
Thirty-day complication and readmission rates associated with resection of metastatic spinal tumors: a single institutional experience
Introduction
Surgical resection of spinal metastases is challenging and represents a difficult treatment paradigm due to associated complication rates, patient morbidities, and poor outcomes (1,2). Spinal metastasis has been estimated to occur in 5–30% of primary cancers, with the most common primary sites coming from breast, prostate, and kidney (3). Metastatic spinal tumors often compress the spinal cord producing pain, loss of mobility, incontinence, and overall decreased quality of life (4). With modern advances in oncologic therapeutic approaches, life expectancy for spinal metastases patients have been extended and spinal metastases are now seen with increasing prevalence (5).
Although a curative state is not achieved, surgical decompression has been shown to significantly alleviate disabling symptoms and improve quality of life compared to other monotherapies, such as radiation therapy alone (6,7). However, due to the reduced state of health of these patients, there is an increased risk for peri-operative complications and morbidity associated with surgical resection (8-13). With a growing national emphasis on reducing overall complication and readmission rates, risk stratifying patients and addressing avoidable complications after resection of spinal metastases is necessary to optimize quality of care and reduce the disparaging healthcare costs (14-17). While previous studies have explored in-hospital complication rates and surgical outcomes for patients undergoing metastatic spinal tumor resections (8-13), there is a paucity of data investigating 30-day complication and readmission rates.
The aim of this study is to investigate the 30-day complication and unplanned readmission rates associated with surgical resection of metastatic spinal tumors.
Methods
In this retrospective study, we reviewed the medical records of 135 adult (≥18 years old) patients who underwent elective spine surgery for resection of spinal cord tumor at a major academic institution from 2005 to 2015. Institutional Review Board approval was obtained before initiation of the study. Tumor pathology was analyzed and diagnosed by a board-certified pathologist. Of the 135 reviewed cases, 30 (22.2%) were identified as metastatic by pathology and clinical presentation. The primary outcomes of this study were intra- and 30-day complication and unplanned readmission rates of the metastatic tumor resection cohort.
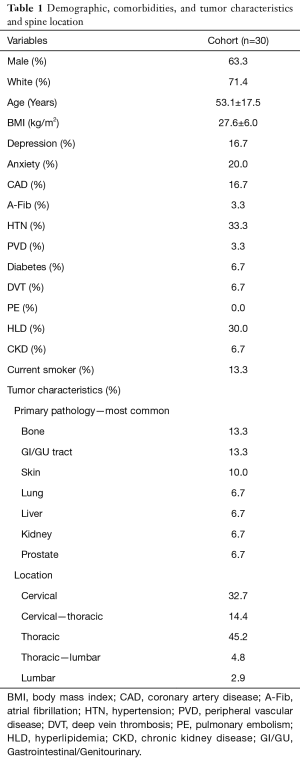
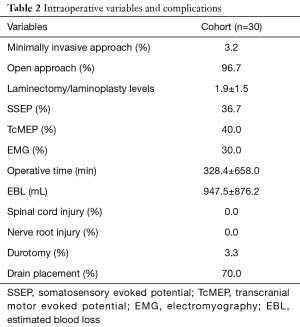
Demographic variables evaluated were patient gender, race, age, and body mass index (BMI). Comorbidities included depression, anxiety, coronary artery disease (CAD), atrial fibrillation (A-Fib), hypertension (HTN), peripheral vascular disease (PVD), diabetes, deep vein thrombosis (DVT), pulmonary embolism (PE), hyperlipidemia (HLD), chronic kidney disease (CKD), and current smoking status. Tumor characteristics evaluated were pathology-determined primary tumor location and anatomic level of metastasis to the spine. Intraoperative variables recorded were operative approach (open vs. minimally invasive), number of vertebral levels involved in laminectomy/laminoplasty, operative time, estimated blood loss (EBL), drain placement, and use of somatosensory evoked potentials (SSEP), transcranial motor evoked potentials (TcMEP), and electromyography (EMG). Intra-operative complications assessed were spinal cord injury, nerve root injury, and durotomy.
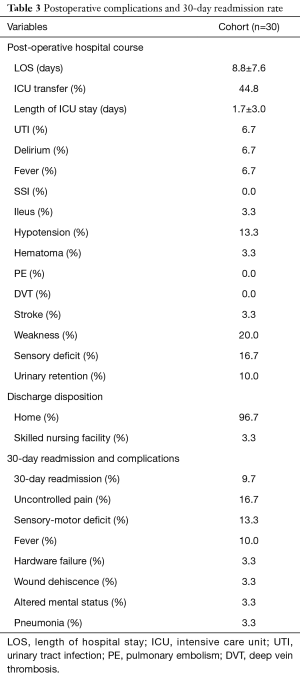
Post-operative complications recorded were length of hospital stay, intensive care unit (ICU) transfer, length of ICU stay, urinary tract infection (UTI), delirium, fever, surgical site infection (SSI), ileus, hypotension, hematoma, PE, DVT, stroke, weakness, sensory deficit, and urinary retention. Discharge disposition and 30-day complication and readmission rates were also evaluated.
Parametric data were expressed as mean ± standard deviation (SD) and compared using the Student’s t-test. Nonparametric data were expressed as median (interquartile range) and were compared using the Mann-Whitney U test. Nominal data were compared with the χ2 test. All tests were 2-sided and were statistically significant if the P value was <0.05. Statistical analysis was performed using JMP Version 12 (SAS Institute Inc., Cary, North Carolina, USA).
Results
Of the 135 spinal tumor resection cases reviewed, 30 (22.2%) were found to be metastatic and were included in this study. The mean age and BMI of the metastatic cohort was 53.1±17.5 years and 27.6±6.0 kg/m2, respectively (Table 1). The majority of the metastatic cohort was male (63.3%) and White (71.4%) (Table 1). The prevalence of comorbidities included depression (16.7%), anxiety (20.0%), CAD (16.7%), A-Fib (3.3%), HTN (33.3%), PVD (3.3%), diabetes (6.7%), DVT (6.7%), HLD (30.0%), CKD (6.7%), and current smoking status (13.3%) (Table 1). The most prevalent primary tumor pathologies associated with spinal metastases included bone (13.3%), Gastrointestinal/Genitourinary (GI/GU) tract (13.3%), skin (10.0%), lung (6.7%), liver (6.7%), kidney (6.7%), and prostate (6.7%) (Table 1). The most prevalent spinal tumor location was thoracic alone (45.2%), followed by cervical alone (32.7%) and cervical-thoracic (14.4%), Table 1.
Full table
The vast majority of metastatic tumor resections were performed by open surgical approach (96.7%) (Table 2). The mean number of laminectomy/laminoplasty levels was 1.9±1.5 vertebral levels (Table 2). The prevalence of intraoperative monitoring utilized in during the resections included 36.7% SSEP, 40.0% TcMEP, and 30.0% EMG (Table 2). The mean operative time and EBL was 328.4±658.0 minutes and 947.5±876.2 mL, respectively (Table 2). The incidence of durotomy was 3.3%, with no intra-operative nerve root or spinal cord injury occuring. A surgical drain was placed in 70.0% of cases (Table 2).
Full table
The mean length of hospital stay was 8.8±7.6 days (Table 3). ICU transfer occurred in 44.8% of cases, with a mean length of ICU stay being 1.7±3.0 (Table 3). Inpatient post-operative complications included UTI (6.7%), delirium (6.7%), fever (6.7%), ileus (3.3%), hypotension (13.3%), hematoma (3.3%), stroke (3.3%), weakness (20.0%), sensory deficit (16.7%), and urinary retention (10.0%) (Table 3). There were no instances of post-operative SSI, PE, or DVT (Table 3).
Full table
The most common discharge disposition was home (96.7%), followed by skilled nursing facility (3.3%). The readmission rate within 30 days of discharge was 9.7% (Table 3). The most common 30-day complications were uncontrolled pain (16.7%) and sensory-motor deficit (13.3%), followed by fever (10.0%), hardware failure (3.3%), wound dehiscence (3.3%), altered mental status (3.3%), and pneumonia (3.3%) (Table 3).
Discussion
In this retrospective study of metastatic spinal tumor resections, we observed a relatively high 30-day hospital readmission rate, with the most prevalent 30-day complications being weakness, sensory deficits, and uncontrolled pain.
There have been a few prior studies have attempted to identify complication and readmission rates associated metastatic spinal tumor resections. In a retrospective study of 164 patients who underwent resection of metastatic spinal tumors, Schairer et al. demonstrated an unplanned 30-day hospital readmission rate of 16.8%, with 7.7% of 1-year readmissions due to pain and 3.3% for palliative care (13). Similarly, in a retrospective study of 118 patients who underwent resection of extradural spinal metastases, Lau et al. reported a 90-day readmission rate of 11.9%, with a diagnosis of lung metastasis as an independent predictor of readmission (18). In a prospective study of 282 patients undergoing surgery for spinal metastases, Jansson et al. observed an overall complication rate of 20%, with 5% of patients experiencing worsened motor deficits post-operatively (19). In another retrospective study of 26,233 patients with surgically managed spinal metastases, Patil et al. showed an inpatient complication rate of 21.9%, with pulmonary and postoperative hemorrhages or hematomas was the most common complications reported (8). Analogous to the aforementioned studies, our study suggests that patients undergoing spinal metastasis resection are at high risk of overall post-operative complications in addition to unplanned readmissions.
High complication rates associated with metastatic spinal tumor resections have been attributable to both the technical difficulty of the procedure and baseline health status of the patient population. Specifically, en bloc resections have been found to increase the complexity and prevalence of intraoperative complications when resecting spinal cord tumors (20,21). In a retrospective study of 1,035 patients undergoing en bloc resection for spinal tumors, Boriani et al. observed an overall 34.3% intra-operative complication rate, with 2.2% of patients who subsequently died due to associated complications (22). Challenges include distortion of normal anatomy by tumor, tumor involvement of vital structures, compromise of integrity of surrounding bone used in reconstruction, and frequent requirement for simultaneous anterior and posterior surgical approach (20). Therefore, there have been efforts to modify en-bloc surgical techniques to optimize surgical resection and minimize associated complications. For instance, in a retrospective study of 33 patients who underwent a modified, 2-stage total en bloc spondylectomy for spinal tumors, Shah et al. demonstrated that the modified technique in selected patients increased visualization of anterior vessels and reduced spinal cord injuries (23). Along with the complexity of the surgical resections, metastatic cancer patients have compromised nutritional status and overall health, and are inherently at an increased surgical risk (10,11). However, despite the high associated morbidity with resection, surgical intervention for spinal metastasis remains the most effective palliative treatment option (6,7,9,24). Therefore, further efforts in optimizing patient selection and surgical approach are necessary maximize the patient benefit and minimize injuries associated with these procedures.
Increasing attention towards decreasing complication and readmission rates are important considerations to ensure optimal patient care, but also to lower healthcare costs. Surgical complications have been estimated to increase cost of hospitalization anywhere from $9,607 for minor complications (25,26) to $159,245 for the most severe complications (27). Moreover, unplanned readmissions are estimated to cost the US health care system over $20 billion annually (28). Patil et al. demonstrated that a single in-house, post-operative complication increases the mean length of hospital stay by 7 days and hospital charges by over $20,000 in patients undergoing metastatic spinal tumor resection (8). Similarly, in a retrospective study of 15,545 intramedullary spinal cord tumor resections, Sharma et al. also found that a single complication increased total hospital charges by more than $20,000 (29). Lau et al. reports that patients undergoing epidural metastasis resection who experience a complication accrue approximately twice the hospital cost (>$40,000) compared to patients without complications (18). Furthermore, the authors found that the mean cost of hospital readmissions was approximately $20,078 in this patient population (18). With exorbitant healthcare costs becoming an increasingly pressing public health issue, the need for targeted efforts to reduce expensive hospital complications and readmissions is readily apparent (30).
One of the most significant ways to decrease morbidity associated with metastatic spinal tumor resection is to improve the ability to determine surgical candidacy in the pre-operative setting (31). Given the palliative nature of these procedures, the remaining survival and potential benefit to the quality of life of the patient must be carefully weighed against the risk of complication and prolonged or repeated hospitalization secondary to surgery (31). For this reason, there has been growing interest in the development of prognostic scoring systems to aid surgeons in making this challenging determination (14-17). Accordingly, a number of risk calculators for spinal metastasis resection have been developed including Bauer (32), Tokuhashi (33,34), Tomita (14), van der Linden (35), and Sioutos (31,36). These systems include pre-operative risk factors such as characteristics and type of primary tumor, neurologic deficit, extent and location of metastases, and other medical comorbidities to predict remaining survival (14,31-36). Multiple studies have been conducted to validate these predictive systems. In a retrospective study comparing surgery versus conservative treatment in 254 patients with spinal metastases, Wibmer et al. found that of the previously mentioned seven systems, all were capable of distinguishing between good and poor prognosis (31). The most significant limitation of these scoring systems is that they are designed to only predict remaining survival, but do not include other important information such as surgical complications and readmission rates. In order to reduce patient morbidity and health care expenses, we aim for our study to inform the creation of future risk calculators that reflect both post-operative complication and readmission rates.
This study has limitations with implications for its interpretation. Readmissions to unaffiliated hospitals were not identified, which may have resulted in an underestimate of 30-day readmission and complication rates. Our small sample size limits our ability to make any firm conclusions. Finally, although pre- and perioperative variables were prospectively recorded into the study registry at the time of surgery, these variables were retrospectively analyzed for the purposes of this study and are subject to the drawbacks associated with all retrospective reviews. Despite these limitations, this study identifies 30-day readmission rate and common postoperative complications after surgical resection of metastatic spinal tumors.
Conclusions
Our study suggests that weakness, sensory deficits, and uncontrolled pain are the most common complications occurring between the time of surgery and 30-day post discharge, and are associated with a relatively high 30-day readmission rate. Further studies are necessary to corroborate our findings and identify strategies to reduce 30-day complication and readmission rates after surgical resection of metastatic spinal tumors.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval was obtained before initiation of the study (Pro00066331).
References
- Dea N, Versteeg A, Fisher C, et al. Adverse events in emergency oncological spine surgery: a prospective analysis. J Neurosurg Spine 2014;21:698-703. [Crossref] [PubMed]
- Schoenfeld AJ, Leonard DA, Saadat E, et al. Predictors of 30- and 90-Day Survival Following Surgical Intervention for Spinal Metastases: A Prognostic Study Conducted at Four Academic Centers. Spine (Phila Pa 1976) 2016;41:E503-9. [Crossref] [PubMed]
- Yao A, Sarkiss CA, Ladner TR, et al. Contemporary spinal oncology treatment paradigms and outcomes for metastatic tumors to the spine: A systematic review of breast, prostate, renal, and lung metastases. J Clin Neurosci 2017;41:11-23. [Crossref] [PubMed]
- Ryken TC, Eichholz KM, Gerszten PC, et al. Evidence-based review of the surgical management of vertebral column metastatic disease. Neurosurg Focus 2003;15. [Crossref] [PubMed]
- Jacobs WB, Perrin RG. Evaluation and treatment of spinal metastases: an overview. Neurosurg Focus 2001;11. [Crossref] [PubMed]
- Klimo P Jr, Thompson CJ, Kestle JR, et al. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro-oncology 2005;7:64-76. [Crossref] [PubMed]
- Ibrahim A, Crockard A, Antonietti P, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine 2008;8:271-8. [Crossref] [PubMed]
- Patil CG, Lad SP, Santarelli J, et al. National inpatient complications and outcomes after surgery for spinal metastasis from 1993–2002. Cancer 2007;110:625-30. [Crossref] [PubMed]
- Weigel B, Maghsudi M, Neumann C, et al. Surgical management of symptomatic spinal metastases: postoperative outcome and quality of life. Spine 1999;24:2240. [Crossref] [PubMed]
- Wise JJ, Fischgrund JS, Herkowitz HN, et al. Complication, survival rates, and risk factors of surgery for metastatic disease of the spine. Spine 1999;24:1943. [Crossref] [PubMed]
- Finkelstein JA, Zaveri G, Wai E, et al. A population-based study of surgery for spinal metastases. Survival rates and complications. J Bone Joint Surg Br 2003;85:1045-50. [Crossref] [PubMed]
- Bauer HC. Posterior decompression and stabilization for spinal metastases. Analysis of sixty-seven consecutive patients. J Bone Joint Surg Am 1997;79:514-22. [Crossref] [PubMed]
- Schairer WW, Carrer A, Sing DC, et al. Hospital readmission rates after surgical treatment of primary and metastatic tumors of the spine. Spine 2014;39:1801-8. [Crossref] [PubMed]
- Tomita K, Kawahara N, Kobayashi T, et al. Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2001;26:298-306. [Crossref] [PubMed]
- Barzilai O, Laufer I, Yamada Y, et al. Integrating Evidence-Based Medicine for Treatment of Spinal Metastases Into a Decision Framework: Neurologic, Oncologic, Mechanicals Stability, and Systemic Disease. J Clin Oncol 2017;35:2419-27. [Crossref] [PubMed]
- Afsar A, Qadeer M, Sharif S. Surgically treated spinal metastases: Do prognostic scores have a role? Surg Neurol Int 2017;8:158. [Crossref] [PubMed]
- Gruenberg M, Mereles ME, Willhuber GOC, et al. Usefulness of Tokuhashi Score in Survival Prediction of Patients Operated for Vertebral Metastatic Disease. Global Spine J 2017;7:260-5. [Crossref] [PubMed]
- Lau D, Chan AK, Theologis AA, et al. Costs and readmission rates for the resection of primary and metastatic spinal tumors: a comparative analysis of 181 patients. J Neurosurg Spine 2016;25:366-78. [Crossref] [PubMed]
- Jansson KÅ, Bauer HCF. Survival, complications and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J 2006;15:196-202. [Crossref] [PubMed]
- Schoenfeld AJ, Ochoa LM, Bader JO, et al. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am 2011;93:1577-82. [Crossref] [PubMed]
- Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: systematic review and meta-analysis. Neurosurg Focus 2015;39. [Crossref] [PubMed]
- Boriani S, Bandiera S, Donthineni R, et al. Morbidity of en bloc resections in the spine. Eur Spine J 2010;19:231-41. [Crossref] [PubMed]
- Shah AA, Paulino Pereira NR, Pedlow FX, et al. Modified En Bloc Spondylectomy for Tumors of the Thoracic and Lumbar Spine: Surgical Technique and Outcomes. J Bone Joint Surg Am 2017;99:1476-84. [Crossref] [PubMed]
- Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 2005;366:643-8. [Crossref] [PubMed]
- Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: A report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004;199:531-7. [Crossref] [PubMed]
- Healy MA, Mullard AJ, Campbell DA Jr, et al. Hospital and Payer Costs Associated With Surgical Complications. JAMA Surg 2016;151:823-30. [Crossref] [PubMed]
- Vonlanthen R, Slankamenac K, Breitenstein S, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 2011;254:907-13. [Crossref] [PubMed]
- Hines AL, Barrett ML, Jiang HJ, et al. Conditions with the largest number of adult hospital readmissions by payer, 2011. Available online: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb172-Conditions-Readmissions-Payer.jsp
- Sharma M, Sonig A, Ambekar S, et al. Discharge dispositions, complications, and costs of hospitalization in spinal cord tumor surgery: analysis of data from the United States Nationwide Inpatient Sample, 2003–2010. J Neurosurg Spine 2014;20:125-41. [Crossref] [PubMed]
- Epstein AM. Revisiting readmissions—changing the incentives for shared accountability. N Engl J Med 2009;360:1457-9. [Crossref] [PubMed]
- Wibmer C, Leithner A, Hofmann G, et al. Survival analysis of 254 patients after manifestation of spinal metastases: evaluation of seven preoperative scoring systems. Spine (Phila Pa 1976) 2011;36:1977-86. [Crossref] [PubMed]
- Bauer H, Tomita K, Kawahara N, et al. Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2002;27:1124-6. [Crossref] [PubMed]
- Tokuhashi Y, Matsuzaki H, Oda H, et al. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005;30:2186-91. [Crossref] [PubMed]
- Tokuhashi Y, Matsuzaki H, Toriyama S, et al. Scoring system for the preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 1990;15:1110-3. [Crossref] [PubMed]
- van der Linden YM, Dijkstra SP, Vonk EJ, et al. Prediction of survival in patients with metastases in the spinal column: results based on a randomized trial of radiotherapy. Cancer 2005;103:320-8. [Crossref] [PubMed]
- Sioutos PJ, Arbit E, Meshulam CF, et al. Spinal metastases from solid tumors. Analysis of factors affecting survival. Cancer 1995;76:1453-9. [Crossref] [PubMed]


