posterior cortical bone of the vertebral body is exposed, it is carefully cut by gentle burr tip control. Cutting by Kerrison punch is not recommended as it frequently results in bleeding. The Caspar pins should be placed into the vertebral bodies above and below the desired level with distraction at the time of mobilizing vertebral body fragments.
Anterior sliding of vertebral bodies
For widening of spinal canal, manual anterior migration of each mobile fragment of the vertebral bodies is performed using several Allis forceps (Figure 2B). Through preoperative measuring of the anteroposterior diameter of the OPLL on CT images, the extent of anterior sliding that is needed is estimated in advance. After pulling out the mobile fragments with OPLL masses, successful anterior translation is confirmed by comparing the height of the protruding anterior portion of the vertebral bodies and the anteroposterior diameter measured before surgery.
Anterior column reconstruction with interbody cage insertion
Cervical interbody cages are packed with locally harvested bony fragments during discectomy and foraminotomy. Cage size and angle can be freely selected based on the height of the disc space with consideration of the physiological sagittal alignment. Through proper sized cage insertion, the cervical anterior column is temporarily stabilized for the next procedure (Figure 2C).
Resection of the protruding anterior vertebral bodies and cervical plating
The protruding portion of the anteriorly translated body is shaved down using a high-speed burr or Leksell rongeurs (Figure 2C) before applying anterior plating to enhance stability. When shaving down the anterior translated vertebral body with high speed burr, care must be taken not to damage the soft tissues and esophagus. The plate should be bent to fit the target sagittal alignment before placing. For additional anterior translation of mobilized vertebral bodies due to lag screw effect, screws are inserted via gradually tightening after proper drilling and tapping (Figure 2D). All patients are instructed to use a hard cervical brace for 6 weeks to ensure postoperative immobilization.
Results
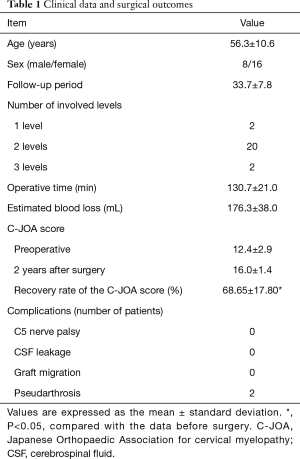
The study group included 24 patients (16 men and 8 women), with a mean age of 56.3±10.6 years. All patients were followed up at least 24 months, with an average follow-up period of 33.7±7.8 months. The mean C-JOA score improved from 12.4±2.9 preoperatively to 16.0±1.4 at the final follow-up (P<0.05). The mean recovery rate of the C-JOA score at the final follow-up was 68.65%±17.80% and no patient showed neurologic deterioration after surgery. The mean operating time was 130.7±21.0 minutes and the estimated blood loss was 176.3±38.0 mL.
The spinal level of OPLL involvement was 1 vertebral level for two patients, 2 levels for 20 patients, and 3 levels for two patients. The most common cases had OPLL over 2 vertebral levels (83.3%). In 22 cases (91.6%), radiographic fusion between vertebral bodies was achieved approximately 12 months after surgery. Pseudarthrosis was detected in two cases at 12 months of follow-up. However, solid fusion was achieved in all patients after 2 years postoperatively without any additional intervention. There were no perioperative complications, such as transient neurological deterioration, major vessel injury, esophageal perforation, instrumented failure, postoperative hematoma or CSF leakage (Table 1).
Full table
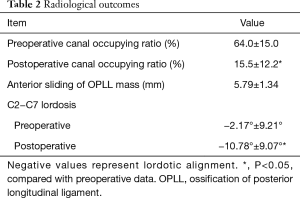
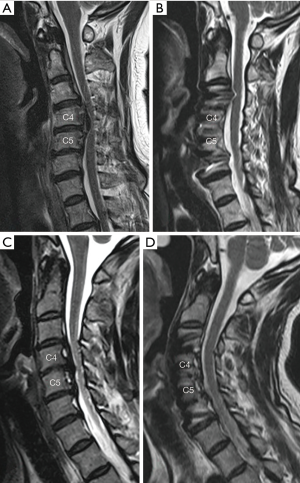
The mean canal compromised ratio decreased from 64.0%±15.0% preoperatively (Figure 3A,B) to 15.5%±12.2% postoperatively (Figure 3B,C,D) (P<0.05), with an average distance of anterior sliding of OPLL mass of 5.15±1.39 mm. Postoperative cervical sagittal angle was −10.78°±9.07° compared with preoperative −2.17°±9.21° (Figure 3E) to −10.78°±9.07° (Figure 3F). The mean recovery angle of sagittal cervical lordosis postoperatively was 9.80°±7.50° (Table 2).
Full table
Discussion
Although posterior decompression surgery is more commonly used for the treatment of cervical OPLL than anterior surgery, controversy still exists over the surgical options. Posterior surgery such as laminoplasty can safely achieve decompression of the spinal canal that results from multilevel involved OPLL (4,5,19-21). However, laminoplasty does not always achieve the expected canal expansion and spinal cord decompression for patients with a high occupying ratio or kyphotic alignment. Furthermore, posterior surgery is associated with higher incidence of transient C5 palsy, postoperative kyphotic deformity, aggravation of neck pain, and postoperative progression of OPLL masses in many studies (22-25).
On the other hand, anterior corpectomy and resection of OPLL are technically demanding and have high rates of surgery-related complications. However, some studies have suggested that anterior decompression surgery improves neurological outcomes in OPLL patients with a large OPLL mass and/or loss of cervical lordosis (7,9,12).
CSF leakage is a known complication linked to anterior corpectomy surgery and may lead to significant increases operating time (14,24,26). The “anterior floating method” was introduced as a way to minimize surgical invasion and leakage of CSF in conventional anterior corpectomy surgery by thinning ossified PLLs without detachment from the dura mater. This method leads to expansion of the canal by hydrostatic pressure produced by CSF to avoid unnecessary dural tearing. However, canal expansion with the floating method is not controlled by surgeon and often results in incomplete decompression of spinal canal.
As mentioned earlier, since the VBSO technique does not require direct manipulation of the interspace between the PLL and dura mater nor the complete removal of the involved vertebral bodies, it can significantly reduce the risk of dural tears and other complications related to resection of OPLL masses (16).
Pseudarthrosis following anterior cervical fusion surgery is also a major concern, and its incidence increases with fusion of multilevel vertebral bodies. Reportedly, the fusion rate in ACCF is 95.9% and 89.8% for one-level and two-level involvement, respectively. As the number of levels being fused increases, the risk of implant failure rate increased as well (12,13). Therefore, pseudarthrosis may cause persistent inappropriate segmental motions, which result in severe neck pain, radiculopathy or myelopathy, and instrument failure. It can sometimes lead to revision surgery. In conventional ACCF surgery, longer anterior column resection and fusions with a single large graft can increase the incidence of graft-related complications, such as extrusion and migration (12,13,22). However, since the VBSO procedure utilizes remaining vertebral bodies and OPLL masses as autogenous bone graft materials for the reconstruction of anterior column, this technique may increase the fusion rate (10).
Anterior cervical discectomy and fusion (ACDF) surgery has been generally applied for various cervical disorders (6,27). Hence, various surgical options and various design cages have been developed for multilevel ACDF to increase fusion rate and provide greater supportive strength. The multiple placements of these short interbody cages at each level combined with anterior plating distributes the load more evenly than multilevel corpectomy and fusion surgery using a long-distance, single-graft.
Numerous authors have reported that blood loss is greater in anterior corpectomy than that in posterior surgery. During anterior corpectomy, the majority of the surgical time, as well as excessive blood loss is usually due to the vertebral body resection and removal of the OPLL masses (7,9,12). Additionally, massive bleeding is a major cause of unclear view of surgical fields and insufficient decompression. In our study, the mean perioperative estimated blood loss was 176.3±38.0 mL and no postoperative hematomas occurred.
We developed the VBSO approach to overcome the risks related with anterior decompression of huge and adhesive OPLL masses. Manipulation of internal surfaces of ossified masses is very challenging as subtle compression of the mass can lead to irreversible cord damage. Sometimes, when an OPLL mass is tightly adhered to the dura mater attempts to resect or thin the mass can result in dural tearing and long-term CSF leakage. Therefore, we asked: “Must we try to remove all huge OPLL mass? Instead, could we translate the central body fragments along with the mass just like playing Jenga game?” We then realized we could achieve canal expansion and cord decompression very safely without the need to touch the OPLL mass (Figure 4).
Fortunately, since implementing this procedure in 2012 we have not experienced any irreversible serious complications apart from one case of dural tearing during root decompression and one case of transient C5 root palsy after 102 procedures. Since 2013, our findings have been presented at many spine meetings including the Cervical Spine Research Society (28).
Conclusions
VBSO, a novel anterior decompression provides similar neurological outcomes to conventional corpectomy. This technique does not involve a direct manipulation of the OPLL lesion or dissection of the interspace between the ossified PLL and dura mater which may reduce the risk of complications, operation time, and intraoperative blood loss. Furthermore, VBSO is based on the multilevel discectomy and fusion technique; thus, it may contribute to restoration of physiologic lordosis and high fusion rates. Therefore, the VBSO may be an effective and safe option for anterior decompression surgery in patients with cervical myelopathy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Institutional Review Board of our hospital (No. S2018-2175-0001) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Epstein N. Diagnosis and surgical management of cervical ossification of the posterior longitudinal ligament. Spine J 2002;2:436-49. [Crossref] [PubMed]
- Choi BW, Song KJ, Chang H. Ossification of the posterior longitudinal ligament: A review of literature. Asian Spine J 2011;5:267-76. [Crossref] [PubMed]
- Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine (Phila Pa 1976) 2012;37:E309-14. [Crossref] [PubMed]
- An HS, Al-Shihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg 2014;22:420-9. [Crossref] [PubMed]
- Shin JH, Steinmetz MP, Benzel EC, et al. Dorsal versus ventral surgery for cervical ossification of the posterior longitudinal ligament: considerations for approach selection and review of surgical outcomes. Neurosurg Focus 2011;30:E8. [Crossref] [PubMed]
- Fraser JF, Härtl R. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. J Neurosurg Spine 2007;6:298-303. [Crossref] [PubMed]
- Liu X, Min S, Zhang H, et al. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis. Eur Spine J 2014;23:362-72. [Crossref] [PubMed]
- Edwards CC 2nd, Heller JG, Murakami H. Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine (Phila Pa 1976) 2002;27:1168-75. [Crossref] [PubMed]
- Chen Z, Liu B, Dong J, et al. Comparison of anterior corpectomy and fusion versus laminoplasty for the treatment of cervical ossification of posterior longitudinal ligament: a meta-analysis. Neurosurg Focus 2016;40:E8. [Crossref] [PubMed]
- Lee DH, Joo YS, Hwang CJ, et al. A novel technique to correct kyphosis in cervical myelopathy due to continuous-type ossification of the posterior longitudinal ligament. J Neurosurg Spine 2017;26:325-30. [Crossref] [PubMed]
- Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976) 2008;33:E990-3. [Crossref] [PubMed]
- Macdonald RL, Fehlings MG, Tator CH, et al. Multilevel anterior cervical corpectomy and fibular allograft fusion for cervical myelopathy. J Neurosurg 1997;86:990-7. [Crossref] [PubMed]
- Sasso RC, Ruggiero RA Jr, Reilly TM, et al. Early reconstruction failures after multilevel cervical corpectomy. Spine (Phila Pa 1976) 2003;28:140-2. [Crossref] [PubMed]
- Min JH, Jang JS, Lee SH. Significance of the double-layer and single-layer signs in the ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine 2007;6:309-12. [Crossref] [PubMed]
- Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: Part 1: Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976) 2007;32:647-53. [Crossref] [PubMed]
- Lee DH, Cho JH, Lee CS, et al. A novel anterior decompression technique (vertebral body sliding osteotomy) for ossification of posterior longitudinal ligament of the cervical spine. Spine J 2018;18:1099-105. [Crossref] [PubMed]
- Lin W, Ha A, Boddapati V, et al. Diagnosing Pseudoarthrosis After Anterior Cervical Discectomy and Fusion. Neurospine 2018;15:194-205. [Crossref] [PubMed]
- Ghiselli G, Wharton N, Hipp JA, et al. Prospective analysis of imaging prediction of pseudarthrosis after anterior cervical discectomy and fusion: computed tomography versus flexion-extension motion analysis with intraoperative correlation. Spine (Phila Pa 1976) 2011;36:463-8. [Crossref] [PubMed]
- Fujimori T, Iwasaki M, Okuda S, et al. Long-term results of cervical myelopathy due to ossification of the posterior longitudinal ligament with an occupying ratio of 60% or more. Spine (Phila Pa 1976) 2014;39:58-67. [Crossref] [PubMed]
- Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8:693-9. [Crossref] [PubMed]
- Iwasaki M, Kawaguchi Y, Kimura T, et al. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 2002;96:180-9. [PubMed]
- Shamji MF, Massicotte EM, Traynelis VC, et al. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976) 2013;38:S195-209. [Crossref] [PubMed]
- Sakaura H, Hosono N, Mukai Y, et al. C5 palsy after decompression surgery for cervical myelopathy: review of the literature. Spine (Phila Pa 1976) 2003;28:2447-51. [Crossref] [PubMed]
- Sakai K, Okawa A, Takahashi M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976) 2012;37:367-76. [Crossref] [PubMed]
- Lee DH, Cho JH, Kim NH, et al. Radiological risk factors for progression of ossification of posterior longitudinal ligament following laminoplasty. Spine J 2018;18:1116-21. [Crossref] [PubMed]
- Matsuoka T, Yamaura I, Kurosa Y, et al. Long-term results of the anterior floating method for cervical myelopathy caused by ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976) 2001;26:241-8. [Crossref] [PubMed]
- Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine (Phila Pa 1976) 2011;36:2045-50. [Crossref] [PubMed]
- Lee DH, Riew KD, Choi SH, et al. Safety and Efficacy of a Novel Anterior Decompression Technique for Ossification of Posterior Longitudinal Ligament of the Cervical Spine. J Am Acad Orthop Surg 2019. [Epub ahead of print]. [Crossref] [PubMed]