Extreme lateral lumbar interbody fusion (XLIF) in the management of degenerative scoliosis: a retrospective case series
Introduction
Adult degenerative scoliosis (DS) is a spinal deformity, characterized by a Cobb angle more than 10° in the coronal plane, affecting more commonly the lumbar spine (1). DS, although most of the times difficult, should be differentiated from adult idiopathic scoliosis since the latter has a different etiology, presentation and treatment choice (1). The average age of presentation is the 6th decade of life (2), and shows a tendency for deterioration with increasing age. In our days, with the increase of the elderly population, it is seen more and more often with a prevalence ranging from 6% to 68% (1).
Traditionally, when conservative treatment fails, among the procedures used in the treatment of DS, is open instrumented fusion of the spine usually combined with osteotomies and/or anterior fusion, to decompress neural elements, maintain or restore the patient’s balance, aiming at a long-lasting effect. The combination of the severity of these procedures, with the comorbidities seen in this age group, has been associated with a high rate of complications ranging from 20% to 80% (3). Among the risk factors, blood loss of more than 2 liters has been considered to be a predisposing factor (4). During the last decade, minimally invasive techniques have gained space in the treatment of DS in order to decrease the perioperative complications. Among them, extreme lateral interbody fusion (XLIF) has shown promising results.
In this report, we present our initial experience in terms of clinical and radiological parameters in the treatment of DS with XLIF. Furthermore, we report a case who suffered from an inadvertent intraoperative bowel perforation, a rare complication described for this technique.
Methods
We retrospectively reviewed the files of all patients with DS who were underwent XLIF at our institution from October 2008 to March 2017 for DS. Our current study did not require approval from the Hospital’s Institutional Review Board, as it was a retrospective analysis of already existing data extracted from the medical files of our Hospital. For the same reason, no participants’ informed consent was necessary. All the participants’ data were handled according to the Helsinki and the Health Insurance Portability and Accountability (HIPAA) Acts.
We excluded patients with incomplete hospital file and insufficient follow-up period. No participants’ informed consent was necessary for our retrospective study. For the purpose of our study we extracted data related to patients demographics, and clinical parameters such as the pain intensity measured by the visual analogue scale (VAS) (5) and the back-related disability according to the Oswestry Disability Index (ODI) (6). Moreover, we recorded radiological data, including the Cobb angle and spinal alignment at the sagittal plane. The measures were performed preoperatively, at the immediate post-operative period and at 3, 6, and 12 months after the index surgery. Finally, we recorded the duration of surgery and the amount of blood loss intra-operatively.
Throughout the procedure the patient was positioned in a lateral decubitus position with a lateral bolster between 12th rib and the iliac crest so as to achieve maximal distraction of the target disc. The whole procedure took place under fluoroscopic guidance and continuous neurophysiological monitoring. The target disc was localized at both the true antero-posterior and true lateral projections and is approached through a small skin incision, not larger than 3 cm. The peritoneum was detached from the neighboring groups of muscles. Proper care was implemented in order to avoid inadvertent injury to the adjacent large vessels, hollow organs and lumbosacral plexus. Discectomy took place after an automatic retractor was anchored at the lateral side of the disc, and a large interbody poly-ether-ketone cage, with a foot-print occupying the whole axial diameter of the vertebrae, filled with DBM was ultimately positioned.
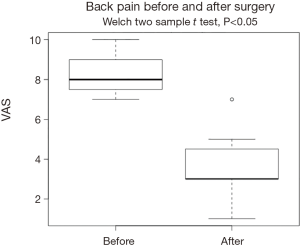
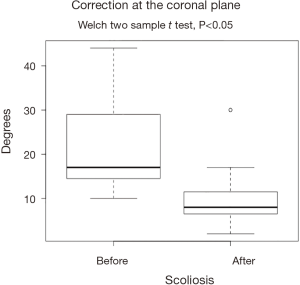
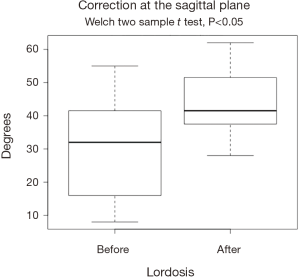
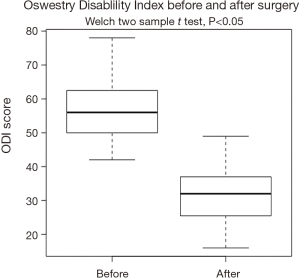
We used descriptive statistics to summarize our data. Continuous variables were summarized as mean and standard deviation (SD), while factor variables were grouped as counts and frequencies (%). Comparisons between groups were performed with the Student’s t-test and the chi-square where appropriate. Differences between repeated measures were plotted as consecutive boxplots. The level of statistical confidence was set at 0.05. All statistical analyses were performed using the R-statistical environment (7).
Results
Study sample
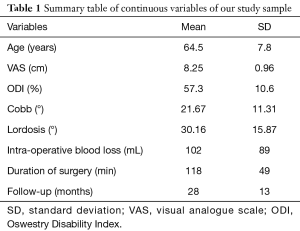
Twelve patients fulfilled the eligibility criteria of our study. All patients were female, with a mean age of 64.5 years (SD =7.8 years) and 28 months (SD =13 months) follow-up. The most prominent symptom in all patients was mechanical low back pain, with/without radicular symptoms and/or neurogenic claudication, not responding to conservative treatment for at least 6 months. The average scoliosis was 21.6° (SD =11.31°), while the average value of lordosis as measured from the upper endplate of L1 to the upper endplate of S1 was 30.16° (SD =15.87°). The average preoperative ODI score was 57.3% (SD =10.6%), with an average back pain VAS score was 8.25 cm (SD=0.96 cm). The patient demographic characteristics are presented on Tables 1 and 2.
Full table
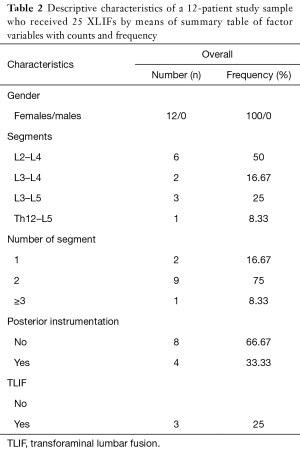
Full table
Twenty-five interbody cages were placed with a mean operative time per case of 118 minutes (SD =49 minutes), and an average blood loss of 102 mL (SD =89 mL) when considering only the XLIF technique (Table 1). Four patients (33%) underwent supplemental instrumentation, in 1 patient transpedicular screws were inserted after posterior decompression through an open approach, and in 3 patients the procedure was completed after decompression, TLIF at L4–L5 level and transpedicular screws, in 1 patient through an open approach, and in the rest through MIS technique.
The XLIF decreased the pain intensity by 4.66 cm (SD =1.23 cm), and improved the back-related disability by 26% (SD =8.35%) in the ODI scale at the 6-month follow-up. Similarly, scoliosis improved by an average of 11.5° (SD =7°) and lordosis changed by an average of 13.5° (SD =10.86°). All changes were statistically significant, and are visualized at Figures 1-4.
We encountered three complications, as two patients experienced meralgia paresthetica with complete recovery in 3 months, and one patient developed ileus, due to intraoperative bowel injury, necessitating laparoscopy and segmental bowel resection. Moreover, in all three patients, received an XLIF at L4–L5 level.
Discussion
DS origins from an asymmetric disc degeneration and facet hypertrophy, leading to progressive loss of lumbar lordosis with increasing deformity in all 3 planes and altered spinopelvic parameters (1). Factors contributing further to its progression is lateral listhesis rotational deformity and osteoporotic vertebral fractures (8). It has also been suggested by Seo et al. (9) that the presence of vertebra L5, below the intercristal line, and asymmetric discopathy below L3 to be predictors of worsening scoliosis. In cases not responding to medical treatment several surgical options exist depending on the main symptom. When the predominant symptom is back pain, proper balance restoration with or without decompression reliefs symptoms in the majority of the patients. In many cases either osteotomies or anterior column support in combination with posterior instrumentation, to achieve an efficient balance is mandatory. These techniques have been associated with increased risk of morbidity (4,8). Hence, the achievement of greatest benefit with decreased perioperative risk it has to be the goal when surgery is considered in these patients.
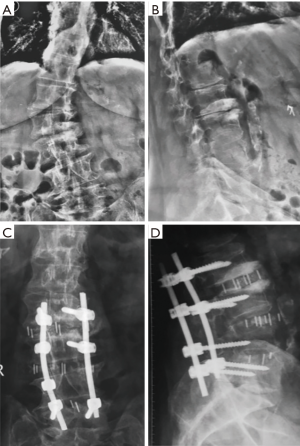
Minimally invasive techniques have been introduced in order to decrease perioperative complications. Their efficacy in the treatment of patients with adult scoliosis has been shown in several studies (10,11). Their goals are to minimize iatrogenic muscle trauma, reduce blood loss, permitting an earlier mobilization of the patient and decreasing hospital stay. Among them, XLIF has shown an advantage in achieving a better deformity correction (8). XLIF for the treatment of lumbar pathology it was first published in the literature in 2006 (12), and description of the technique, as well as its anatomical details, have been widely described (12-15). It is a muscle and ligament sparing procedure, allowing, preservation of the spine’s stabilizer, including the ALL and posterior osteoligamentous complex (14,15). In addition, the size of the interbody implant, as well as its position within the intervertebral space spanning the ring apophysis, provides maximum vertebral support and achieves an indirect decompression through ligamentotaxis. These advantages have as a consequence an efficient correction in all 3 planes, facilitation of alignment and increased segmental stability (Figure 5).
When compared biomechanically to other interbody techniques, it also provides a less risk of cage subsidence since the lateral regions of the endplate are strongest and stiffest than the central region (16).
It was first reported as a technique for the treatment of patients with DS by Pimenta et al. (17). Since then, several studies reported on its efficacy and safety-profile in this particular population (3,18-20). Phillips et al. (20) in their study concluded that XLIF, compared to open traditional procedures, is associated with similar clinical and radiographic results, improvement of coronal and sagittal alignment and a lower complication rate. The overall complication rate for this technique in a large series of 600 patients has reported being 6.2% (21), while when considering only patients treated for DS, Isaacs et al. reported a major complication rate of 12.1% (22).
The results of our study confirm the efficacy of XLIF reported in the literature regarding the treatment of patients with adult DS. VAS and ODI improved by an average of 46% and 26%, respectively. Similar are the findings for the achievement of coronal and sagittal restoration, showing an average improvement of 11.5° (SD =7.5°) and 13.5° (SD =10.86°), respectively. In our series we had 3 complications, 2 patients with meralgia paresthetica resolved completely within 3 months, and 1 patient with bowel perforation treated surgically. As a consequence, our total complication rate was 25% and 8.33% when only major complications are considered. Bowel perforation is a major complication, and only a few cases have been reported in the literature (23-27). The complication, in our series, to our opinion, occurred apart from the steep learning curve known for this procedure, from the fact that because of the level treated (L4–L5), we tried to be as anterior as possible resulting in this inadvertent intraoperative injury. It is worthy to note that this patient was the only treated with a single incision, instead of the two-incision technique we are used to, and that has been initially described for this procedure. Limitations of this study are quite evident since this represents a small series of patients, treated for DS from a group still improving its learning curve in this technique.
Conclusions
XLIF is a feasible and efficient alternative in the treatment of DS. It can be the treatment of choice in elderly patients in whom comorbidities increase the perioperative risk of complications. Multi-segmental correction can be performed with less blood loss and morbidity than for traditional open procedures, achieving, at least, the same clinical and radiological results. However, although rare, does not preclude the occurrence of major complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study did not require approval from the Hospital’s Institutional Review Board, as it was a retrospective analysis of already existing data extracted from the medical files of our Hospital. All the participants’ data were handled according to the Helsinki and the Health Insurance Portability and Accountability (HIPAA) Acts.
References
- Kotwal S, Pumberger M, Hughes A, et al. Degenerative Scoliosis: A Review. HSS J 2011;7:257-64. [Crossref] [PubMed]
- Gupta MC. Degenerative scoliosis: Options for surgical management. Orthop Clin North Am 2003;34:269-79. [Crossref] [PubMed]
- Dakwar E, Cardona RF, Smith DA, et al. Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus. Neurosurg Focus 2010;28. [Crossref] [PubMed]
- Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976) 2007;32:2232-7. [Crossref] [PubMed]
- Luria RE. The validity and reliability of the visual analogue mood scale. J Psychiatr Res 1975;12:51-7. [Crossref] [PubMed]
- Fairbank JC, Pynsent PB. Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940-52; discussion 2952. [Crossref] [PubMed]
- R Development Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2016.
- Dangelmajer S, Zadnik PL, Rodriguez ST, et al. Minimally invasive spine surgery for adult degenerative lumbar scoliosis. Neurosurg Focus 2014;36. [Crossref] [PubMed]
- Seo JY, Ha KY, Hwang TH, et al. Risk of progression of degenerative lumbar scoliosis. J Neurosurg Spine 2011;15:558-66. [Crossref] [PubMed]
- Kanter AS, Tempel ZJ, Ozpinar A, et al. A Review of Minimally Invasive Procedures for the Treatment of Adult Spinal Deformity. Spine (Phila Pa 1976) 2016;41 Suppl 8:S59-65. [PubMed]
- Anand N, Baron EM, Khandehroo B, et al. Long-term 2- to 5-Year Clinical and Functional Outcomes of Minimally Invasive Surgery for Adult Scoliosis. Spine (Phila Pa 1976) 2013;38:1566-75. [Crossref] [PubMed]
- Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 2006;6:435-43. [Crossref] [PubMed]
- Berjano P, Lamartina C. Minimally invasive lateral transpsoas approach with advanced neurophysiologic monitoring for lumbar interbody fusion. Eur Spine J 2011;20:1584-6. [Crossref] [PubMed]
- Hood B, Vanni S. Minimally Invasive Extreme Lateral Trans-Psoas Approach to the Lumbar Spine: Applications and Techniques. In: Chung K. editor. Spine Surgery. Rijeka, Croatia: InTech, 2012:43-78.
- Billinghurst J, Akbarnia BA. Extreme lateral interbody fusion - XLIF. Curr Orthop Pract 2009;20:238-51. [Crossref]
- Grant JP, Oxland TR, Dvorak MF. Mapping the Structural Properties of the Lumbosacral Vertebral Endplates. Spine (Phila Pa 1976) 2001;26:889-96. [Crossref] [PubMed]
- Pimenta L, Lhamby J, Gharzedine I, et al. 107. XLIF Approach for the Treatment of Adult Scoliosis: 2-year Follow-up. Spine J 2017;7:52S-3S. [Crossref]
- Mundis GM, Akbarnia BA, Phillips FM. Adult deformity correction through minimally invasive lateral approach techniques. Spine (Phila Pa 1976) 2010;35:S312-21. [Crossref] [PubMed]
- Berjano P, Lamartina C. Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J 2013;22 Suppl 2:S242-53. [Crossref] [PubMed]
- Phillips FM, Isaacs RE, Rodgers WB, et al. Adult Degenerative Scoliosis Treated With XLIF. Spine (Phila Pa 1976) 2013;38:1853-61. [Crossref] [PubMed]
- Rodgers WB, Gerber EJ, Patterson J. Intraoperative and Early Postoperative Complications in Extreme Lateral Interbody Fusion. Spine (Phila Pa 1976) 2011;36:26-32. [Crossref] [PubMed]
- Isaacs RE, Hyde J, Goodrich JA, et al. A Prospective, Nonrandomized, Multicenter Evaluation of Extreme Lateral Interbody Fusion for the Treatment of Adult Degenerative Scoliosis. Spine (Phila Pa 1976) 2010;35:S322-30. [Crossref] [PubMed]
- Uribe JS, Deukmedjian AR. Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: a survey study and literature review. Eur Spine J 2015;24:386-96. [Crossref] [PubMed]
- Fujibayashi S, Kawakami N, Asazuma T, et al. Complications Associated With Lateral Interbody Fusion: Nationwide Survey of 2998 Cases During the First 2 Years of Its Use in Japan. Spine (Phila Pa 1976) 2017;42:1478-84. [Crossref] [PubMed]
- Balsano M, Carlucci S, Ose M, et al. A case report of a rare complication of bowel perforation in extreme lateral interbody fusion. Eur Spine J 2015;24 Suppl 3:405-8. [Crossref] [PubMed]
- Malham GM, Ellis NJ, Parker RM, et al. Clinical Outcome and Fusion Rates after the First 30 Extreme Lateral Interbody Fusions. ScientificWorldJournal 2012;2012. [Crossref] [PubMed]
- Tormenti MJ, Maserati MB, Bonfield CM, et al. Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation. Neurosurg Focus 2010;28. [Crossref] [PubMed]