Simultaneous anterior vertebral column resection-distraction and posterior rod contouring for restoration of sagittal balance: report of a technique
Introduction
Adult spinal deformity often presents with a patient suffering from significant sagittal imbalance. This is associated with incapacitating back pain, postural instability and symptoms related to neurogenic claudication. In severe cases, patients may progressively develop swallowing and/or speech dysfunction, gastroesophageal reflux disease and neurological deterioration. When such clinical presentations are accompanied by a lumbar curve of more than 30–40°, a lateral listhesis of 6mm or greater and a progressive curve (as measured on plain radiographs), patients may require surgical intervention (1).
Complications in deformity correction may be as high as 40 percent (2). A proportion of these complications can be related to inadequate sagittal balance correction. Consequently, pre-operative planning to determine the degree of correction, is required. This is important in order to ensure that adequate correction is achieved (2).
Various osteotomies have been described to correct such a deformity and in severe cases it is possible to perform a vertebral body resection to correct the alignment. In the thoracic spine this is possible from a posterior approach, but this can be difficult in selected lumbar cases due to the importance of preserving the lumbar nerve roots (3). Here, we describe a circumferential vertebral body resection, followed by simultaneous anterior inter-vertebral distraction and posterior in situ rod contouring, to achieve a large degree of sagittal balance.
Case presentation
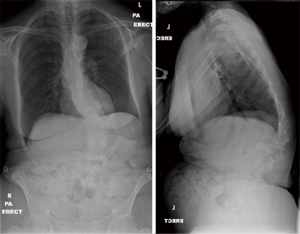
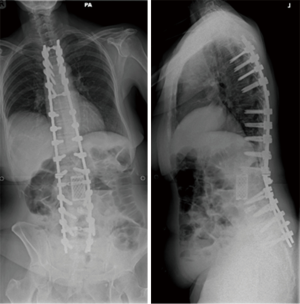
Case 1: A 62-year-old lady presented with a significant thoraco-lumbar curve with the apex at L1 and a Cobb angle of 40°. She complained of significant back pain, postural difficulty and an inability to perform daily tasks. She had no other significant co-morbidities (Figure 1).
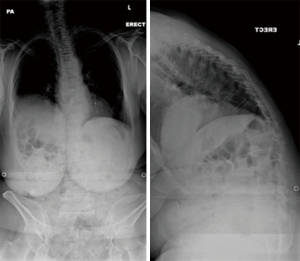
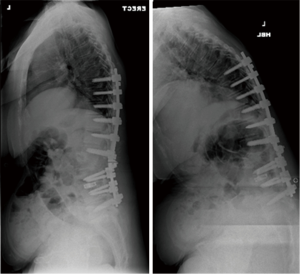
Case 2: A 69-year-old lady presented with a thoracolumbar curve and a history of previous spinal surgery in the form of a L2 pedicle subtraction osteotomy (PSO) and L3/4 posterior lumbar interbody fusion with instrumented fusion from T8 to L5 (Figure 2). Within 9 months of the index operation she developed significant back pain at the cranial end of the construct with development of kyphosis. She had resultant difficulty in walking, postural instability and symptoms suggestive of gastro- esophageal reflux disorder (Figure 3).
Both patients were initially treated non-operatively, but subsequently considered for surgical intervention after a detailed multi-disciplinary assessment. Radiographic parameters for both are shown in Table 1.
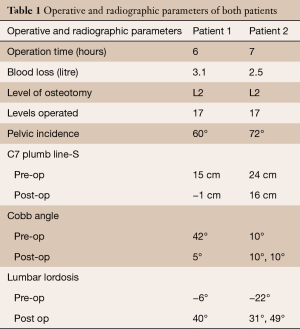
Full table
Surgical technique
Based on the analysis of the spino-pelvic balance using pre-operative radiographs, the degree of the correction required is determined and the level of osteotomy selected. The surgical steps are described below.
Stage 1: osteotomy
The patient is initially positioned prone and pressure areas are protected. Using a posterior midline approach, the osteotomy level is exposed. Pedicle screws are inserted at three spinal levels above and below the osteotomy site. At the level of the osteotomy, the dural sac and nerve roots are exposed by complete resection of posterior elements. Bilateral temporary rods are inserted. At this stage, it is important to place in situ benders underneath the temporary rods. This will facilitate contouring in Stage 2. The posterior wound is temporarily closed and covered with a waterproof dressing (Figure 4).
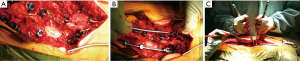
Stage 2: anterior distraction and posterior rod contouring
The patient is turned to the right lateral position (left side up), with a lateral retroperitoneal approach. The previously selected vertebral body and both adjacent intervertebral discs are exposed. The level is checked radiographically. The vertebral body and adjacent discs are excised; a 360° release is thus completed. An intervertebral spreader is inserted, with the flanges snugly fit on the endplates above and below. The posterior wound is now reopened. At this stage, the surgeon carries out contouring of the rods utilizing the previously applied in situ benders. An assistant applies anterior intervertebral distraction to assist posterior rod contouring, achieving maximum lordosis.
Once desired correction is achieved, a cage is impacted into the corpectomy site. This can either be an expandable or Moss cage filled with bone graft from the vertebral body. The temporary rods are tightened. Neuromonitoring is essential at this stage: a simultaneous anterior distraction and posterior rod contouring manoeuvre. The lateral retroperitoneal wound is closed in layers (Figure 5).
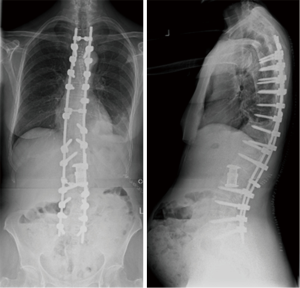
Stage 3: temporary rod exchange and closure
With the patient still in the right lateral position, temporary rods are exchanged and the whole construct is tightened. The posterior wound is then closed in layers (Figures 6,7).
Operating time and blood loss were 6 hours and 2.5Litres (L) for the first patient and 7 hours and 3L for the second patient. In the second patient, who had a previous PSO and metal work in situ, all the metal work was removed and the pedicle screws were replaced with larger diameter rescue screws to achieve better purchase.
Discussion
Glassman et al. showed that even a mildly positive sagittal balance can be detrimental and that symptom severity can directly increase in proportion to a progressive sagittal imbalance (4). The goal of adult spinal deformity surgery is restoration of both the sagittal and coronal balance. Sagittal balance restoration is more important as it facilitates decreased energy requirements on walking, improving cosmesis and patient satisfaction. It also limits pain, fatigue and complications associated with new or untreated deformities (5)
There are several recognized techniques which describe correction of a fixed sagittal imbalance (6-8). These include posterior only or anterior/posterior combined approaches, osteotomies such as the Smith-Peterson osteotomy (SPO), PSO and vertebral column resection (VCR). With regards to SPO, the amount of correction achievable is limited. SPO can also lengthen the anterior column with a risk of traction injury to the great vessels and pseudoarthrosis. PSO provides better correction, has superior mechanical stability and a high union rate. However, PSO can shorten the spinal column. Kawahara et al. studied the effect of acute shortening of the vertebral column on the spinal cord (9). When the spinal column is shortened by two thirds or more of a vertebral segment, the resultant effect is dural buckling and a reduction of the spinal cord blood flow. Although PSO provides better correction than SPO or chevron osteotomies, in severe sagittal imbalances it may not be sufficient. Schwab et al. reviewed sagittal realignment failures following PSO and suggested that a standard single level standard PSO may not achieve optimum outcome in patients with high pre-operative spino-pelvic mismatch. Such cases will require additional procedures beyond PSO (2).
The technique reported here allows for a greater degree of correction. Pre-operative planning requires careful analysis of the spino-pelvic and global sagittal balance. There are several important steps, which each require attention to detail.
Selection of osteotomy site
We believe that L2 allows easier access, through the retroperitoneal approach. If there is a resultant neurological deficit from the correction, it would involve the cauda equina rather than the conus or spinal cord. The L2 level is distal enough to achieve a greater degree of correction, but also proximal enough to achieve sufficient purchase distally. However, the choice of osteotomy level may be otherwise chosen by the type of curve requiring correction.
Pedicle screws
As this technique heavily relies upon pedicle screws for achieving correction, it is important to have adequate screw purchase. We recommend standard diameter screws, however rescue screws with or without cement augmentation may also be used as an alternative.
Correction manoeuver
During a pre-operative analysis of radiographs, one should aim to achieve a lumbar lordosis where pelvic incidence—lumbar lordosis <10 (PI-LL<10) and the C7 plum line (C7PL) falls through the posterior aspect of the sacrum. We recommend contouring a rod to the desired angle for use as a template, based on these pre-operative radiographs. This rod can then be sterilized and used as a guide during the operation.
During correction, there is a risk of stretching the spinal cord with subsequent vascular infarct and neurological consequences. We recommend multimodality neuromonitoring throughout the correction manoeuver (10).
Anterior column reconstruction
Corpectomy and posterior release provide a large amount of local bone. A bone graft-filled Moss or expandable cage enhances the fusion and provides a strong strut for anterior column reconstruction; the bone graft works optimally under compressive forces through the anterior column. The osteotomy site may be bridged using large struts or artificial substitutes.
Proximal and distal extension
We use a limited posterior approach in Stage 1 to minimize bleeding. If desired, the incision may be extended.
Temporary rod exchange
It is important to exchange the temporary rods due to the stress riser effect generated by the contouring forces.
Staging the procedure
All stages of this technique may be carried out in one sitting. However Stage 3 (rod exchange) may be scheduled for another day, depending on the intraoperative parameters of the patient.
Complications
One of the patients developed intestinal pseudo-obstruction on the 3rd post-operative day, subsequently receiving a diagnostic laparotomy. There were no other observed complications.
Post-operative care
We recommend post-operative intensive care management for 24–48 hours.
Summary
We report a technique which can be utilized in the correction of severe sagittal imbalance in adult deformity patients. The advantage of this technique is the potential to achieve a larger correction. As with all deformity correction there still remains the potential for complications. Attention to detail is thus required for each of the critical steps mentioned; every case needs to be considered on an individual basis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this mauscript and any accompanying images.
References
- Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010;28:E1. [Crossref] [PubMed]
- Schwab FJ, Patel A, Shaffrey CI, et al. Sagittal realignment failures following pedicle subtraction osteotomy surgery: are we doing enough?: Clinical article. J Neurosurg Spine 2012;16:539-46. [Crossref] [PubMed]
- Lenke LG, Sides BA, Koester LA, et al. Vertebral column resection for the treatment of severe spinal deformity. Clin Orthop Relat Res 2010;468:687-99. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-9. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013;22 Suppl 2:S254-64. [Crossref] [PubMed]
- Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. J Bone Joint Surg Am 2008;90:2509-20. [Crossref] [PubMed]
- Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine (Phila Pa 1976) 2006;31:S171-8. [Crossref] [PubMed]
- Kawahara N, Tomita K, Kobayashi T, et al. Influence of acute shortening on the spinal cord: an experimental study. Spine (Phila Pa 1976) 2005;30:613-20. [Crossref] [PubMed]
- Bhagat S, Durst A, Grover H, et al. An evaluation of multimodal spinal cord monitoring in scoliosis surgery: a single centre experience of 354 operations. Eur Spine J 2015;24:1399-407. [Crossref] [PubMed]