Extra-skeletal Ewing sarcoma of the lumbosacral region in an adult pregnant patient: a case report
Introduction
Extra-skeletal Ewing sarcoma is a rare subtype within the Ewing sarcoma family of tumors (ESFT) (1-3). It is a highly aggressive soft tissue tumor that responds considerably well to robust local therapies, such as complete surgical resection (1,2). Tumors of this kind occur in both appendicular and axial locations, but have a poorer prognosis when present axially (1,4). The incidence of the extra-skeletal subtype is rare in adults and development within the context of active pregnancy rarer still (4,5). Given the scarcity of such an illness, there is scant evidence available to guide clinicians in the management of affected patients. Management strategies are consequently based on anecdotal evidence and a limited number of existing case reports and small series (5). We herewith report a unique approach to the management of extra-skeletal Ewing sarcoma in a pregnant patient—aggressive complete surgical resection prior to 20-weeks’ gestation followed by adjuvant chemotherapy at a later date.
Case presentation
A 32-year-old woman presented in her 16th week of pregnancy, G3P2, with a 2-month history of progressive, nocturnal right-sided back; and gluteal pain. The pain radiated into her right lower limb, roughly approximating the L5 and S1 distribution, and was associated with paraesthesia. Despite strong analgesics, including morphine, the patients’ pain severity score persisted at 10/10. She had no other significant medical history.
On examination, spinal movements were pain-limited, particularly worst on flexion. There was a marked right paraspinal swelling. Straight leg raise in the right leg was limited to 10 degrees. Right foot plantar flexion was weak and scored 3/4 in power. Right ankle jerk was absent. The power in her upper and lower limbs was otherwise normal.
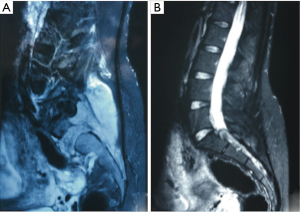
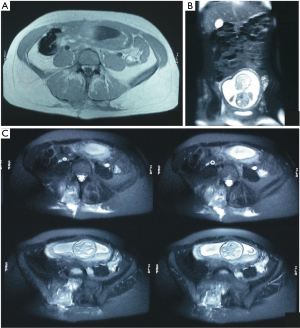
Lumbosacral magnetic resonance imaging (MRI) revealed an approximate 40 mm × 50 mm indeterminate mass in the lower right paraspinal musculature. There was extension of the mass into the first right sacral foramen and the central canal. The mass also impinged on the S2 exiting nerve (Figures 1,2). Given the patients’ pregnant status, neither more dedicated contrast imaging nor a bone scan was possible. She was subsequently admitted to hospital for acute pain management.
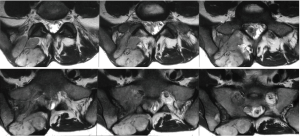
After a multidisciplinary meeting including an obstetrician, the decision was made to undergo radical surgical intervention to excise the mass. She was consequently operated on whilst 18-weeks’ pregnant and prior to receiving any chemotherapy or radiation therapy. The complex operation involved a right vertical paraspinal incision, extending from the L4 vertebra to the sacrum. The large mass was identified within the paraspinal musculature and was carefully dissected away from the paraspinal region. An en-bloc excision was not possible and thus the tumor was removed in two great pieces. Hemi-laminectomy of L5, S1 and S2 vertebrae were performed to gain access to the epidural portion which was found to be adherent to the right S2 nerve root. This was carefully dissected away from the S2 nerve root and the epidural portion subsequently removed (Figure 3).
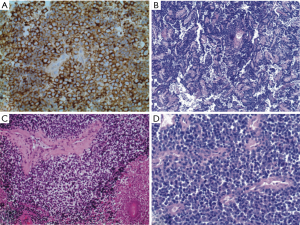
Histopathological examination of the biopsied mass revealed islands of small blue round tumor cells with prominent necrosis. The tumor cells were strongly membrane positive for CD99, nuclear positive for S100 and positive for cytoplasmic glycogen (Figure 4). Given the morphological, histochemical and immunochemical findings, as well as the absence of any bone involvement, a provisional diagnosis of extra-skeletal Ewing sarcoma was made. Molecular cytogenetics subsequently confirmed the diagnosis with the presence of EWSRI-FLI1 rearrangement.
A post-operative MRI was taken on day seven showing no residual tumor (Figure 5). The patient experienced immediate resolution of the pain and was discharged home 48 hours after surgery, with no complications. Six weeks following the surgery, she was able to comfortably cease the use of all analgesics for her pain.
Beginning at 20-weeks’ gestation, she underwent three cycles of vincristine, doxorubicin and cyclophosphamide (VDC) chemotherapy for the soft tissue tumor. Given the decision to continue with the pregnancy, chemotherapy was only continued until 32-weeks’ gestation - the earliest possible time for delivery. She tolerated the chemotherapy well with her main side effect being fatigue.
At 32-weeks’ gestation, as per schedule, she was induced and underwent an uncomplicated vaginal delivery. Following the delivery, she undertook 40 days of radiation therapy given in 28 fractions to the paraspinal region. This was well tolerated. She then continued on systemic chemotherapy and completed a full 14 cycles.
At the most recent follow-up of 9 months, she remains disease free and has experienced complete resolution of the right sided back and gluteal pain. She has been successfully weaned off all analgesic medications. At 6 months of age, her infant has had a normal growth with no physical or developmental deficits.
Discussion
Among the four subtypes within the high-grade and aggressive ESFT, extra-skeletal Ewing sarcoma is rare (1-3). Unlike the classical osseous based sarcoma presenting in children and adolescent males, the extra-skeletal subtype occurs in soft tissue with less of a male predilection; and at peak incidence in the second and third decades of life. Though seemingly distinct, the subtypes all arise from a common gene translocation resulting in a fused EWS/FLI1 gene (1,2). Treatment for the subtypes is thus similarly based and follows a rather standardized protocol (2). The protocol includes 14–17 cycles of neo-adjuvant chemotherapy, definitive resection surgery if possible and 6 weeks of daily radiation treatment to the primary site, if complete surgical resection is not possible (2). An initially robust response to treatment is usually seen irrespective of a primary or metastatic neoplasm—this is a unique trait of the ESFT (1,2). Though, like other sarcomas, the ESFT are known to have a poorer prognosis for tumors arising axially when compared to the appendicular location (1,4). This is a risk that persists despite adjustment for both pre-treatment and treatment variables and is suspected to be due to the intrinsic properties of axial tumors (4). The location of the tumor should thus be taken into consideration when estimating both prognosis and the value of treatment.
This case is unique as our patient presented with symptoms related to extra-skeletal axial Ewing sarcoma whilst pregnant. The concurrence of spinal tumors within pregnancy is particularly rare and requires alteration to routine therapeutic management (3,5). Based on the currently recognized treatment strategies, there would usually be three options by which the management of this patient would be approached (5). They include:
❖ Adhering to standard protocol, including chemotherapy, with the attendant risks to the foetus;
❖ Termination of the pregnancy followed by treatment;
❖ To await or advance delivery and commence treatment post-natally.
This case report thus provides an additional and unique approach to management of a pregnant patient with an axial tumor. It includes the decision not to terminate the pregnancy and to proceed with radical surgical intervention (complete resection) as the first line management option with delayed chemo- and radio-therapy.
The decision to proceed with urgent treatment of the axial tumor whilst in the second trimester of pregnancy was made based on a number of factors (5). Given that the patient presented at only 16-weeks’ gestation, postponing treatment until after delivery was not a viable option. Induction of delivery can be carried out at 32-weeks’ gestation or later and therefore 16 weeks of no therapy would have been inappropriate in the context of an aggressive malignancy (5). Whilst the underlying pathology of the mass is highly predictive of how rapid tumor growth will be, this remained unknown at the time of presentation and current imaging modalities remain unreliable to determine this (1,3). Thus, in the context of progressive and rapid development of motor weakness, it was deduced that the tumour of unknown origin was likely growing at a considerable rate and was of an aggressive nature. This may be partly explained by the changing hormonal milieu in pregnancy that may increase the potential for tumor growth (5). Moreover, given the axial location of the tumor, the severe degree of cauda equina compression and rapid motor deterioration, it was clinically evaluated as beneficial to proceed with urgent local therapy. In conjunction with this decision, strong consideration was made for the potential risk to the fetus associated with adjuvant therapies in early gestation and the patient’s wishes to achieve an uncomplicated and successful pregnancy (5).
Furthermore, the decision to pursue complete resection rather than partial resection is controversial, due to the known risks and complications of radical tumour resection within the sacral region (3). This decision was made based on numerous factors, which included the poor prognosis associated with extra-skeletal Ewing sarcoma (3). Particularly, 5-year survival rates have been reported to be 0% to 37.5% even with chemo- and radio-therapy (3). Such a poor prognostic outlook has been attributed to partial rather than complete resection and the subsequent tumor recurrence (3). Therefore, it seems that aggressive resection with less residual, as conducted in this situation, may give patients better outcomes. Additionally, with complete aggressive resection, it is expected that the usual progression of the tumor into the pelvis may be halted, allowing for an uncomplicated vaginal delivery without the need for caesarean (3).
The decision to treat with chemotherapy after aggressive resection was made following confirmation that the mass was chemo-sensitive. Given the knowledge that the ESFT dramatically respond to chemotherapy and that micro-metastases should be assumed in all cases, chemotherapy was indicated (1,2). Though, this practice is controversial in pregnancy due to the known risk of trans placental toxicity (5). Fortunately, as in this case, the risk in second trimester is dramatically decreased compared to the first trimester (5).
Radiation therapy was not considered whilst actively pregnant and is not recommended for use in pregnancy (5). It elicits adverse events in all phases of gestation and should particularly not be used for a tumor in the lumbar spine and sacrum due to the proximity to the fetus (5).
Conclusions
As the presentation of axial extra-skeletal Ewing sarcoma in pregnancy is unique, this case report provides a corresponding unique approach for treatment. Future similar cases could thus consider the use of early and complete aggressive surgical resection followed by chemotherapy prior to delivery.
Acknowledgements
Mr. Aidan McEvoy—Research Scientist, The Crown Princess Mary Cancer Centre, Westmead, NSW 2145, Australia; Healthscope Pathology, Bella Vista, NSW 2153, Australia; Nepean Radiology, Penrith, NSW 2751, Australia.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Javery O, Krajewski K, O'Regan K, et al. A to Z of extraskeletal Ewing sarcoma family of tumors in adults: imaging features of primary disease, metastatic patterns, and treatment responses. AJR Am J Roentgenol 2011;197:W1015-22. [Crossref] [PubMed]
- Bernstein M, Kovar H, Paulussen M, et al. Ewing's sarcoma family of tumors: current management. Oncologist 2006;11:503-19. [Crossref] [PubMed]
- Merimsky O, Le Chevalier T, Missenard G, et al. Management of cancer in pregnancy: a case of Ewing's sarcoma of the pelvis in the third trimester. Ann Oncol 1999;10:345-50. [Crossref] [PubMed]
- Hense HW, Ahrens S, Paulussen M, et al. Factors associated with tumor volume and primary metastases in Ewing tumors: results from the (EI)CESS studies. Ann Oncol 1999;10:1073-7. [Crossref] [PubMed]
- Meng T, Yin H, Li Z, et al. Therapeutic strategy and outcome of spine tumors in pregnancy: a report of 21 cases and literature review. Spine (Phila Pa 1976) 2015;40:E146-53. [Crossref] [PubMed]
- Al Khawaja D, Vescovi C, McEvoy A, et al. Two part video showing complete resection surgery of axial extra-skeletal Ewing sarcoma both macroscopically and microscopically. Asvide 2017;4:124. Available online: http://www.asvide.com/articles/1423


