
Five-year clinical outcomes with endoscopic transforaminal foraminoplasty for symptomatic degenerative conditions of the lumbar spine: a comparative study of inside-out versus outside-in techniques
Introduction
Lumbar endoscopic spinal decompression surgery has been validated to be both safe and effective in recently published long-term follow-up studies suggesting that the procedure may be the answer to the call for a more direct simplified, and more cost-effective spinal decompression procedure (1). Staged outpatient endoscopic decompression of a painful degenerative lumbar motion segment causing back pain, claudication- and sciatica-type back and leg symptoms is a less disruptive alternative procedure compared to traditional more surgically invasive decompression and fusion surgeries (2). In many cases, the patients’ subjective weakness, back pain, and intermittent claudication limiting walking endurance and other physical activities can be traced back to unilateral or single-level foraminal stenotic process (3).
There are two main well established endoscopic spinal decompression procedures. Yeung pioneered his widely publicized YESS™ inside-out foraminoplasty technique (4,5) in the 1990s (6). Hoogland was one of a few prominent European pioneer surgeons, a colleague of Yeung, who ultimately popularized the outside-in technique (7) which emerged over the years into an alternative to the inside-out endoscopic surgical protocol to treat lumbar herniated disc and spinal stenosis. Hoogland’s surgical concept followed the surgical decompressive technique developed for chymopapain injection into the intervertebral disc utilizing the lateral intradiscal approach. While both techniques have similar goals of decompressing the neural elements, some procedural steps vary considerably with reduced reliance on intradiscal therapies with the outside-in foraminal decompression by serial dilation. The outside-in technique may also impact long-term clinical outcomes, but could lead to higher failure to cure rates by ignoring the importance of intradiscal therapy.
When studied by traditionally trained surgeons because the entire foraminal zone is not adequately or wholly visualized with the translaminar approach that is dependent on extensive removal of the facet to expose the extraforaminal zone. It is best visualized minimally invasively with direct visualization using the foraminal endoscope. While the extraforaminal region can be reached through Wiltse’s extraforaminal approach, visualization is still less effective and dependent on palpation of the lateral recess without destabilization of the spinal segment. Direct visualization with the endoscope is still the most effective method because it can visualize soft tissue as well as bony stenosis. This approach is also aided and enhanced by surgical treatment using only local anesthesia, where the patient can provide intra-operative feedback during surgery.
In this comparative study, the authors attempted to establish long-term primary functional results with outcome measures, complication- and reoperation rates in patients who underwent inside-out and outside-in endoscopic transforaminal decompression for symptoms related to foraminal stenosis. The authors’ extensive experience with the transforaminal endoscopic a surgical approach to treat symptomatic conditions of the lumbar spine is discussed in this paper comparing the inside-out with the outside-in transforaminal techniques in the context of long-term survival of the clinical treatment effect.
Methods
Study groups
The first author (A Yeung) selected 86 consecutive patients who underwent transforaminal endoscopic foraminoplasty decompression for degenerative foraminal stenosis before 2015 at the Dessert Institute for Spine Care using A. Yeung’s philosophy and selective endoscopic discectomy (SED™) technique of endoscopic decompression (5). Of the 86 inside-out patients 22 (25.6%) were women, and 64 (74.4%) were men.
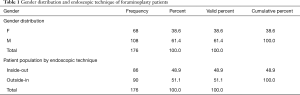
The second author (KU Lewandrowski) provided 90 patients for this comparative analysis who had transforaminal endoscopic surgery at the Center for Advanced Spine Care of Southern Arizona for the treatment of foraminal stenosis due to lumbar herniated disc and spinal stenosis employing the outside-in decompression procedure popularized by Hoogland et al. (7). The outside-in technique was also utilized for symptomatic disc herniation without foraminal stenosis, but the technique adapted foramioplasty inherent in Hoogland’s original approach and technique with serial dilation was later modified by KUL as described below (8). The outside-in patients were operated between the years of 2012 to 2014 and included 46 females, and 44 males between the ages of 19 to 84 years. Therefore, this study had two patient groups: group 1—inside-out (86 patients), and group 2—outside-in (90 patients). The total study population consisted of 176 patients consisted of 68 males and 108 females (Table 1). Patients of both groups were followed for a minimum of 5-year using the following inclusion criteria:
- Complaints of lumbar radiculopathy, dysesthesias, and decreased walking endurance due to neurogenic claudication;
- Symptoms correlating with foraminal or lateral recess stenosis shown on preoperative magnetic resonance images (MRI) and computed tomography (CT) scans using radiographic criteria described below;
- Failed conservative management with physical therapy and transforaminal epidural steroid injections to the patient’s clinical satisfaction.
- Definitive diagnostic work-up correlating physical examination, and imaging studies with favorable response to diagnostic and therapeutic injections to identify the symptomatic pain generator as described below.
Full table
The following exclusion criteria were used:
- Patients with severe central stenosis (less than 100 mm2) that were better candidates for translaminar decompression (9);
- Metastatic disease,
- Patients thought to be poor candidates by their unexpected or inconclusive response to diagnostic and therapeutic injections performed by the operating surgeon.
- Spondylolisthesis with anterolateral translation of more than 3–5 mm or rotation of more than 10 to 15 degrees in the extension/flexion views (10).
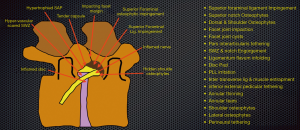
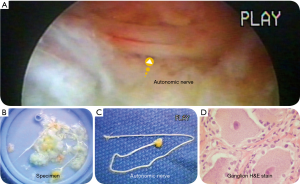
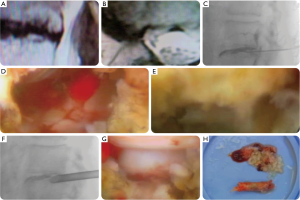
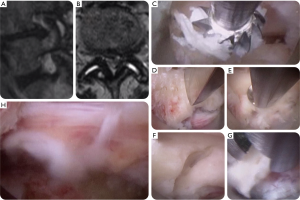
Preoperative image-based findings were correlated with intraoperative evaluation of the patients’ specific predominant pain generators. Analysis of Yeung’s extensive database of patho-anatomic pain generators found nine common endoscopic visualized painful conditions: (I) inflammed disc; (II) inflamed nerve; (III) hypervascular scar; (IV) hypertrophied superior articular process (SAP) and ligamentum flavum; (V) tender capsule; (VI) impacting facet margin; (VII) superior foraminal facet osteophyte; (VIII) superior foraminal ligament impingement; and (IX) hidden shoulder osteophyte (Figure 1). Additional intradiscal painful conditions that can be better visualized with the inside-out technique because of the more medial position of the working cannula underneath the dural sac. Patho-anatomy visualized through the endoscope included autonomic nerves, furcal nerves, conjoined nerves, and synovial cysts. An example of an anamolous autonomic nerves and their anatomic location in the lumbar neuroforamen is illustrated in Figure 2. All patients in this consecutive case series provided informed consent and IRB approval was obtained (CEIFUS 106-19).
Radiographic classifications
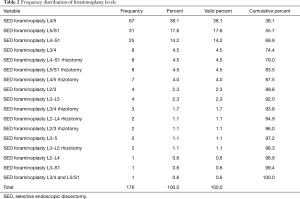
Previously published radiographic classification systems were used to classify the severity and location of the stenotic process in the neuroforamen (11-14). Neuroforaminal stenosis was classified according to Lee by dividing the neuroforamen from medial to lateral into entry-, middle-, and exit zone (15). Each zone has a predominant pathology causing neural compression. Hypertrophy of the superior articular facet is typical of entry zone stenosis. An osteophyte underneath the pars interarticularis is a common cause of mid-zone stenosis, whereas exit zone stenosis is often due to a subluxed and hypertrophic facet joint. The foraminal and lateral recess stenosis was recorded by noting the location of the main offending pathology. A posterior intervertebral disc height of less than 3–4 mm and a lumbar neuroforaminal height of 15 mm or less was considered radiographic evidence of spinal stenosis (12). These radiographic descriptors of foraminal stenosis have previously been employed by the authors and were used in this study to stratify patients for the further diagnostic workup of the level(s) believed to be causing the patient’s symptoms (see below) (13). The frequency distribution of selective endoscopic foraminoplasty discectomy (SEDTM) procedures performed is listed by level in Table 2 with the L4/5 (37.5%; 66/176 patients) and the L5/S1 (17.6%; 31/176 patients) levels being the most common stenotic locations treated endoscopically with a transforaminal decompression. The comparative analysis of 5-year long-term clinical outcomes with either the inside-out or outside-in endoscopic transforaminal lumbar foraminoplasty was done using these radiographic descriptors.
Full table
Prognosticators of successful outcome
History and physical examination (H&P) is a factor in establishing the diagnosis of clinical symptoms of foraminal stenosis. The physical exam, however, may be “normal” while resting. Abnormalities in motor and sensory function patients were subjectively elicited when patients were asked reproduce their symptoms creating their clinical complaints. Electrodiagnostic EMG and nerve conduction studies were sometimes used to elucidate the clinical severity of symptoms. However, there may be questions on the severity and disabling aspects of pain by the complaining patient. When the pain generator is correlated with diagnostic and therapeutic injections and confirmed by visualizing the patho-anatomy of each individual’s pain, this publication provides clinical information on surgical pain care. Some patients may be misinformed about unrealistically expecting to have no pain, and must be counselled about endoscopic spine surgery, no matter how low risk and effective. Because of their low specificity and sensitivity, the authors also did not routinely employ electrodiagnostic studies in the preoperative workup of patients but reviewed them whenever they were available. The EMG may be “normal” or “abnormal,” but abnormal interpretation was considered by the authors as a validation the patient’s subjective complaints (5). Peripheral neuropathy and other co-morbidities may increase the risk of complications (4-6), and failure to “cure” and are often diagnosed by nonsurgical physicians to offer a diagnosis because there was no other clinical diagnosis to explain the patient’s symptoms.
The patient’s actual symptoms do not always correspond to traditional imaging studies (16). Diagnostic and therapeutic transforaminal epidural steroid injections (TESI) containing steroids and/or a local anesthetic are more reliable predictors of successful clinical outcomes with the transforaminal decompression procedure (17). Given the high positive predictive value of preoperative diagnostic TESI of 98.38%, successful outcomes were expected with the transforaminal decompression if patients had a diagnostic response to the injection by reporting a 50–75% reduction in pain on the visual analog scale for back and leg (15,18,19). Intraoperative epidurograms may provide additional information by delineating extent and location of foraminal compression due to disc protrusion and other anatomic abnormalities.
Surgical steps inside-out techniques
Yeung’s inside-out philosophy and technique was trademarked in 2000 as an intradiscal therapy procedure arising from Kambin’s original concept of staying inside the disc. The underlying concept of chymopapain was validated by 2 large level 1 double blind studies and 38 cohorts studies (20). Low-dose chymopapain used during the early era of intradiscal therapy by intradiscal injection aided in the removal of the nucleus pulposis embedded in the annular defect causing annular deformity and pain (21). Endoscopic surgery evolved gradually on that basis after chymopapain was taken off the market by the FDA in the United States following scientific validation of its efficacy as new endoscopes, surgical instruments, laser, and bipolar flexible electrothermal radiofrequency devises were developed and FDA approved.
Yeung’s inside-out techniques were employed in group 1 patients. The working sheath is placed into the intervertebral disc with a custom designed cannula in his YESSTM endoscopic system, used to rest on the annulus, and used to retract and avoid injuring the exiting nerve root. A foraminoplasty is performed in patients with foraminal and lateral stenosis to treat discogenic pain and radiculopathy due to herniated discs (Figure 3) (2). The patient was positioned in prone position and surgery was performed under local anesthesia with or without sedation in all patients. During foraminoplasty, percutaneous small tooth trephines controlled and directed using pliers and a mallet to cut and remove bone from the ventral facet. Straight and articulating endoscopic drills, Kerrison rongeurs, and surgical lasers or other innovative endoscopic tools aided the surgical procedure. Endoscopic instruments such as drills and rongeurs were deployed through the working cannula without the endoscope or through the inner working channel of the endoscope. During these maneuvers, the exiting nerve root was carefully retracted to minimize the risk of postoperative dysesthesia due to irritation of the dorsal root ganglion (DRG). Gradual enlarging the decompression from the center of the cannula outward with this type of visualized serial dilation and decompression. The decompression was typically performed under continuous direct video endoscopic visualization. The compressive pathology was removed by aiming the instruments at until the target pain generator was sufficiently decompressed during the foraminoplasty. This would mean visualizing both the traversing and exiting nerve by decompressing the hidden zone of the axilla. The “inside-out” technique allowed straightforward decompression of contained herniations. Extruded disc herniations were removed through a small annular window from the disc annulus or foramen. This technique often relieved contralateral sciatica by decompressing the disc intradiscally. The tip of the SAP was frequently removed with a laser which was introduced via a glass fiber through the central working channel of the endoscope. The laser was also used when necessary to remove disc tissue embedded within the annulus.
Surgical steps of the outside-in techniques
Patients with symptomatic foraminal stenosis were treated with by employing the transforaminal approach in prone position under local anesthesia and sedation and under intermittent video endoscopic visualization. Patients were treated following the outside-in technique which calls for advancing the working sheath into the safe zone of Kambin’s triangle within the neuroforamen bordered by the traversing nerve root medially, the exiting nerve root laterally, and the lower adjacent pedicle distally (10,22). This crucial initial maneuver aided in the retraction of the exiting nerve root. Hoogland’s original technique depended on serial dilation with percutaneous trephines, endoscopic rasps, osteotomes, motorized drills, Kerrison rongeurs, and many of the instrumentation developed by endoscopic companies. Percutaneous trephines were employed using manually controlled T-handles, but evolved as new instruments were developed. Visualization later mimicked the YESSTMinside out philosophy. The neuroforaminal volume was increased by removing bone from the ventral surface of the SAP and the inferior articular process (IAP) with instruments introduced through the inner 4.1 mm working channel of the spinal endoscope (Figure 4). The upward migrated tip of the (SAP) was resected starting rostral to distal via osteotomy from the axilla of the exiting nerve root. In some cases of advanced disc degeneration with near complete vertical collapse, the foraminoplasty was expanded by the addition of partial pedicle resection. The discectomy was commenced after completion of the foraminoplasty without entering the intervertebral disc space with the endoscope or its working sheath. Ultimately the decompressed targeted patho-anatomy determined the success of the procedure.
Correlation of imaging to clinical presentation
Patients were counseled to consider other types of surgery if there was radiographic evidence of fractures due to trauma, or osteoporosis and greater than grade I spondylolisthesis, reduced posterior disc height due to advanced degenerative disc disease, excessive spinal deformity, pars defects, and other indicators of subclinical instability including facet hypertrophy and osteophytosis. Advanced imaging modalities including MRI CT were evaluated for lateral recess stenosis. CT myelography was assessed whenever available as the best measure of central and lateral canal due to any extradural cause of neural compression. It was ordered for patients with suspected dynamic stenosis, postoperative leg pain, severe scoliosis or spondylolisthesis, metallic implants, other contraindications to MRI, and, most importantly, in patients with lower extremity symptoms in the absence of plausible MRI findings (3,23). Central and lateral recess stenosis was assessed on midline T2-sagittal and axial images. Neuroforaminal height of less than 15 mm and width of less than 3 mm and a reduced posterior height of the intervertebral disc of less than 3 mm were considered indicators of symptomatic spinal stenosis in more than 80% of patients (12). Foraminal anatomy was best assessed on sagittal T1-weighted images. Prognosticators of neuroforaminal stenosis were the absence of normal fat around the root. Axial T1-weighted images were assessed for extraforaminal stenosis by checking for obliteration of the regular interval of fat between the disc and nerve root. Advanced imaging studies were carefully correlated with the response to diagnostic and therapeutic injections. The combination of these preoperative diagnostic tests have been found to be more accurate prognosticators of successful clinical outcomes following the endoscopic transforaminal decompression as MRI imaging may underestimate the degree of stenosis and soft tissue impingement causing the patients symptoms.
Clinical follow-up & outcome analysis
At five years postoperatively, primary clinical outcomes measures for patients who underwent the inside out and outside-in technique were assessed using modified Macnab criteria (24). Postoperative imaging studies were scrutinized for instability, recurrent stenosis at the index level in patients with fair and poor Macnab outcomes. Visual analog scale (VAS) scores were obtained preoperatively (preop VAS), within the immediate postoperative period (postop VAS), and at final follow-up (last F/U VAS) (25). Two-tailed t-test, ANOVA testing, and cross-tabulation statistics and measures of association were computed for two-way tables using IBM SPSS Statistics software, Version 25.0. Descriptive statistic measures were used to calculate the mean, range, and standard deviation as well as percentages. Cross tabulation methods were used to assess for any statistically significant association between variables by employing the Pearson chi-square and Fisher’s exact test as statistical measures of association. Expected cell counts, continuity corrections, and likelihood ratios were calculated for some analyses.
Results
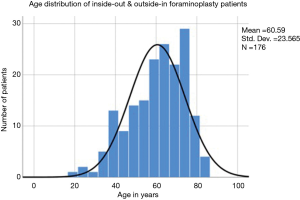
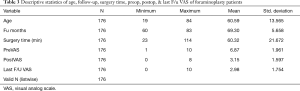
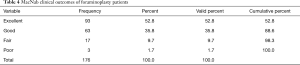
The age distribution of our patient population was normal (Figure 5). The average age was 60.59 years [standard deviation (STD) 13.57 years] with the youngest patient being 19 years of age and the oldest patient 84 years, respectively. The mean follow-up was 69. 3 months ranging from 60 to 83 months (Tables 3,4). As shown in Table 2, the most common surgical level for the index SED™ procedure was L4/5 (38.1%) followed by L5/S1 (17.6%), and by unilateral two-level surgery L4–S1 (17.6%). At minimum 5-year follow-up, excellent results according to the Macnab criteria were obtained in 93 (52.8%) patients, good in 63 (35.8%), fair in 17 (9.7%), and poor in 3 (1.7%), respectively (Tables 3,4). The mean preoperative VAS was 6.87±1.96. The mean postoperative VAS was 3.15±1.59 and 2.98±1.75 at last follow-up, respectively. Both postoperative VAS and last follow-up VAS were statistically reduced at a significance level of P<0001 (Tables 3,4).
Full table
Full table
There were no major approach-, surgical- or anesthesia-related complications in this series. The vast majority of patients (112/176; 63.6% of the study population) did not require any additional interventional or surgical treatment following the index SED™. Postoperative dysesthesia due to irritation of the DRG occurred in 17 patients (9.7%) and was the most common benign postoperative sequelae (an unavoidable side effect of an otherwise expertly executed surgery; Table 5). It was managed with activity modification, gabapentin or pregabalin, and transforaminal epidural steroid injections. Most patient’s DRG irritation resolved with these supportive care measures within 2 to 3 weeks. Occasionally a longer recovery period was required when there were severe comorbities. In the inside-out group, there were 9 (5.1%) patients with recurrent disc herniations versus none in the outside-in group. One inside-out patient had an incidental postoperative hematoma which required no surgical treatment. The patient was treated with aspiration if the hematoma and a TESI. No other complications were observed in the immediate postoperative period (90 days). In the inside-out group, very few additional problems occurred postoperatively. These included persistent pain in 3 patients due to the inability to complete the decompression endoscopically with failure to cure. Another 2 patients developed pain at another level several years later. Nine (5.1%) outside-in patients experienced recurrence of pain due to the natural progression of the degenerative disease process (Table 5).

Full table
Additional postoperative treatments were done on 30 of the 86 (34.9%) inside-out patients postoperatively. Most of them (23 patients) were treated with TESI postoperatively to diminish their symptoms. Three of the 9 patients with recurrent HNP opted for another SED™. One patient underwent L3/4 fusion and another patient an L3–L5 fusion at the index levels of their respective endoscopic foraminoplasty. An additional patient required a postoperative hemilaminectomy at the index level to control his symptoms, and yet another patient underwent a foraminotomy at another than the index level (Table 5). In the outside-in group, additional surgeries were done in 32 (35.6%) of the 90 patients. Development of axial back pain after SED™ prompted additional surgery at an average of 22.57 months postoperatively (7/90; 7.8%). This was followed by recurrence of familiar pain from the same surgical level (9/90; 10%), development of sciatica type back and leg pain on the opposite side but from the same surgical level (8/90; 8.9%), and pain from a different adjacent level (7/90; 7.8%), respectively. One additional patient underwent ablation of his painful sacroiliac (SI) joint at 73 months following the index SED™ (1/90; 1.1%).
Cross-tabulation of long-term outcomes versus additional intervention (Table 6) showed that patients, who initially rated their VAS scores and Macnab outcomes favorably, also did so at final follow-up in spite of some of them requiring additional intervention or surgery throughout their entire follow-up period. In the inside-out group, the 55 patients without any need for additional intervention (55/86) and the 24 patients with DRG irritation, who were successfully treated with TESI and did not require any additional surgery throughout the follow up period, totaled a 91.9% portion of the inside-out patient group who did not receive any additional surgery following the index SED™. In the outside-in group, the 50 patients without any need for additional intervention (50/90) and the 8 patients with DRG irritation, who were successfully treated with TESI and did not require any additional surgery throughout the follow up period, totaled a 64.4% portion of the entire patient population who did not receive any additional surgery following the index decompression. In the inside-out group, functional outcomes reported at long-term 5-year follow-up were not affected by the need for additional surgeries at a statistically significant level.

Full table
In the outside-in group, however, long-term clinical outcome data were favorably affected by follow-up interventional and surgical treatments at a statistically significant level (P<0.0001; Table 6). The majority of the additional surgeries (26/32; 81.25%) being performed on patients who ultimately rated their outcome as excellent and good. Only 5 of the 61 patients (5.5% of 90) with excellent results opted for more surgery with 2 patients undergoing SED™ on the opposite side at the same level, another 2 patients undergoing same level TLIF, and 1 patient being treated with a laminectomy. The latter 3 patients underwent surgery for the progression of the degenerative disease process. Another 6 patients who reported fair long-term outcomes developed pain from adjacent segment disease (2 patients), recurrent pain from the same level (1 patient), and pain from the opposite side of the same surgical level (3 patients). The majority of patients (21/90; 23.3%) who opted for additional surgery within the minimum 5-year follow-up period rated their long-term 5-year Macnab outcomes as good.
While most of the follow-up surgeries (23/32) following outside-in SED™ were additional endoscopic decompressions and rhizotomies (24/32; 75%) non-fusion procedures, only 8 of the whole study series of 90 patients (8.9%) underwent fusion after index SED™ during the minimum 5-year follow-up period. One patient opted for an open laminectomy (1.1%). This higher reoperation rate at the index level (20%; 18/90 patients) with either an opposite side same level SED™ (8 patients), same level fusions (6 TLIF and 2 ALIF patients), same level and side SED™ (1 patient), and same level laminectomy (1 patient) was statistically significantly higher in the outside-in group than in the inside-out group (P<0.001), where aggressive open surgeries were performed in only 3 patients with 2 of them having been treated with a fusion (2.3% fusion rate). In comparison, a higher fusion rate was observed in the outside-in group with 8 patients having been treated with fusion (8.9% fusion rate).
Discussion
This study aimed at assessing long-term outcomes and reoperation rates in patients who underwent endoscopic transforaminal decompression for foraminal spinal stenosis. Favorable long-term clinical results with this study’s primary outcome measure in the majority of patients. The authors employed two conceptually different transforaminal decompression methodologies—the inside-out YESS™ technique (1-6) and a modified outside-in technique originally popularized by Hoogland et al. (7) During the inside-out decompression (group 1 patients), the working cannula is initially placed to obtain access inside the disc for intradiscal therapy, thus, protecting the exiting nerve root and its DRG from manipulation and irritation. During the outside-in decompression, the working cannula is not placed inside the intervertebral disc. The modified technique employed in the outside-in patients of this study (group 2) consisted of an initial foraminoplasty under direct visualization with a motorized power drill passed through the inner working channel of the spinal endoscope instead of the non-visualized use of percutaneous cannulated reamers or trephines over a guidewire as called for by the contemporary TESSYS® technique (26). This modification was indented to lower the risk of forceful injury to the facet joint complex or the nerve roots observed in some patients due to the sharp trephines’ cutting teeth (27).
Age-related degeneration of the lumbar spine and of the intervertebral disc in particular may produce instability of the spinal motion segment. Radiographic prognosticators of hypermobility include thickening of the ligamentum flavum and soft tissues in the foramen, as well as hypertrophy of the facet joints. Enlargement and upward migration of the SAP is frequently encountered (10,28,29). Subjective symptoms reported by patients include numbness, intermittent claudication and weakness from increased activity and exertion. Painful irritations become increasingly bothersome and then debilitating. In spite of having these symptoms, patients are often caught up in the controversy on appropriate surgical indications and the best timing of surgical intervention for lumbar foraminal stenosis that does not respond favorably to standard non-operative and supportive care measures. Inaccuracies in the preoperative advanced imaging reporting may also contribute to delays of effective treatments (23) and contribute to entrapping patients in repetitive referral cycles to physical therapy or pain management.
Patient selection is crucial for successful outcome with either of the two decompression techniques. Therefore, considering additional information from diagnostic and therapeutic injections using Yeung’s surgical trajectories to perform foraminal epidurograms and discography is crucial to determine the source of the patient’s pain. This diagnostic information from diagnostic and therapeutic injection technique provided additional clinical information to augment clinical diagnosis correlated with traditional imaging such as CT scans, X-rays, and MRI (17,23). This concept of an integrative diagnostic preoperative work-up has withstood the test of time and has been applied by the authors and all affiliated surgeons in Yeung’s. With these use of these inclusion/exclusion criteria, patients who meet traditional criteria for translaminar decompression or fusion such as degenerative spondylolisthesis or isthmic spondylolisthesis were advised that these conditions were good indications for translaminar decompression and fusion, but less invasive alternatives were also discussed with the patient to arrive at a shared decision between patient and surgeon.
This comparative study between two different endoscopic transforaminal decompression techniques was motivated by the need to investigate what happens to patients in the long run who underwent transforaminal treatment of symptomatic foraminal stenosis and lateral recess stenosis by either method. Other important associated questions revolved around what type of planned and unplanned surgical and non-surgical aftercare, if any, was necessary to treat any shortcomings of the procedure and what was the longevity of the treatment effect as defined by the ultimate goal of avoiding spinal fusion five years after the initial endoscopic index procedure? In short, the authors attempted to define any long-term differences in clinical outcomes with inside-out versus outside-in endoscopic transforaminal decompression—a discussion that is highly relevant in the context of the appropriate choice of initial procedure to treat sciatica-type low back and leg pain. While this discussion may seem trivial on the surface, the authors argue that it is far from it. There are profound differences between the inside-out and outside-in endoscopic decompression techniques. For example, the initial placement of the working cannula into the intervertebral disc during the inside-out technique may protect the exiting nerve root and perhaps simplify the discectomy procedure and shorten the initial learning curve but could provoke postoperative disc collapse. On the other hand, the lack of intradiscal visualization during the outside-in endoscopic decompression may preclude treatment of painful conditions best visualized and treated from within the intervertebral disc. For example, annular tears and contained herniated discs maybe amenable to intradiscal therapies including direct mechanical and indirect radiofrequency decompression and tissue modulation. Furthermore, the inside-out technique visualizes painful abnormalities in the hidden zone of Macnab underneath the dural sack when retracting the working cannula that are simply not visualized with the outside-in technique since the entire outside-in decompression procedure takes place more lateral and posterior. These perceived shortcomings of both procedures were at the heart of this clinical investigation.
Results of this study showed that 88.6% of patients were rated to have excellent (52.8%) and good (35.8%) outcomes using Macnab standardized outcome criteria at five-year follow-up. The VAS reductions were also statistically significant (P<0.0001) both immediately postoperatively and at final follow-up. Nearly two-thirds of the study population (63.6%) did not require any additional intervention following their endoscopic transforaminal foraminoplasty regardless of whether it was carried out with the inside-out or the outside-in technique. Approximately one-third (36.4%) had some unintended aftercare postoperatively which was not automatically associated with fair or poor outcomes (Table 6). The majority of unintended aftercare was delivered to patients with excellent and good outcomes (34/176 patients). The rate of additional postoperative treatment was similar between the inside-out (34.9%), and the outside-in group (35.6%) patients. The rate of postoperative DRG irritation was also similar between the inside-out (10.5%) and outside-in (8.9%) group. The difference between these calculated rates did not reach statistical significance. Hence, much of the unintended aftercare was due to benign transitory postoperative DRG irritation or postoperative pain which was managed successfully with TESI.
While the long-term outcomes with endoscopic transforaminal foraminoplasty regardless of technique are similar to outcomes reported with microdiscectomy or laminectomy (9,21), there were some substantial differences in the types of postoperative complications and sequelae between the two groups of patients. There were 9 patients with recurrent disc herniations in the inside-out group (10.5%) versus none in the outside-in group. This recurrence rate in the inside-out group was higher than the published rate of around 5% with traditional microdiscectomy but not unusual considering the advanced degree of disc degeneration of patients in the inside-out group (10,22,24). Many of the outside-in patients also had advanced disc degeneration. Recurrent disc bulges and herniations may have been less clinically relevant and perhaps asymptomatic due to the extensive foraminoplasty with partial resection of the SAP routinely performed during the outside-in decompression. Compared to established complication rates (30-36) with open lumbar spine surgery or other forms of translaminar or transforaminal minimally invasive spinal surgery there were no significant postoperative complications.
Perhaps the most significant limitation of this retrospective study may have been the impact of affective (unconscious emotional reaction) and cognitive (distortions of thinking) biases in the clinical diagnostic and surgical decision-making process (37,38). Cognitive biases, such as hindsight or outcome bias, are virtually unavoidable in retrospective studies as knowledge of the clinical outcome by the surgeon has been recognized to inflate the predictability of an event after it happened (39-41). Hindsight cognitive biases may have been less relevant since the individual patient-specific pain generators ascertained during awake intraoperative evaluation under local anesthesia were not known throughout the 7-year study period. Intuition bias (40) may have played a role in patient selection for surgery after the initial learning curve.
This long-term follow-up study shows that patients who opted for additional surgery at other levels or on the opposite side of the same surgical level, may have multiple pain generators within one motion segment or may develop new ones in follow-up due to progression of the degenerative disease process that can influence clinical outcomes. Therefore, the staged management of degenerative lumbar disease on the basis of the patient’s leading symptoms which are painful at the time when the care is delivered appears to be more appropriate. Often, the surgical plan is based X-rays and MRI findings. Endoscopic visualization of the patient’s lumbar foraminal anatomy, whether a variation of normal or abnormal, needs to be evaluated intraoperatively as to whether it causes pain and then be correlated with preoperative imaging studies and treated accordingly during the decompression procedure (4-6,16). The initial foraminoplasty during the outside-in decompression with power drills was intended to merely create a safe space for the working sheath to be placed in by facing the lateral aspect of the facet joint complex at the beginning of the surgery before advancing into Kambin’s triangle (41,42). The author considered this a way of assuring that the intraforaminal anatomy is not distorted or destroyed, as is possible during the fluoroscopically guided drilling or reaming called for by the TESSYS® method (26), before such real-time intraoperative evocative evaluation of pain generators in the awake patient has been completed. Mechanical compression of the exiting or traversing nerve root created by a herniated disc or bony obstruction of the neuroforamen is common problems but other pain generators may exist (4-6). This study was limited in its statistical power to further analyze the impact of individual pain generators including the rostral migration of the cranial tip of the SAP into the axilla of the exiting nerve root, hypertrophy of the transverse process and pars interarticularis, soft tissues impingement caused by hypertrophy of the ligament flavum and facet cysts or by apophyseal ring osteophytes of the upper vertebral body within the axilla of the exiting root, and the impact of nerve root tethering and chronic inflammation of the DRG caused by far lateral extraforaminal disc herniations.
While the distinction between the outside-in and the inside-out techniques for the foraminoplasty discussion may seem academic on the surface, to those who practice endoscopic spine surgery at the highest level, it is far from it. This long-term clinical outcome study on the utility of the inside-out and the outside-in transforaminal decompression provides additional insights on how the clinical course of degenerative lumbar spinal stenosis may be affected by the selection of either endoscopic decompression technique. The many distinct procedural steps between these two techniques, their pros and cons, and how the skilled endoscopic spine surgeon may apply them to benefit her/his patient by avoiding pitfalls and by capitalizing on advantages that ultimately may play out in short- and long-term follow-up have been illustrated by this study. With both authors executing the inside-out and outside-in decompression and foraminoplasty techniques for stenosis at the highest skill level it became clear that the overall additional surgery rate with the inside-out patients (group 1) was lower than in the outside-in patients (group 2). Of particular interest in this discussion is the need for additional surgery at the same index level but on the opposite side. The lack of intradiscal visualization and treatment with the outside-in technique could have resulted in incomplete treatment of the degenerative disease process of the intervertebral disc which ultimately may have contributed to higher reoperation (8.1% inside-out versus 35.6% outside-in) and fusion (2.3% inside-out versus 8.9% outside-in) rate in the outside-in group. Ultimately, the long-term clinical outcomes with the endoscopic transforaminal decompression procedure were favorable regardless of whether the inside-out or outside-in technique was used. In comparison to published 5-year reoperation rates for decompression/fusion of 18.4% (43,44), only 5.7% of patients of this study required a secondary fusion to continue to manage their symptoms—a 3.2-fold decrease.
Conclusions
Patients with symptomatic foraminal stenosis can be treated favorably either with the inside-out or the outside-in transforaminal decompression technique. Direct access to the stenotic neuroforamen with the endoscopic transforaminal approach and its low propensity to destabilize the lumbar spinal motion segment forms the basis for low reoperation and secondary fusion rates. The reoperation rates due to same level problems may be slightly higher with the outside-in technique since intradiscal pain generators are neither directly visualized nor treated. These unconventional endoscopic spinal surgery concepts may continue not to be well recognized by traditionally trained surgeons unless validated with high-grade clinical studies.
Acknowledgments
None.
Footnote
Conflicts of Interest: First author designed and trademarked his inside-out YESS™ technique and receives royalties from the sale of his inventions), Indirect conflicts of interest (honoraria, consultancies to sponsoring organizations, is donated to IITS.org, a 501c 3 organization). The second author has no direct or indirect conflicts. This manuscript is not meant for or intended to endorse any products or push any other agenda other than the associated clinical outcomes with lumbar endoscopic foraminoplasty. The motive for compiling this clinically relevant information is by no means created and/or correlated to directly enrich anyone due to its publication. This publication was intended to substantiate contemporary endoscopic spinal surgery concepts to facilitate technology advancements.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patients in this consecutive case series provided informed consent and IRB approval was obtained (CEIFUS 106-19).
References
- Yeung A, Roberts A, Zhu L, et al. Treatment of Soft Tissue and Bony Spinal Stenosis by a Visualized Endoscopic Transforaminal Technique Under Local Anesthesia. Neurospine 2019;16:52-62. [Crossref] [PubMed]
- Yeung AT. Endoscopic Decompression, Foraminal-plasty and Dorsal Rhizotomy for Foraminal Stenosis and Lumbar Spondylosis: A Hybrid Procedure in Lieu of Fusion. J Neurol Disord 2016;4:322. [Crossref]
- Yeung A, Yeung CA. Endoscopic Identification and Treating the Pain Generators in the Lumbar Spine that Escape Detection by Traditional Imaging Studies. J Spine 2017;6:369.
- Yeung AT. In-vivo Endoscopic Visualization of Pain Generators in the Lumbar Spine. J Spine 2017;6:385. [Crossref]
- Yeung AT. The Yeung Percutaneous Endoscopic Lumbar Decompressive Technique (YESSTM). J Spine 2018;7:408. [Crossref]
- Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722-31. [Crossref] [PubMed]
- Hoogland T. Percutaneous endoscopic discectomy. J Neurosurg 1993;79:967-8. [PubMed]
- Lewandrowski KU. “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: a retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg 2014.8. [PubMed]
- Sengupta DK, Herkowitz HN. Lumbar spinal stenosis. Treatment strategies and indications for surgery. Orthop Clin North Am 2003;34:281-95. [Crossref] [PubMed]
- Rauschning W. Normal and pathologic anatomy of the lumbar root canals. Spine (Phila Pa 1976) 1987;12:1008-19. [Crossref] [PubMed]
- Lee CK, Rauschning W, Glenn W. Lateral lumbar spinal canal stenosis: classification, pathologic anatomy and surgical decompression. Spine (Phila Pa 1976) 1988;13:313-20. [Crossref] [PubMed]
- Hasegawa T, An HS, Haughton VM, et al. Lumbar foraminal stenosis: critical heights of the intervertebral discs and foramina. A cryomicrotome study in cadavera. J Bone Joint Surg Am 1995;77:32-8. [Crossref] [PubMed]
- Kirkaldy-Willis WH, Wedge JH, et al. Lumbar spinal nerve lateral entrapment. Clin Orthop Relat Res 1982.171-8. [PubMed]
- Jenis LG, An HS. Spine update: lumbar foraminal stenosis. Spine (Phila Pa 1976) 2000;25:389-94. [Crossref] [PubMed]
- el-Khoury GY, Ehara S, Weinstein JN, et al. Epidural steroid injection: a procedure ideally performed with fluoroscopic control. Radiology 1988;168:554-7. [Crossref] [PubMed]
- Yeung AT. Failed Back Surgery Syndrome: Endoscopic Documentation of Common Causes by visualization of Painful Patho-anatomy in the hidden zone of the axilla containing the Dorsal Root Ganglion and Salvage treatment of Neuropathic pain with DRG neuromodulation. SF J Neuro Sci 2017;1:1.
- Lewandrowski KU. Successful outcome after outpatient transforaminal decompression for lumbar foraminal and lateral recess stenosis: The positive predictive value of diagnostic epidural steroid injection. Clinical Neurology and Neurosurgery 2018;173:38-45. [Crossref] [PubMed]
- Botwin KP, Gruber RD, Bouchlas CG, et al. Fluoroscopically guided lumbar transforaminal epidural steroid injections in degenerative lumbar stenosis. Am J Phys Med Rehabil 2002;81:898-905. [Crossref] [PubMed]
- Bogduk N, Aprill C, Derby R. Epidural spinal injections. In: White AH, Schollerman J. editors. Spinal Care: Diagnosis and Treatment. St Louis: Mosby, 1995:322-43.
- Nordby EJ, Wright PH. Efficacy of chymopapain in chemonucleolysis. A review. Spine (Phila Pa 1976) 1994;19:2578-83. [Crossref] [PubMed]
- Hoogland T, Schubert M, Miklitz B, et al. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31:E890-7. [Crossref] [PubMed]
- Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg 2002;96:34-44. [PubMed]
- Yeung AT, Lewandrowski KU. Retrospective analysis of accuracy and positive predictive value of preoperative lumbar MRI grading after successful outcome following outpatient endoscopic decompression for lumbar foraminal and lateral recess stenosis. Clin Neurol Neurosurg 2019;181:52. [Crossref] [PubMed]
- Macnab I. Negative disc exploration: An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]
- Huskisson EC, Jones J, Scott PJ. Application of visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976;15:185-7. [Crossref] [PubMed]
- Jasper GP, Francisco GM, Aghion D, et al. Technical considerations in transforaminal endoscopic discectomy with foraminoplasty for the treatment of spondylolisthesis: Case report. Clin Neurol Neurosurg 2014;119:84-7. [Crossref] [PubMed]
- Li ZZ, Hou SX, Shang WL, et al. Modified Percutaneous Lumbar Foraminoplasty and Percutaneous Endoscopic Lumbar Discectomy: Instrument Design, Technique Notes, and 5 Years Follow-up. Pain Physician 2017;20:E85-98. [Crossref] [PubMed]
- Holm S. Pathophysiology of disc degeneration. Acta Orthop Scand Suppl 1993;251:13-5. [Crossref] [PubMed]
- Rauschning W. Pathoanatomy of lumbar disc degeneration and stenosis. Acta Orthop Scand Suppl 1993;251:3-12. [Crossref] [PubMed]
- O’Lynnger TM, Zuckerman SL, Morone PJ, et al. Trends for Spine Surgery for the Elderly: Implications for Access to Healthcare in North America. Neurosurgery 2015;77 Suppl 4:S136-41. [Crossref] [PubMed]
- Hernandez-Perez PA, Prinzo-Yamurri H. Analysis of the lumbar discectomy complications. Article in Spanish. Neurocirugia (Astur) 2005;16:419-26. [PubMed]
- Lewandrowski KU. Incidence, Management, and Cost of Complications After Transforaminal Endoscopic Decompression Surgery for Lumbar Foraminal and Lateral Recess Stenosis: A Value Proposition for Outpatient Ambulatory Surgery. Int J Spine Surg 2019;13:53-67. [Crossref] [PubMed]
- Ramirez LF, Thisted R. Complications and demographic characteristics of patients undergoing lumbar discectomy in community hospitals. Neurosurgery 1989;25:226-30; discussion 230-1. [Crossref] [PubMed]
- Tafazal SI, Sell PJ. Incidental durotomy in lumbar spine surgery: incidence and management. Eur Spine J 2005;14:287-90. [Crossref] [PubMed]
- Kraemer R, Wild A, Haak H, et al. Classification and management of early complications in open lumbar microdiscectomy. Eur Spine J 2003;12:239-46. [Crossref] [PubMed]
- Schizas C, Neumayer F, Kosmopoulos V. Incidence and management of pulmonary embolism following spinal surgery occurring while under chemical thromboprophylaxis. Eur Spine J 2008;17:970-4. [Crossref] [PubMed]
- Bakeman R, Quera V, McArthur D, et al. Detecting sequential patterns and determining their reliability with fallible observers. Psychological Methods 1997;2:357-70. [Crossref]
- Sibbald M, Cavalcanti RB. The biasing effect of clinical history on physical examination diagnostic accuracy. Med Educ 2011;45:827-34. [Crossref] [PubMed]
- Zwaan L, Monteiro S, Sherbino J, et al. Is bias in the eye of the beholder? A vignette study to assess recognition of cognitive biases in clinical case workups. BMJ Qual Saf 2017;26:104-10. [Crossref] [PubMed]
- Henriksen K, Kaplan H. Hindsight bias, outcome knowledge and adaptive learning. Qual Saf Health Care 2003;12 Suppl 2:ii46-50. [Crossref] [PubMed]
- Kambin P, Casey K, O’Brien E, et al. Transforaminal arthroscopic decompression of lateral recess stenosis. J Neurosurg 1996;84:462-7. [Crossref] [PubMed]
- Kambin P, O’Brien E, Zhou L, et al. Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop Relat Res 1998.150-67. [PubMed]
- Hugh TB, Tracy GD. Hindsight bias in medicolegal expert reports. Med J Aust 2002;176:277-8. [Crossref] [PubMed]
- Kuo CC, Merchant M, Kardile MP, et al. In Degenerative Spondylolisthesis, Unilateral Laminotomy for Bilateral Decompression Leads to Less Reoperations at 5 Years When Compared to Posterior Decompression with Instrumented Fusion: A Propensity Matched Retrospective Analysis. Spine (Phila Pa 1976) 2019. [Epub ahead of print]. [Crossref] [PubMed]


