Navigating the learning curve of spinal endoscopy as an established traditionally trained spine surgeon
Introduction
Endoscopic spine has been practiced the world over for over 30 years. The body of peer-reviewed literature demonstrating that clinical effectiveness has grown substantially (1-8). The acceptance of endoscopic spinal surgery by established spine surgeons is impacted by academic, regulatory, and reimbursement (9-11). Up until recently, no billing code was available in the United States. In 2017, a new code—62380—was included in the American Medical Association’s (AMA) current procedural terminology (CPT) system for reimbursement. The lack of a reimbursement mechanism for surgical services, including spinal endoscopy, has significantly hampered the broader implementation of spinal endoscopy in the United States. Therefore, it is no surprise that historically spinal endoscopy has been treated as a stepchild of spinal surgery. The training standards for teaching endoscopic techniques in postgraduate surgical residency and fellowship programs have not been established. To date, there is no formalized easy way for practicing spine surgeons wanting to familiarize themselves with the techniques and clinical protocols of spinal endoscopy (12,13). Neither the North American Spine Society (NASS) nor the American Academy of Orthopedic Surgeons (AAOS) offers any master courses or instructional courses lectures on spinal endoscopy. The American Association of Neurological Surgeons (AANS) also has nothing to offer to the aspiring endoscopic spine surgeon. Most are left to become autodidacts after a weekend cadaver course sponsored by industry; few are lucky enough to have an opportunity to be taken in by an established key opinion leader (KOL) mentor. Others are fortunate enough to have access to a local preceptor who may take them under their wings over a more extended period. The problem is obvious. How is a busy spine surgeon to retool her or his practice with limited time to invest in a formal training program?
The first author is an orthopedic spine surgeon who has been in practice for over 28 years. The majority of his practice was and currently still is devoted to the open surgical treatment of degenerative conditions of the lumbar and cervical spine. The second author is also an orthopedic spine who has been in practice for more than 12 years. He completed a spinal deformity fellowship and devoted and a substantial part of his practice to long-segment corrective surgeries. The remaining two authors are orthopedic spine surgeons with an extensive background in spinal endoscopy. The senior author, Dr. Anthony Yeung, has pioneered endoscopic spinal surgery in the United States since 1992. He has treated over 11,000 patients with the procedure and has been recognized as one of the few remaining of the original group of pioneer KOL. The third author, Dr. Kai-Uwe Lewandrowski, has been practicing endoscopic spinal surgery since 2006 and has devoted his practice to the advancement and application of endoscopic spinal surgery techniques to common everyday clinical problems of the lumbar and cervical spine. Both the senior and the third author—the teaching surgeons—have served in the capacity of training other spine surgeons with the intent of improving traction with the endoscopic spinal surgery among traditionally trained spine surgeons. They have organized training national and international courses including courses for the International Intradiscal Therapy Society (IITS), International Society of Advancement of Spine Surgery (ISASS), and the North American Spine Society. At their surgical facilities—the Desert Institute of Spine Care (DISC, Phoenix, AZ, USA) and the Surgical Institute of Tucson (SIT, Tucson, AZ, USA) —both authors trained spine surgeons in endoscopic spine surgery employing either a mentorship (short course or fellowship), or a proctorship training model (prolonged fellowship and hands-on surgical training).
The first and second authors of this article—the apprentice surgeons—describe how they as established traditionally trained spine surgeons learned endoscopic spine surgery under these training models and how their clinical decision making in their day to day practice regarding their preferred treatment recommendation to patients for open versus endoscopic surgery changed over time. They describe the learning curve, pitfalls, and the pace of integrating it into their routine clinical practice with increasing comfort level as they gained more experience with the endoscopic spinal decompression procedure.
Methods
From recognizing the need to bridging the gap
The first author (NA Ransom), has closely worked together with the third author in a traditional practice setting where he has seen first-hand how patients benefit from minimally invasive spinal surgery techniques, including endoscopy. He attended a cadaver course and started assisting the third author and eventually performed lumbar endoscopic decompression on his own patients together with the third author (KU Lewandrowski). The idea of a preceptorship program to help the first author with the selection of suitable patients for the endoscopic decompression, acquire the necessary hands-on surgical skills, and recognize the videoendoscopic surgical transforaminal anatomy was born. The first author became more interested in learning spinal endoscopy side-by-side once he quickly realized there were no formal course programs offered by AAOS and NASS. International courses and short weekend courses run by companies were impractical, and small courses by subspeciality spine society course were few far and between.
The second author (S Gollogly) had painful cervical and lumbar spine disease. He suffered from C6 radiculopathy at age 39 and suffered from a herniated L2/3 lumbar disc at age 45. Both problems ultimately were treated surgically. As a practicing spine surgeon, the second author did know about the future burden associated with fusion surgeries and after his personal experiences with spinal surgery sought to add less aggressive and more straightforward protocols to his practice to treat lumbar disc herniations and spinal stenosis. After 12 years of practice in the same location, the second author sought to learn alternative, less disruptive techniques. He found out that formalizing training in endoscopic spine surgery was not straightforward. In 2017, the International Society for Minimal Intervention in Spinal Surgery (ISMISS) offered a one-day course at their annual meeting in Chicago, IL. For the first time, the second author had the opportunity to insert an endoscope and perform a transforaminal decompression of the intervertebral disc. In the cadaver lab, the actual surgery was simulated with an identical setup. The three-dimensional anatomy of the spine, as seen through the endoscope, became a new perspective. The next step was to find a mentor. Eventually, he found Dr. Yeung, who proctored him in his injection suite, and operating room at the Desert Institute of Spine Care (DISC) in Phoenix, Arizona. During this visit, the entire protocol from the initial consultation, diagnostic injection to the endoscopic surgery was reviewed. In this mentorship setting, numerous clinical scenarios were discussed in greater detail than at cadaver courses or instructional lectures.
The transition during mentorship & preceptorship
When he first considered transitioning endoscopic spine surgery into their practice, the first author had a hospital-based spine practice with an emphasis on the degenerative spine. The third author assisted him during his initial endoscopic surgeries. The first author regarded performing his first endoscopic surgeries in this familiar hospital setting as ideal because he would be able to deal with any unforeseen problems and convert the operation to open should he not be able to perform an adequate decompression. Typically, patients were sent home from the recovery room at the hospital. Later, the first author performed endoscopic surgeries with the third author at his outpatient surgical facility in Tucson, Arizona. The second author had some experience with outpatient spine surgery at an Ambulatory Surgery Center (ASC) in Monterey, California. Therefore, adding selective nerve root blocks and epidurograms to his ASC program was straightforward.
Before scheduling their first endoscopic spine surgery, both apprentice surgeons started with perfecting transforaminal epidural steroid injections (TESI). Dr. Yeung taught the skills to outline the course of the traversing and exiting nerve roots during routine epidurogram. Whether in the mentorship or preceptorship scenario, both apprentice surgeons familiarized themselves with the transforaminal injections was a significant stepping stone in increasing the level of confidence to access the neuroforamen safely. The apprentice surgeons performed their first selective endoscopic discectomy (SED™) after 20 to 50 TESI.
Surgical techniques & patient selection for the learning curve
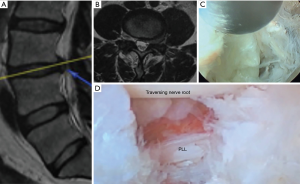
The first author followed the teachings of KUL who has been performed endoscopic spinal procedures since 2007 at the Center for Advanced Spine Care of Southern Arizona in Tucson Arizona (14). Patients treated with the transforaminal outside-in decompression procedure popularized by Hoogland et al. (15). The first author’s surgical techniques are a modification of the transforaminal approach initially described by Hoogland. The second author followed the senior author’s inside-out technique, who established his endoscopic outpatient spinal surgery program at the Squaw Peak Facility in Phoenix, Arizona, 21 years ago (2). It was later integrated into the Desert Institute of Spine Care founded by his son—Christopher Yeung—in 2003. The inclusion and exclusion criteria have been described in detail elsewhere (16). In brief, patients with lumbar radiculopathy, dysesthesias, and decreased motor function refractory to 12 weeks of conservative care due to foraminal or lateral recess stenosis confirmed on magnetic resonance images (MRI), and computed tomography (CT) scans are appropriate candidates for the lumbar endoscopic decompression procedure. At the recommendation of their respective proctors and mentors, the apprentice surgeons consented patients, for lateral herniated disc. The initial spinal endoscopies were for far lateral and foraminal disc herniations since they are often difficult to access using a standard translaminar approach (Figure 1). More difficult surgical indications, including broad-based central protrusions in overweight patients, were performed after several successful endoscopic discectomies. Patients with severe central stenosis (less than 100 mm2) (10), massive facet hypertrophy, infection, or metastatic disease were deemed not suitable for this procedure. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Clinical follow-up & outcome analysis
After each surgery, the patient was typically evaluated at 2, 6, and 12 weeks, and after that at 6, and 12, postoperatively. Additional visits were scheduled to deal with any unexpected problems. Primary clinical outcomes measures were the visual-analog scales (VAS) (17) for leg pain ranging from no pain [0] to worst pain [10] and the Oswestry disability index (ODI) (18). Macnab outcomes (19) were scrutinized in order of priority for inflammatory DRG irritation, recurrent stenosis, and instability, or the emergence of other pain generators postoperatively. Descriptive statistics and simple two-way cross-tabulations were performed to measure any statistically significant association between variables using IBM SPSS Statistics software, Version 25.0. Pearson Chi-Square and Fisher’s exact test were employed to assess the strength of association between variables statistically. The mean, range, and standard deviation, and percentages of all nominal variables were calculated.
Results
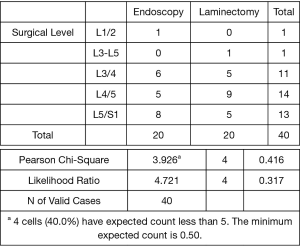
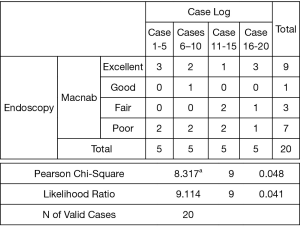
The first author—NA Ransom—performed a retrospective review of his clinical decision making regarding lumbar decompression procedures with increasing knowledge of spinal endoscopy. The author analyzed a total of 40 patients with 20 open control laminectomies and 20 endoscopic decompression cases for similar clinical problems, including sciatica-type low back and leg pain without instability. Patients consisted of 22 females and 18 males who underwent surgery between 2011 and 2018 with an average follow-up of 38.58 months (range 19 to 66 months). Descriptive statistics showed an average age of 57.38 years. The level distribution between the open laminectomy and the endoscopy group was nearly identical without any statistically significant difference (Figure 2). As expected L4/5, and L5/S1 were the most commonly operated levels. The preoperative VAS for patients in both groups was 7.95 compared to the postoperative VAS at final follow-up of 4.01. Paired T-testing showed a statistically significant reduction with a P value of <0.001. Crosstabulation of clinical outcomes with several confounding variables, including reduced posterior disc height, the size of the disc herniation, smoking status, and BMI > than 30 were analyzed. As expected, the analysis showed statistically greater clinical improvements as measured by the postoperative Macnab criteria in patients with less advanced disc degeneration as evidenced by a posterior disc height greater than 3 mm (P=0.048). Crosstabulation of Macnab outcomes by laminectomy and endoscopy showed similar clinical improvements without any statistically significant difference. Plotting outcomes against the number of surgical cases showed that poor clinical outcomes were obtained during the first 15 cases. The first author’s clinical outcomes improved after 15 cases despite the increasing complexity of endoscopic surgeries (Figure 3). The first author started with extraforaminal herniations (Figure 1) and progressed to surgically treating more difficult contained central and paracentral herniation (Figure 4) after his first 15 cases. The overall success rate with the endoscopic procedure by NAR was 65% (all improved Macnab categories) compared to 70% with the open laminectomy (P=0.036).
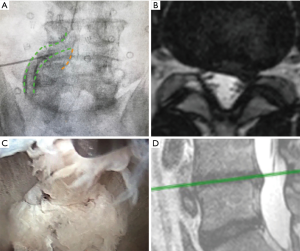
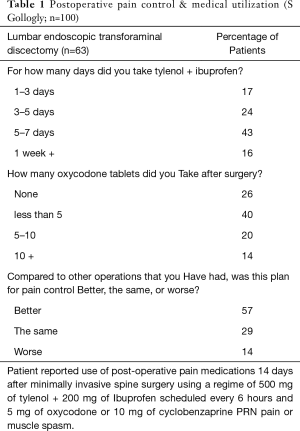
The second author—S Gollogly—had a similar experience. He operated on 15 patients with far-lateral, foraminal, or central contained disc herniations (Figure 5). After this initial series, improved proficiency with the procedure gave the second author more confidence to tackle more complex problems, such as recurrent disc herniation after previous open discectomy. In some select cases, free fragments were removed by judiciously employing the selective nerve root block and epidurogram techniques (Figure 6). For the next 12 months, a total of 65 patients underwent endoscopic spinal operations with good clinical outcomes and some failures, including two patients suffering from recurrent disc herniations which ultimately required re-operation. None of the endoscopically operated patients were readmitted to a hospital after their discharge from the ASC. There were no infections, and patients reported high satisfaction with the overall ASC experience. This initial cohort of cases has solidified the author’s understanding of the endoscopic anatomy. Successful implementation of the endoscopic transforaminal decompression procedure also allowed to solidify ASC pain management protocols relying less on opiate pain medication and more on a combination of 500 mg of tylenol + 200 mg of Ibuprofen every 6 hours and 5 mg of oxycodone or 10 mg of cyclobenzaprine as needed for pain and muscle spasms (Table 1). The overall clinical success rate was 57% for SG.
Full table
Discussion
The aspiring endoscopic spine surgeon may encounter many barriers to transition away from conventional spine surgery. They range from institutional barriers to hurdles related to the high initial upfront cost of capital equipment purchases and disposables, lack of acceptance in the local health care market, difficulty with insurance preauthorization and reimbursement, and many others. Some surgeons may also encounter a crucial psychological barrier when having to start all over again when leaving the familiar territory of open spine surgery. Many surgeons have gained extensive experience with its routine clinical application with confidence—something that will have to be rebuilt when starting an endoscopic spine practice. This author can report from first-hand experience that every anatomical structure routinely evaluated during open spine surgery has a different appearance on endoscopic video visualization. Therefore, to guarantee a successful transition from conventional open spine surgery to an endoscopic spine practice surgeons should aim to:
- Understand the pathophysiology of neurogenic pain and neurogenic claudication must be understood;
- Correlate surgical anatomy with symptomatic pain generators;
- Employ a staged management approach by opting for the least invasive treatment first;
- Avoid fusion for surgical pain management unless there is gross instability or deformity.
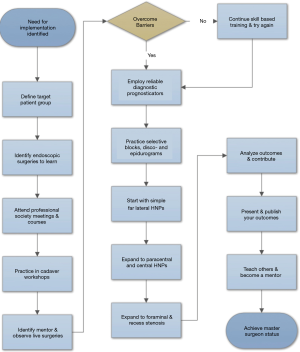
The apprentice surgeon authors of this article recognized during their careers as an established spine surgeon that there is a role for smaller targeted endoscopic outpatient procedures and consequently integrated them into their clinical program alongside traditional open and other minimally invasive spinal surgeries. As shown by the story told in this study, the transition from traditional open surgeries to endoscopic spine surgery was not smooth and in the opinion of the apprentice surgeons’ opinion cannot be accomplished only by attending an industry-sponsored weekend course. The apprentice surgeons of this study utilized all available avenues with training courses organized by subspecialty societies, such as the ISMISS or the International Intradiscal Therapy Society (IITTSS). However, the one single most crucial factor in succeeding with the implementation of endoscopic spine surgery into the traditional spinal surgery program was having a mentor or a preceptor. Perhaps, someday formalized training in residency and fellowship programs or formalized training provided by national and international surgeon’s organizations may become available. Until then, mentorship and proctorship seem to be the best option for any surgeon attempting to integrate spinal endoscopy in her or his practice. An implementation plan for spinal endoscopy into a well-established spine practice is suggested in the flow chart presented in Figure 7.
In the current state of spinal endoscopy training, both teaching surgeons (KU Lewandrowski & A Yeung) find a mentor- or proctorship program to educate the aspiring endoscopic spine surgeons on these core principles of endoscopic spine surgery to a high competence level more suitable that relatively short surgical workshops or visitations. Additional training opportunities lie in cadaver workshops focusing on cadaveric dissection and anatomic study. The authors recommend the aspiring endoscopic spine surgeon to actively participate in professional societies and mentorships to discuss the clinical application of the various endoscopic surgical pain management techniques to understand the appropriate patient selection better. The learning curve for experienced and committed traditionally trained spine surgeons under close supervision either in a mentor- or proctorship scenario may be approximately 15 cases. Both apprentice surgeons attempted more complex cases after having completed 15 cases. On the basis of this data, the teaching surgeons of this study propose the following criteria for the credentialing of endoscopic spine surgeons:
- Evidence of technical and clinical competence after completion of an acredited training program;
- Passing of a standardized technical proficiency examination administered by credentialed peers;
- Ability to manage potentially harmful complications.
At the moment, there is no widely accepted core curriculum detailing appropriate qualifications and competency requirements for endoscopic spinal surgery. Therefore, an institution offering endoscopic spine surgery currently must rely on the medical staff to craft their own standards. This could open the door to potential abuse of the institutional peer review system if the aspiring endoscopic surgeon encounters complications during the initial learning curve mainly if the senior spine surgeons at their institution are critical of spinal endoscopy. Therefore, a formalized credentialing process should be instituted as professional interest in this subspecialty continues to grow. The controversy as to who can be credentialed to perform endoscopic spine surgery and after fulfilling what type of training will most likely continue.
Conclusions
Patients with symptomatic foraminal stenosis can be treated favorably with early outside-in transforaminal endoscopic decompression. Many traditionally trained spine surgeons who routinely performs open surgery are interested in learning endoscopic spine surgery but do not know how to start the process of integrating it into their busy well-established spine practice. Proctorship and mentorship programs are an effective way to acquire endoscopic surgery skills without compromising patient safety, clinical outcomes, or jeopardizing one’s well run general spine surgery practice. Under the close guidance of an endoscopic master spine surgeon, the endoscopic learning curve may be comprehended by the experienced traditionally trained spine surgeon in approximately 15 lumbar decompression cases.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no direct (employment, stock ownership, grants, patents), or indirect conflicts of interest (honoraria, consultancies to sponsoring organizations, mutual fund ownership, paid expert testimony). The authors are not currently affiliated with or under any consulting agreement with any vendor that the clinical research data conclusion could directly enrich. This manuscript is not meant for or intended to endorse any products or push any other agenda other than to report the associated problems with learning endoscopic spinal surgery and the clinical outcomes during the learning curve. The motive for compiling this clinically relevant information is by no means created and/or correlated to directly enrich anyone due to its publication. This publication was intended to substantiate contemporary endoscopic spinal surgery concepts to facilitate technology advancements.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Choi G, Pophale CS, Patel B, et al. Endoscopic Spine Surgery. J Korean Neurosurg Soc 2017;60:485-97. [Crossref] [PubMed]
- Yeung AT. Transforaminal endoscopic decompression for painful degenerative conditions of the lumbar spine: A review of one surgeon’s experience with over 10,000 cases since 1991. J Spine Neurosurg 2017;6:266.
- Yeung AT. The Yeung Percutaneous Endoscopic Lumbar Decompressive Technique (YESSTM). J Spine 2018;7:408. [Crossref]
- Yeung AT, Kotheeranurak V. Transforaminal endoscopic decompression of the lumbar spine for stable degenerative spondylolisthesis as the least invasive surgical treatment using the YESS surgery technique. J Spine 2018;7:407. [Crossref]
- Yeung AT. In-vivo endoscopic visualization of pain generators in the lumbar spine. J Spine 2017;6:385. [Crossref]
- Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician 2015;18:61-70. [PubMed]
- Birkenmaier C, Komp M, Leu HF, et al. The current state of endoscopic disc surgery: review of controlled studies comparing fullendoscopic procedures for disc herniations to standard procedures. Pain Physician 2013;16:335-44. [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. [Crossref] [PubMed]
- Belatti DA, Phisitkul P. Trends in orthopedics: an analysis of Medicare claims, 2000-2010. Orthopedics 2013;36:e366-72. [Crossref] [PubMed]
- Pannell WC, Savin DD, Scott TP, et al. Trends in the surgical treatment of lumbar spine disease in the United States. Spine J 2015;15:1719-27. [Crossref] [PubMed]
- Morgenstern R, Morgenstern C, Yeung AT. The learning curve in foraminal endoscopic discectomy: experience needed to achieve a 90% success rate. SAS J 2007;1:100-7. [Crossref] [PubMed]
- Meyers JE, Wang J, Khan A, et al. Trends in Physician Reimbursement for Spinal Procedures Since 2010. Spine (Phila Pa 1976) 2018;43:1074-9. [PubMed]
- Huang TJ, Kim KT, Nakamura H, et al. The State of the Art in Minimally Invasive Spine Surgery. Biomed Res Int 2017;2017:6194016. [PubMed]
- Lewandrowski KU. "Outside-in" technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: a retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg 2014. doi: . eCollection 2014. [Crossref]
- Hoogland T, Schubert M, Miklitz B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31:E890-7. [Crossref] [PubMed]
- Yeung A, Roberts A, Zhu L, et al. Treatment of Soft Tissue and Bony Spinal Stenosis by a Visualized Endoscopic Transforaminal Technique Under Local Anesthesia. Neurospine 2019;16:52-62. [Crossref] [PubMed]
- Huskisson EC, Jones J, Scott PJ. Application of visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976;15:185-87. [Crossref] [PubMed]
- van Hooff ML, Mannion AF, Staub LP, et al. Determination of the Oswestry Disability Index score equivalent to a "satisfactory symptom state" in patients undergoing surgery for degenerative disorders of the lumbar spine-a Spine Tango registry-based study. Spine J 2016;16:1221-30. [Crossref] [PubMed]
- Macnab I. Negative disc exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]