Duration of antibiotics for penetrating spine trauma: a systematic review
Introduction
Penetrating trauma to the spine represents a devastating injury that has achieved no consensus regarding management. Gunshot injuries are the third most common cause of such traumatic injuries to the spinal cord, following motor vehicle accidents and falls (1). While previous studies have focused on surgical debridement, decompression and stabilization of the spine as well as long-term antibiotics, no prospective randomized controlled trials exist regarding the proper treatment protocol to prevent spinal and paraspinal infections ranging from spinal epidural abscess to paravertebral osteomyelitis or disk space infection. Furthermore, earlier retrospective reviews regarding penetrating injuries to the spine based their management on high-velocity military assault rifles. Most penetrating spine injuries today are sustained from low-velocity civilian handguns which necessitate unique surgical and medical management, and the Center for Disease Control reports that 100,000 Americans are wounded by guns each year (1-3).
Uniform consensus exists that broad-spectrum antibiotics as well as tetanus prophylaxis should be administered as soon as possible following traumatic penetrating injury to the spine and spinal cord (2). However, the duration of antibiotics for such injuries remains a topic of controversy with no established protocol. Numerous authors have highlighted in retrospective reviews that viscus perforation and especially wounds that perforate the colon have a greatly increased infection risk that necessitates longer term antibiotic coverage. The goal of such antibiotic prophylaxis is to prevent deep infection of the spine (3).
Given the increased incidence of gun violence in the United States (3), establishing a protocol for duration of antibiotic protocol for penetrating injuries of the spine is imperative. Previous reports recommend 7–14 days of prophylactic antibiotics following such injuries (2). However, more recent retrospective studies have demonstrated that standard antimicrobial prophylaxis of 48 hours or less may be sufficient for minimizing infection risk in such patients without the role for extended antibiotic coverage (3). Given that there is no universally accepted practice regarding duration of antimicrobial coverage, the aim of this systematic review is to evaluate the rates of deep infection for patients with penetrating spine injuries. We present the article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/jss-20-451).
Methods
A search of three databases (PubMed, SCOPUS, and Ovid) was conducted to find articles that were relevant to this inquiry. The following keywords were used during literature searches: “penetrating spine trauma”, “spine infection”, and “spine trauma antibiotics.” Articles not in the English language were excluded from the search. Furthermore, articles that discussed spine-related infections such as epidural abscess and meningitis from mechanisms other than penetrating injury to the spine were excluded. Case reports and studies that did not report how long patients were placed on antibiotics were excluded from final analysis as they would not have data relevant to our inquiry.
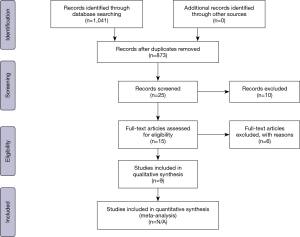
All nine of the studies that met eligibility criteria were retrospective reviews. Data was collected independently from the reports by two authors and was confirmed by each co-author. Literature searches and data collection to find appropriate studies were performed by two independent reviewers and followed the PRISMA guidelines as demonstrated in Figure 1. No randomized controlled trials or prospective studies were identified in a search of the literature. These studies were queried for number of patients, length of antimicrobial coverage, duration of follow-up, and incidence of deep infection of the spine. A difference in mean duration of antibiotics and number of infections were the primary outcome measures for this study. The mean duration of antibiotics was reported for each study.
Potential bias is inherent to any literature review and is also important to recognize in our systematic review. All studies included in this review are retrospective in nature and therefore have inherent flaws, such as sampling bias and confounding. Furthermore, they also lack control groups for comparison. Given the sampling bias of the retrospective reviews included in our study, they may lack generalizability to the general population as well.
Results
The initial literature searches of three databases returned 873 articles after all duplicates were removed. Searches using the keywords mentioned earlier returned numerous articles that discussed spine injuries that were not relevant to the systematic review and were subsequently excluded from analysis. Case reports were also excluded from final analysis. No prospective studies were found through an extensive literature search as well. Our final analysis included 9 studies, all of which were retrospective reviews from single institutions. The largest sample size belonged to a study by Simpson et al. in 1989 and included 160 patients, while the smallest sample size presented data from 20 patients (4,5).
The majority of studies included in final analysis discussed penetrating spinal trauma in the form of gunshot wounds (1-3). Only Simpson et al. discussed 18 patients who had stab wounds in their cohort of 160 patients (4). Furthermore, all studies included in analysis highlighted that patients in their sample sustained low-velocity gunshot injuries which often cause comparably less surrounding soft-tissue trauma compared to high-velocity injuries (6). Gunshot injuries from high-velocity military assault rifles and similar weapons are associated with much more significant soft tissue destruction as well as local tissue contamination (1-3), and this may be reflected by a higher incidence of infectious complications.
The minimum duration of antibiotics following penetrating spinal injury of the studies included in analysis was 24 hours (3). Pasulpuleti et al. described this as routine antimicrobial prophylaxis while anything longer than 48 hours was classified as extended antibiotic prophylaxis (7). Only Simpson et al. did not identify a specific duration, frequency, and dosage of antibiotics for their cohort of patients. Rabinowitz et al., Kihtir et al., Romanick et al. and Pasulpuleti et al. all described routine 48 hours of antibiotics and an infection rate of less than 5% in their patients (3,5,7,8). Furthermore, Lin et al. and Quigley et al. recommended a minimum of 5 days of antimicrobial prophylaxis given their findings while Kumar et al. and Roffi et al. demonstrated that patients had decreased infectious complications if they received at least 7 days of antibiotic prophylaxis (1,6,9,10). All of the included studies acknowledged that there are no guidelines for recommended antibiotic prophylaxis following penetrating spine injury. Treating surgeons either followed their institution’s protocol or did not provide details on how they decided what would be a reasonable duration of therapy given the extent of injury and whether patients developed additional infection unrelated to the spine (4-6).
When reporting incidence of infection in these studies, an important distinction needs to be made from spinal and paraspinal infections and those related to wound complications, abdominal injury, and operative intervention for hollow viscus trauma or gastrointestinal injury. The included studies classified spinal and paraspinal infections as those ranging from osteomyelitis, meningitis, disc space infection, epidural abscess, or paravertebral abscess (1-5,8,9). These do not include incidence of urinary tract infections, intra-abdominal abscess, abdominal wound complications, or peritonitis as many studies did not report how many patients had such complications following penetrating spine trauma. Furthermore, the included studies represented a variety of patients who had both operative intervention for intra-abdominal injuries requiring procedures such as a diverting colostomy and extensive wound debridement. Our systematic review focuses on the incidence of spinal and paraspinal infections in the studies included in analysis.
Overall, studies reported a low incidence of infections whether they used routine antimicrobial prophylaxis (48 hours) or extended prophylaxis for 7–14 days. The earliest study included by Roffi et al. reported that 3 of their 42 patients developed infection needing long-term antibiotics, and that 7 days of prophylaxis prevented infection in most patients (9). In 1985, Romanick et al. demonstrated that 7 of their 8 patients with trans-colonic injuries developed infection, and this correlated with earlier findings that injuries to the colon were associated with much higher infection risk that may necessitate extending antimicrobial coverage (5). However, antibiotics were only continued for 48–96 hours in this cohort, not the minimum of 5–7 days as recommended in later studies. Simpson et al. included the largest sample size in their retrospective review and found that only 4 patients out of 160 overall developed meningitis while another 4 developed unrelated wound complications. However, they did not report the duration of antibiotics for their patient population.
Later studies differed in their recommendations regarding duration of antimicrobial therapy. Kumar et al. demonstrated in their cohort of patients that none of the 13 patients who had gunshot injuries to the spine developed spinal or paraspinal infections after a course of antibiotics for 2 to 43 days (1). They recommended 7 days of broad-spectrum coverage to minimize infection. However, more recent studies published by Rabinowitz and Pasulpuleti demonstrate a very low risk of spinal infection with routine antimicrobial prophylaxis of only 24–48 hours (3,7). Both studies also demonstrate extended follow-up of 9–18 months as well. Previous studies have demonstrated that a mean of 6 months of follow-up is necessary for determining that a patient is free of infection ranging from meningitis, osteomyelitis, or epidural abscess (1,4-6).
As highlighted earlier, all studies included in our systematic review are retrospective in nature. As such, they are subject to both potential confounding and sampling bias. Our reported results should be viewed in the context of these potential areas of bias. Furthermore, duration of follow-up was not reported for most studies included in this systematic review.
Discussion
In penetrating injuries to the spine, bullets or other projectiles typically must travel through clothing, skin, and subcutaneous tissue before reaching the spine and potentially through the abdominal viscus and hollow organs if traversing the anterior viscera (1). Therefore, potential for contamination remains elevated especially with such high-energy injuries. Several studies have also demonstrated that colonic perforation is associated with the highest incidence of infection ranging from osteomyelitis, epidural abscess, and disc space infection (2,3,8). And while earlier recommendations demonstrated lowest infection risk with 7–14 days of broad-spectrum coverage of gram-positive, gram-negative, and anaerobic organisms, these were often based on higher-velocity injuries from military rifles that often caused more significant soft tissue contamination and were associated with higher potential for deep space infection. Given the current push in medicine to combat the increased prevalence of antibiotic resistant organisms and the costs associated with treating such organisms, it is imperative to clarify the lowest amount and duration of antimicrobial coverage that would reduce infection from penetrating injuries to the spine (7).
Adequate duration of antibiotics following such injuries becomes even more critical when discussing the limited role for surgical irrigation and debridement. Kihtir et al., Lin et al., and Roffi et al. all demonstrated favorable outcomes regarding limiting spinal infection in patients who had extended antibiotics and nonoperative management of such injuries (6,8-11). However, any spinal instability or neurologic injury usually portends poor prognosis without operative intervention for surgical stabilization of the spine. Surgical intervention to the spine is also not without complications including CSF leakage, wound complications, and meningitis as numerous studies included in our analysis demonstrated (2,6).
Management of penetrating orthopaedic trauma to areas other than the spine also warrants consideration for guiding management in spine trauma as such injuries occur with greater frequency and have more established protocols for care (12). Current literature recommends superficial debridement with antibiotic administration for extremity trauma following low-velocity gunshot injuries that do not present with vascular compromise, gross contamination, or massive soft tissue injury (13). Furthermore, low-velocity ballistic injuries may also be managed solely with antibiotic administration, while high-velocity ballistic injuries as well as those involving bowel injuries may necessitate surgical debridement in addition to antibiotics (12). A systematic review on gunshot-induced fractures of the extremities by Sathiyakumar et al. also found equivalent efficacy in patients treated with oral ciprofloxacin and intravenous (IV) cephalosporin plus gentamicin, with an infection rate of 1.8% for low-velocity non-operative fractures (12). The majority of studies included recommended brief hospitalization with IV antibiotics followed by a 7-day course of oral antibiotics as an outpatient (12,13). None of the included articles in our systematic review discuss whether oral or IV antibiotics are optimal and which class of drug is ideal for penetrating spine trauma (Table 1).
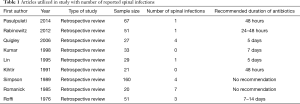
Full table
Our study puts into perspective the available information regarding duration of antibiotics following penetrating injuries to the spine. It is important to note that no prospective study exists regarding this topic and all the studies included in our systematic review are retrospective in nature. However, all of the aforementioned studies have an extended follow-up of at least 6 months, which is sufficient to detect any spinal infection (1,4-6,14,15). Several important conclusions can be drawn regarding the results presented. Romanick et al. demonstrated the highest percentage of patients developing spinal infections (35%) and noted that each of them had a trans-colonic gunshot injury (5). However, several of these patients also only had antibiotics continued for 48–96 hours, and others received them for 5 days or more. The authors do not make any specific recommendations regarding duration of therapy though this study is often cited as evidence supporting extended antibiotic prophylaxis.
Subsequent studies recommended anywhere from 5–14 days of broad-spectrum coverage for spine injuries that involved the colon (5,6,10). Lin et al. and Kumar et al. recommended 5 and 7 days of antimicrobial coverage given their low incidence of infection in their cohorts. However, though Lin et al. recommended a 5-day course of antibiotics, their patients only received 48 hours of antibiotics unless another source of infection was identified (1-10). Therefore a 5-day course of therapy would not be empirically indicated given their findings. Kumar et al. recommended 7 days of therapy as no patients in their group developed spinal or paraspinal infections after such a prolonged course. However, they also made no mention of adverse effects of prolonged antibiotic therapy and the potential to develop resistance. Quigley et al. also recommended 5 days of coverage given that 3 of the 19 (15.8%) patients in their group receiving what they described as inadequate coverage (less than 5 days) developed while only 1 of 8 (12.5%) patients in the adequate coverage (5 days of therapy) group developed spinal infection. However, this was not a statistically significant difference (P=0.74) and it is unclear how 5 days was deemed adequate coverage (3,6).
Our systematic review finds that while an extended duration of antimicrobial prophylaxis of greater than 48 hours may be advisable in patients who have trans-colonic gunshot injuries, it may not be necessary in patients who do not have such involvement following penetrating spinal trauma. Pasulpuleti et al. and Rabinowitz et al. had cohorts of 67 patients and 51 patients, respectively, with only one patient in each group developing a central nervous system infection. All patients in their groups received standard prophylactic antibiotics of 48 hours or less following penetrating spinal injury (3,7). The one patient who developed meningitis in the study by Pasulpuleti et al. also had already received a prolonged 2-week course of piperacillin-tazobactam and developed late meningitis following recurrent bacteremia. Therefore, in these two more recent studies the authors find no evidence supporting therapy longer than the 48-hour prophylactic antibiotic course (7). Kihtir et al. also found that a 48-hour course of antimicrobial prophylaxis was sufficient in preventing infection in all 21 of their patients along with the standard irrigation and debridement of the missile track (8).
The conclusions of our review should be put into context with the limitations of conducting such an analysis with only retrospective studies. As no prospective studies on the subject of penetrating injuries to the spine are currently available, it is not possible to make definitive treatment recommendations or establish guidelines. Furthermore, studies highlighted in this review varied significantly in terms of type of penetrating trauma that patients sustained and duration of follow-up, and did not report what type of antibiotics were administered (1-6,9). Given the heterogeneity of these studies, it is important to consider that factors such as age and co-morbidities, associated injuries, class of antibiotics, and administration of oral versus intravenous antibiotics are all potential confounders that lie outside the scope of available information from these studies. Future prospective studies on optimal duration of antibiotics for penetrating spine trauma would address many potential confounders and may provide stronger recommendations for treatment.
Conclusions
Our systematic review finds that penetrating injuries to the spine can be associated with serious spinal and paraspinal infections, however most penetrating spinal injuries are not associated with such infection. And despite concerns for contamination with concomitant injury to the gastrointestinal tract, these injuries can often undergo nonoperative management with antimicrobial prophylaxis. While no definitive recommendations can be made regarding duration of prophylaxis given the retrospective nature of studies included in this systematic review, more recent studies have demonstrated the efficacy of 48 hours of standard antimicrobial prophylaxis to cover gram-positive, gram-negative, and anaerobic organisms. However, patients with trans-colonic injuries may benefit from an extended course of antibiotics given the potential greater risk for spinal and paraspinal infection. Future prospective studies examining the optimal duration of antibiotics for penetrating spine trauma may help guide clinicians by establishing more definitive recommendations that are not possible to ascertain through this study given that all currently published literature is retrospective in nature,
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. (Available at http://dx.doi.org/10.21037/jss-20-451).
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/jss-20-451). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kumar A, Wood GW, Whittle AP. Low-velocity gunshot injuries of the spine with abdominal viscus trauma. J Orthop Trauma 1998;12:514-7. [Crossref] [PubMed]
- Bono CM, Heary RF. Gunshot wounds to the spine. Spine J 2004;4:230-40. [Crossref] [PubMed]
- Rabinowitz RP, Tabatabai A, Stein DM, Scalea TM. Infectious complications in GSW's through the gastrointestinal tract into the spine. Injury 2012;43:1058-60. [Crossref] [PubMed]
- Simpson RK, Venger BH, Narayan RK. Treatment of acute penetrating injuries of the spine: a retrospective analysis. J Trauma 1989;29:42-6. [PubMed]
- Romanick PC, Smith TK, Kopaniky DR, et al. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am 1985;67:1195-201. [Crossref] [PubMed]
- Quigley KJ, Place HM. The role of debridement and antibiotics in gunshot wounds to the spine. J Trauma 2006;60:814-9. [Crossref] [PubMed]
- Pasupuleti LV, Sifri ZC, Mohr AM. Is extended antibiotic prophylaxis necessary after penetrating trauma to the thoracolumbar spine with concomitant intraperitoneal injuries? Surg Infect (Larchmt) 2014;15:8-13. [Crossref] [PubMed]
- Kihtir T, Ivatury RR, Simon R, et al. Management of transperitoneal gunshot wounds of the spine. J Trauma 1991;31:1579-83. [Crossref] [PubMed]
- Roffi RP, Waters RL, Adkins RH. Gunshot wounds to the spine associated with a perforated viscus. Spine 1989;14:808-11. [Crossref] [PubMed]
- Lin SS, Vaccaro AR, Reisch S, et al. Low-velocity gunshot wounds to the spine with an associated transperitoneal injury. J Spinal Disord 1995;8:136-44. [Crossref] [PubMed]
- Kitchel SH. Current treatment of gunshot wounds to the spine. Clin Orthop Relat Res 2003.115-9. [Crossref] [PubMed]
- Sathiyakumar V, Thakore RV, Stinner DJ, et al. Gunshot-induced fractures of the extremities: a review of antibiotic and debridement practices. Curr Rev Musculoskelet Med 2015;8:276-89. [Crossref] [PubMed]
- Nguyen MP, Savakus JC. Infection Rates and Treatment of Low-Velocity Extremity Gunshot Injuries. J Orthop Trauma 2017;31:326-9. [Crossref] [PubMed]
- Heiden JS, Weiss MH, Rosenberg AW, et al. Penetrating gunshot wounds of the cervical spine in civilians. Review of 38 cases. J Neurosurg 1975;42:575-9. [Crossref] [PubMed]
- Ivatury RR, Zubowski R, Psarras P, et al. Intra-abdominal abscess after penetrating abdominal trauma. J Trauma 1988;28:1238-43. [Crossref] [PubMed]