
Routine perioperative practices and postoperative outcomes for elective lumbar laminectomies
Introduction
With increasing expenditures and growing demands in a publicly-funded health care system, attention has focused on the issue of low-value health care services. Campaigns such as Choosing Wisely Canada have been implemented to help clinicians and patients avoid unnecessary tests and treatments (1). This physician-led campaign has developed lists of test and treatments that are commonly used but not supported by evidence.
Among these practices, and relevant to the care of the perioperative patient, is the routine use of baseline laboratory studies for asymptomatic patients undergoing low-risk, non-cardiac surgery (2). The Canadian Anesthesiologists’ Society guidelines state that laboratory testing should not be performed on a routine basis and only obtained when results will change perioperative management (3). In this setting, abnormal test results rarely influence management and do not improve clinical outcomes (4,5). A randomized controlled trial in an ambulatory surgery population, which included patients undergoing spine surgery among other surgical procedures, demonstrated no difference in intraoperative and postoperative outcomes for patients with and without preoperative testing (6). Similar findings have been reported in patients undergoing cataract surgery (7). Despite the growing evidence that routine preoperative bloodwork has little utility for patients undergoing low-risk surgeries, institutions across Ontario, Canada, still order these types of investigations with varying frequency (8).
Elective lumbar laminectomy is a low-risk procedure for spinal stenosis that is often performed as ambulatory surgery, with patients being discharged home after a short period of monitoring. Few studies have evaluated the utility of preoperative bloodwork for elective lumbar laminectomy. The published literature to date suggests that bloodwork may be safely disregarded (9,10). Still, these investigations have been routinely ordered for patients in our facilities. Identification of current practices is essential to determining where system improvements can be made. Our goal was to identify perioperative practices that have little utility for elective lumbar laminectomies.
The primary purpose of this study was to describe the prevalence and types of preoperative bloodwork testing for patients undergoing elective lumbar laminectomy and to determine whether preoperative bloodwork was associated with intraoperative and postoperative complications. Secondary objectives were to describe the prevalence of intraoperative tranexamic acid administration, hospital length of stay, and 30-day readmission.
Methods
Patients & setting
This retrospective cohort study included all patients 18 years of age and older who underwent elective lumbar laminectomy (one or more levels) for spinal stenosis by one orthopaedic spine surgeon (DY) between July 01, 2013 and July 30, 2017. All procedures were performed at the university-affiliated inpatient hospital or ambulatory care hospital. At the time of surgical booking, the primary surgeon selected the most appropriate facility for each patient according to his/her medical history and perioperative risk. Medically-fit patients without significant comorbidities underwent surgery at the ambulatory care hospital, which supports outpatient and short-stay (<24 hours) procedures, while higher risk patients underwent surgery at the inpatient hospital. Patients undergoing a lumbar spine procedure for fracture or pre-existing infection, pseudarthrosis, malignancy, or scoliosis were excluded. None of the patients underwent an associated spinal fusion. The clinical criteria for blood transfusion included symptomatic anemia with any of the following signs or symptoms: tachycardia, hypotension, angina, dyspnea, and/or syncope.
If a patient had multiple lumbar laminectomies on different dates during the study period, only the first spine procedure was included. Patients who were booked for elective lumbar laminectomy but did not undergo surgery due to cancellation were reviewed separately. The study was approved by the University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board.
Data collection
A retrospective electronic chart review was conducted. Data on baseline patient characteristics, preoperative and postoperative bloodwork investigations, blood transfusion, surgical details, hospital length of stay, and 30-day readmission were collected. Preoperative bloodwork was defined as any bloodwork that was collected less than 30 days prior to surgical date and was not associated with a hospital admission or routine follow-up appointment for another diagnosis. The following surgical details were collected: number of operative levels of the lumbar spine, surgical approach, duration of surgery, estimated blood loss, and tranexamic acid use. Due to small sample sizes, an aggregate for intraoperative complication was created, which included intraoperative blood transfusion and dural tears requiring surgical repair. Any complication in the intraoperative or postoperative records was collected. Furthermore, all surgical follow-up notes were reviewed for details about potential complications.
For patients whose surgeries were cancelled, data on patient demographics and preoperative investigations was collected whenever available.
Statistical analysis
Differences between groups were compared using the Wilcoxon-Mann Whitney test and two-sample independent t-test, when appropriate. All statistical analyses were performed using Statistical Analysis Software (SAS version 9.4).
Results
Baseline characteristics
A total of 256 patients underwent elective lumbar laminectomy of one or more levels by a single orthopaedic spine surgeon (DY) during the study period. One patient had two eligible procedures during the study period; only the first procedure was included. The average patient age was 66.7±9.77 (SD) years old, and 55.9% were male (Table 1). All patients had at least one postoperative visit with the surgeon. There were five surgical cancellations during the study period.
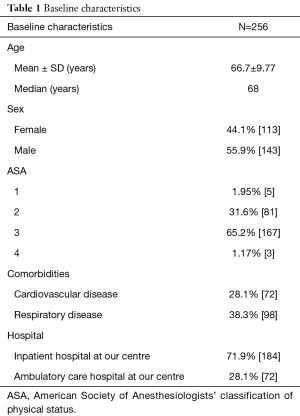
Full table
Preoperative investigations and cancellations
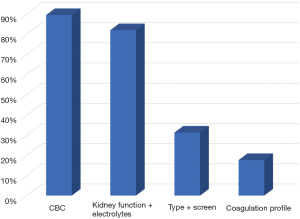
At least one preoperative bloodwork investigation was ordered in 89.5% of patients. The most commonly-ordered preoperative investigations are shown in Figure 1 and include: 89.5% complete blood count, 82.0% electrolytes and kidney function tests, 31.3% type and screen, and 17.6% coagulation profile testing. Presence of preoperative bloodwork was not associated with hospital length of stay after surgery (P=0.99). Of those whose surgeries were cancelled, fewer than five patients had preoperative bloodwork prior to cancellation; no major bloodwork abnormalities were identified in this group.
Operative details and postoperative findings
Operative details and postoperative findings are shown in Table 2. Most patients underwent laminectomy at either two or three levels of the lumbar spine (46.48% and 31.64%, respectively). Duration of surgery was, on average, 153.87±36.51 minutes and did not differ significantly based on number of operative levels (P=0.62). Estimated blood loss was 97.11±111.69 mL. Less than 2% of patients received intraoperative intravenous tranexamic acid. A composite of surgical complications, including intraoperative blood transfusion and dural tear requiring surgical repair, occurred in 2.34% of cases. Patients were typically discharged home on the day of surgery (35.9%), or on postoperative day 1 (52.7%). No patient received a postoperative blood transfusion. In the 30 days following surgery, there were no hospital readmissions.
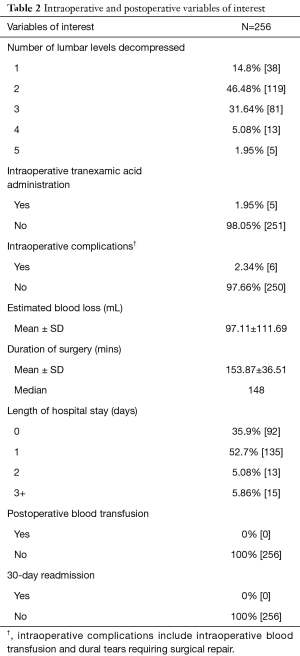
Full table
Discussion
We measured the prevalence and types of preoperative bloodwork completed in our centres prior to elective lumbar laminectomy and compared these to rates of postoperative complications and blood transfusion. This is the largest study to date looking at the utility of preoperative testing in elective lumbar laminectomies.
We demonstrated that blood transfusion in the context of elective lumbar laminectomy is rare. Our findings are in keeping with existing literature, which suggests that given the low risk of transfusion for this procedure, it would be safe to discontinue preoperative type and screen (9,10).
With respect to other bloodwork, it has been shown that neither preoperative blood testing, nor abnormal test results, are associated with postoperative complications (11). Similar findings have been reported for elective pediatric spinal cases (12). Given low complication and transfusion rates, we felt that evaluation of the statistical association between preoperative bloodwork and postoperative complications was of little value. However, the low perioperative and postoperative complication rates are reassuring and reinforce the hypothesis that routine preoperative bloodwork does not affect perioperative care and outcomes.
We completed a chart review on patients who were booked for elective lumbar laminectomy, but their surgeries were cancelled. There were five cancellations over the study period. This proportion is similar to the proportion of cancellations in related literature (6). We did not compare preoperative testing between completed and cancelled cases for a number of reasons. First, the number of cancellations was low. Second, some cancelled patients had no preoperative bloodwork. Third, we were not able to identify the reason for cancellation in most cases. Still, the low proportion of cancellations is reassuring.
There is substantial inter-institution variation in utilization of routine preoperative investigations (13). Some hospitals have pre-specified investigations that are ordered prior to each elective surgical procedure. Existing policies should be re-evaluated in light of evidence from this study and similar studies that suggest little utility in routine bloodwork prior to elective lumbar laminectomy.
Use of intraoperative, intravenous tranexamic acid among our patients was low. The literature suggests that tranexamic acid decreases intraoperative and postoperative blood loss in complex spine surgery with expected significant blood loss (14-17). In our study, however, blood loss estimates were, on average, <100 mL, and blood transfusion risk was extremely low regardless of whether tranexamic acid was administered. The routine use of intraoperative tranexamic acid is unlikely to be beneficial for patients undergoing elective lumbar laminectomy.
Strengths & limitations
This study has several strengths. First, given a joint electronic chart system, there is complete follow-up of patients at both institutions. All specialist clinic visits, hospital admissions, and emergency department visits in the city would be identified and tracked. Second, we minimized selection bias by looking at both completed and cancelled cases.
This study also has some limitations. If a patient had a postoperative complication that was treated outside of the University Health Sciences Centre, his or her hospital records would not be seen in our electronic chart review. This would lead to underestimation of the 30-day readmission rate. Given the ease of patient transfer within our local health integration network, we suspect that a patient with a major complication, or one requiring revision surgery, would have been transferred back to our facilities and would therefore have been appropriately included in our study. In addition, all procedures were performed by a single surgeon in one academic setting. It would be valuable to assess the replicability of results, both with respect to preoperative investigations and postoperative outcomes, in different settings.
Conclusions
Despite anesthesiology guidelines that suggest routine preoperative bloodwork should not be ordered prior to low-risk elective surgical procedures, these investigations are still being ordered prior to lumbar laminectomy for spinal stenosis. This may be attributable, at least in part, to hospital policies requesting routine preoperative bloodwork. For this elective procedure, the risk of postoperative complications, including blood transfusion, is low. In an effort to save healthcare resources and limit unnecessary testing, existing hospital policies around elective lumbar laminectomy should be re-evaluated, and routine bloodwork prior to elective lumbar laminectomy may be discontinued. Preoperative investigations for patients at higher risk of perioperative complication should continue to be considered on a case-by-case basis.
Acknowledgements
Funding: Travel costs were covered by the Department of Surgery, Queen’s University to present preliminary results at the Canadian Spine Society 18th Annual Scientific Conference in Banff, Alberta and the Canadian Orthopaedic Association 2018 Annual Meeting in Victoria, British Columbia.
Footnote
Footnote
Conflicts of Interest: Preliminary work was presented at the Canadian Spine Society 18th Annual Scientific Conference in Banff, Alberta; an abstract of this presentation was published in the Canadian Journal of Surgery, 2018;61:S86.
References
- Levinson W, Huynh T. Engaging physicians and patients in conversations about unnecessary tests and procedures: Choosing Wisely Canada. CMAJ 2014;186:325-6. [Crossref] [PubMed]
- Choosing Wisely Canada. Five Things Physicians and Patients Should Question by Canadian Anesthesiologists’ Society. 2017 [cited 22 Aug 2018]. Available online: https://choosingwiselycanada.org/wp-content/uploads/2017/02/Anesthesiology.pdf
- Merchant R, Chartrand D, Dain S, et al. Guidelines to the Practice of Anesthesia - Revised Edition 2016. Can J Anaesth 2016;63:86-112.
- Kirkham KR, Wijeysundera DN, Pendrith C, et al. Preoperative testing before low-risk surgical procedures. CMAJ 2015;187:E349-58. [Crossref] [PubMed]
- Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology 2012;116:522-38. [Crossref] [PubMed]
- Chung F, Yuan H, Yin L, et al. Elimination of preoperative testing in ambulatory surgery. Anesth Analg 2009;108:467-75. [Crossref] [PubMed]
- Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery. Study of Medical Testing for Cataract Surgery. N Engl J Med 2000;342:168-75. [Crossref] [PubMed]
- Kirkham KR, Wijeysundera DN, Pendrith C, et al. Preoperative Laboratory Investigations. Rates and Variability Prior to Low-risk Surgical Procedures. Anesthesiology 2016;124:804-14. [Crossref] [PubMed]
- Lin JS, Chen YJ, Tzeng CH, et al. Revisiting of preoperative blood ordering policy--a single institute's experience in Taiwan. J Chin Med Assoc 2006;69:507-11. [Crossref] [PubMed]
- Wilson WT, Young AM, Fivey P. Minimising costs in spinal surgery: is group & save testing justified in lumbar decompression surgery? J Spine Surg 2016;2:277-80. [Crossref] [PubMed]
- Benarroch-Gampel J, Sheffield KM, Duncan CB, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg 2012;256:518-28. [Crossref] [PubMed]
- Yang MM, Singhal A, Au N, et al. Impact of preoperative laboratory investigation and blood cross-match on clinical management of pediatric neurosurgical patients. Childs Nerv Syst 2015;31:533-9. [Crossref] [PubMed]
- Yonekura H, Seto K, Ide K, et al. Preoperative Blood Tests Conducted Before Low-Risk Surgery in Japan: A Retrospective Observational Study Using a Nationwide Insurance Claims Database. Anesth Analg 2018;126:1633-40. [Crossref] [PubMed]
- Raksakietisak M, Sathitkarnmanee B, Srisaen P, et al. Two Doses of Tranexamic Acid Reduce Blood Transfusion in Complex Spine Surgery: A Prospective Randomized Study. Spine (Phila Pa 1976) 2015;40:E1257-63. [Crossref] [PubMed]
- Elwatidy S, Jamjoom Z, Elgamal E, et al. Efficacy and safety of prophylactic large dose of tranexamic acid in spine surgery: a prospective, randomized, double-blind, placebo-controlled study. Spine (Phila Pa 1976) 2008;33:2577-80. [Crossref] [PubMed]
- Badeaux J, Hawley D. A systematic review of the effectiveness of intravenous tranexamic acid administration in managing perioperative blood loss in patients undergoing spine surgery. J Perianesth Nurs 2014;29:459-65. [Crossref] [PubMed]
- Yu CC, Gao WJ, Yang JS, et al. Can tranexamic acid reduce blood loss in cervical laminectomy with lateral mass screw fixation and bone grafting: a retrospective observational study. Medicine (Baltimore) 2017;96. [Crossref] [PubMed]


