Survey of lumbar discectomy practices: 10 years in the making
Introduction
Lumbar discectomy is a common neurosurgical procedure. Nearly 300,000 operations are performed annually in the USA (1). The North American Spine Society (NASS) has provided grade B recommendation that earlier surgery (within 6 months to 1 year) is associated with faster recovery and improved long-term outcomes (2). The SPORT trial indicated that surgery for lumbar disc herniation provides superior long-term results in comparison to conservative treatment (3). Variability exists among neurosurgeons in pre-, intra- and post-operative management strategies with lumbar discectomy. In 2007, the authors A Cenic and E Kachur conducted a questionnaire survey to measure differences in practice between neurosurgeons in Canada (4). We repeated the survey conducted in 2007 to assess and compare changes in practice patterns among neurosurgeons in Canada over 10-year period. We present the following survey in accordance with the SURGE reporting checklist (available at: http://dx.doi.org/10.21037/jss-20-519).
Methods
This study design was a cross-sectional survey of neurosurgeons in Canada. A 17-item questionnaire was distributed electronically to neurosurgeons practicing in Canada using the REDCap online platform. This 17-item questionnaire was created, tested and used in 2007. A list of certified neurosurgeons was obtained from the Royal College of Physicians and Surgeons of Canada. Contact information, e-mail addresses and fax numbers for the neurosurgeons was collected from previously existing distribution lists and publicly accessible websites, particularly neurosurgical department websites from academic institutions. Contact information for 249 neurosurgeons practicing in Canada was identified. Survey invitations were sent out electronically by A Martyniuk and E Kachur with several electronic reminders. For those who did not respond, or no e-mail address was identified, an invitation was faxed. No incentives (financial or other) were offered to neurosurgeons who received the survey. The research was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Research ethics approval was not required as per our institutional research ethics board. Participants have completed and submitted the survey implied consent.
The following questions were included in the survey:
- Number of years in practice?
- Do you perform Lumbar Discectomy(s) in your practice?
- Is your practice predominantly: adult, pediatric or both?
- Do you have a spine fellowship?
- Do you use pre-incision localizing plain film X-ray?
- What is your favorite preoperative imaging?
- Do you use preoperative antibiotics?
- Do you use pre-incision local anesthetic injection?
- Intramuscular local anesthetic injection prior to closure?
- What is your magnification preference?
- Do you use tubular retractors (e.g., METRx® system, Sofamor-Danek, Memphis, TN, USA)?
- For dural tears, do you use fibrin glue (e.g., Tisseel®, Baxter, Deerfield, IL, USA)?
- Prior to closure, do you use fat graft?
- Do you use epidural steroids prior to closure?
- If there are no complications, when do you discharge from hospital?
- If patient’s job requires physical labour, when do you recommend a post-operative return to work?
- Would you operate on a patient whose major complaint is back pain?
Descriptive statistics were reported using counts and percentages. Group differences in response rates for each question were assessed using Chi-square Goodness-of-fit test assuming no difference in response between the categories. Differences in responses between the two surveys (2017 and 2007) were assessed using Chi-square or Fisher’s exact test. The statistical significance was achieved with a P value ≤0.05. SPSS statistical software version 25 (www.IBM.com) was used for analysis.
Results
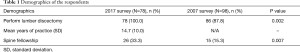
Of the 249 Canadian neurosurgeons invited to participate in the survey, 109 responded, resulting in a 43.8% response rate. This was lower than the 64.4% response rate in 2007 (112 responses from 174 potential participants). Of the 109 respondents, 83 (76.1%) reported their predominant neurosurgical practice group (adult and/or pediatric). The analysis included only 78 responses that indicated their practice was adult only [76] or both adult and pediatric [2], compared to 98 in 2007. All 78 participants in 2017 performed lumbar discectomy in their practice, in comparison to 87.8% in 2007 (P=0.002). There was a significant increase in the number of neurosurgeons that had a spine fellowship in 2017 from 2007 (33.3% in 2017 vs. 15.3% in 2007; P=0.007). The average number of years of practice for the 2017 participants was 14.7 years. Table 1 demonstrates the demographics of the respondents. Table 2 demonstrates the results of the 2017 survey and Table 3 shows a comparison of the 2007 and 2017 surveys.
Full table
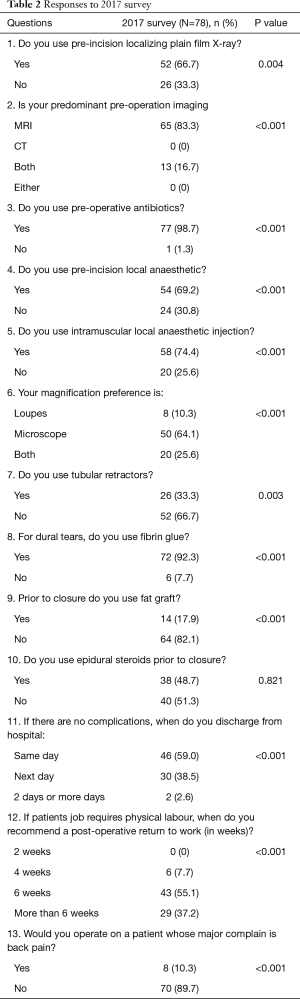
Full table
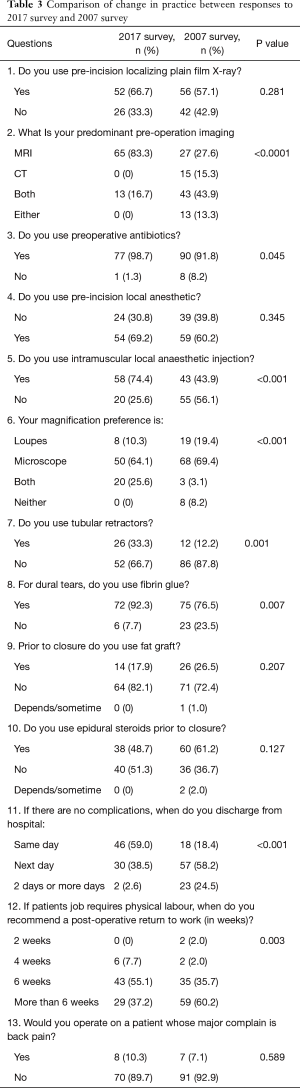
Full table
Imaging
There was a significant difference in regards to the radiological modality of choice in 2017 for pre-operative diagnosis and planning, 83.3% preferred magnetic resonance imaging (MRI) while 16.7% used both MRI and computed tomography (CT), and no one predominantly used CT alone (P<0.001). This has significantly changed from 2007, when MRI was used predominantly by only 27.6% of surgeons, CT by 15.3%, 43.9% used both, and 13.3% used either (P<0.001). The majority of respondents (66.7%, P<0.05) used a pre-incision localization plain film X-ray, not significantly changed from the previous study (57.1%; P=0.281).
Use of intraoperative local anesthetic
Most neurosurgeons in the survey (69.2%; P<0.001) used a pre-incision local anesthetic, consistent with 60.2% in the previous survey (P=0.345). The practice of intra-muscular local anesthetic injection has significantly changed with 74.4% of the current survey respondents reporting using it, compared to only 43.9% in the 2007 study (P<0.001).
Peri-operative antibiotics
Nearly all the surgeons (98.7%, P<0.001) use pre-operative antibiotics in the 2017 survey. This has significantly increased from an already high rate in 2007 (91.8%; P<0.05).
Epidural fat and steroids
According to the current analysis, the practice of placing a fat graft over the exposed nerve root has not significantly changed over the past decade (26.5% in 2007 vs. 17.9% in 2017; P=0.207). Regarding the use of epidural steroids before closure, the practice continues to be split with 48.7% using them in 2017 and 61.2% in 2007 (P=0.127).
Discharge and return to work
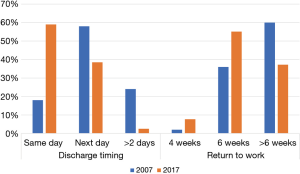
The majority of respondents (59.0%) discharge their patient the same day of surgery, in the absence of complications, while 38.5% discharge the next day, and 2.6% discharge 2 days or later (P<0.001). This is statistically different from the previous survey where only 18.4% would discharge on the same day, 58.2% the next day, and 24.5% 2 days or later (P<0.001) (Figure 1). With respect to return to work, if patient’s job requires physical labor, 55.1% of participants would recommend return to work in 6 weeks, 37.2% more than 6 weeks, and 7.7% in 4 weeks (P=0.001). This has significantly changed compared to the 2007 survey, when the majority of surgeons (60.2%) would recommend return to work after more than 6 weeks and only 35.7% at 6 weeks (P<0.05) (Figure 1).
Technical aspects
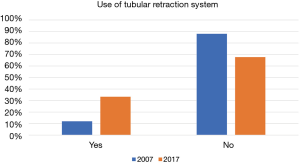
With respect to the intraoperative magnification of choice, 64.1% used microscope, 10.3% loupes, and 25.6% use both (P<0.001). This has significantly changed from the in 2007 survey where, 69.4% used microscope, 19.4% loupes, 3.1% both, and 8.2% neither (P<0.001). The use of minimally invasive tubular retractor systems (e.g., METRx®) has become more popular as shown by the current survey (33.3% yes in 2017 vs. 12.2% yes in 2007; P=0.001) (Figure 2). In case of dural tears, there is a significantly increased utility of fibrin glue (e.g., Tisseel®) as 92.3% responded yes in 2017 compared to 76.5% in 2007 (P=0.007).
Surgical indications
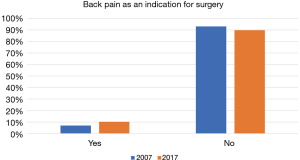
Most surgeons (89.7%) will not operate on patients whose major complaint is back pain (P<0.001). There has not been a significant change in this practice over the past decade (89.7% in 2017 vs. 92.9% in 2007, P=0.589) (Figure 3).
Discussion
In this study we examined the multitude of variables in the surgical management of lumbar disc herniation. The present study is the first in the literature to assess lumbar discectomy management at 2 distinct periods of time. Studies in the literature have explored individual aspects of the questions presented in our surveys. The incidence of surgical site infection (SSI) in lumbar discectomy surgery is reported as less than 1% (5). In our recent survey, nearly all respondents support the use of pre-incisional antibiotics for lumbar discectomy. The practice of peri-operative antibiotic prophylaxis has been recommended by the Centers for Disease Control and Prevention (CDC) guidelines to reduce SSI (6). In a retrospective study by Kanayama et al. including 1,597 patients, a single dose of preoperative antibiotics was found to be equally effective when compared to multiple doses (7).
Both the recent and previous survey showed that the majority of neurosurgeons in Canada are using pre-incision local anesthetic agents. A significant increase in the use of local anesthetic intra-muscularly prior to wound closure was seen in the present survey. This practice is well-described in the literature to reduce post-operative pain (8). A recent meta-analysis of 11 prospective randomized trials showed reduction in postoperative analgesic requirements, prolonged time to first analgesic demand and reduced visual analogue score (VAS) score at 1 hour post-operatively was associated with use of intra-muscular local anesthesia in lumbar spine patients, the majority of whom underwent lumbar microdiscectomy (9). A prospective, blinded, placebo-controlled study by Yörükoglu et al. was conducted to compare the postoperative analgesic efficacy of low-dose intrathecal and epidural morphine with paraspinal muscle infiltration of bupivacaine in lumbar discectomy patients (10). The trial showed that low-dose intrathecal and epidural morphine was associated with more post-operative pain control and lower analgesic requirements with no increase in the side effects.
MRI has been shown to be a superior test for accurately pre-operatively predicting a lumbar disc herniation vs. CT and CT-myelogram (11). In the recent survey, MRI was the modality of choice among the majority of neurosurgeons in Canada. There was a significant increase in the utility of MRI as the preferred pre-operative imaging modality. Wittenberg found that preoperative MRI is highly correlated with intraoperative findings of structural changes in the lumbar disc, in terms of nerve root compression by the disc and the presence of free disc sequestration or subligamentous extrusion (12).
Both of our surveys found the microscope to be the dominant tool used in lumbar microdiscectomy. However, the recent survey found more combined usage of microscope and loupes vs. individual use of each in the previous survey. Kumar et al. found improved clinical outcomes with the use of the microscope vs. magnifying loupes for patients undergoing single level unilateral microdiscectomy and microdecompression (13). In the consecutive case series of 51 patients per group, microscope vs. loupes, patients in the microscope group had significantly improved satisfaction scores and VAS for pain, but not complication rates. In his retrospective analysis of the American College of Surgeons National Surgical Quality Improvement (ACS-NSQIP) database for elective spinal procedures, Basques et al. analyzed spinal procedures with and without operating microscope for the years 2011 and 2012 (14). No significant difference in 30-day infection rates occurred between the microscope and non-microscope groups. The use of microscope was associated with minor increase in total operating room time.
Bioglue or fibrin glue are both safe and effective dural sealants in non-instrumented lumbar spine surgeries (15). Jankowitz et al. performed a retrospective analysis of 4,835 lumbar spine procedures for a 10-year period. Five hundred and forty-seven patients (11.3%) experienced a durotomy during surgery and fibrin glue was used in approximately half of these cases (50.8%) to assist in the repair. There was no statistical difference in the post-operative cerebrospinal fluid (CSF) leak rate between cases in which fibrin glue was or was not used (16). In a survey of spinal dural repair to the Canadian Neurologic Surgical Society, Oitment et al. found a sealant was used in 36.7% of cases for a pin hole durotomy and up to 80% for a large size tear. The majority used Tisseel (80%) as their preferred sealant (17). Our survey demonstrated significant increase in utility of fibrin glue over the past 10 years.
Epidural fat grafts have been placed over the dural sac and nerve root following lumbar microdiscectomy in an effort to prevent chronic pain from epidural fibrosis and scar formation which may cause nerve root tethering and irritation (18). Our survey detected no significant change regarding this practice. In a study by Dobran et al., lumbar microdiscectomy patients were randomized into two groups, with fat graft (N=18) and those without (N=18). No difference was shown in VAS or Oswestry Disability Index (ODI) post-operatively at 1 and 6 months (19). Our study showed a trend away from fat graft usage. It is possible that no change in the use of fat graft in our survey occurred because of the lack of evidence in the literature to support this practice.
In our survey, half the respondents are using epidural steroid in an effort to decrease post-operative pain. In a systemic review and meta-analysis of epidural steroid use in lumbar discectomy, Akinduro et al. found supportive evidence of decrease short term post-operative pain and narcotic use. However, there was a trend toward increased infections with epidural steroid use at 0.94% [epidural steriod (ES)] vs. 0.08% (no ES), P=0.10 (20). In a retrospective cohort trial of epidural steroid application to the decompressed nerve, lumbar microdiscectomy patients (N=53) showed less disability on the Roland-Morris Disability Index and health-related quality of life health survey on post-operative day 3 and at 6 weeks vs. matched control patients not receiving epidural steroids. However, the author noted that the group differences were lower than the commonly accepted minimally important clinical difference for each metric (21).
The recommendation to restrict activities and return to work usually vary based on the nature of the job. In the recent survey more surgeons recommended a faster return to work vs. the previous survey. The prevailing recommendation in the 2017 survey was to return to work at 6 weeks, instead of more than 6 weeks, as recommended in the 2007 survey. A randomized control trial suggested no difference in clinical outcome or re-herniation rate with activity restriction for 2 vs. 6 weeks (22). A prospective study by Carragee et al. of 152 patients with no post-operative activity restrictions found an average work loss of 1.2 weeks and return to full activity after 8 weeks (23). In an Australian survey addressing peri-operative management of lumbar discectomy, 52.9% of respondents would recommend lifting restriction for 4–8 weeks (24). Written post-operative instruction sheets could be helpful to avoid complications.
There is a new trend among neurosurgeons in the current survey to discharge their patient on the same day of surgery in the absence of a complication compared to the first post-operative day in 2007 study (Figure 1). In a survey by Zoia et al., most of the respondents discharge their patients within the next 2 days postoperatively (8). The literature support early discharge in cases of good pain control and no complications, such as CSF leak (25).
Minimally invasive spinal surgery (MIS) has increased in popularity over the last decade due to its benefits in decreasing length of stay in hospital and cost associated with the procedure. Additionally, it has been shown to have lower rates of SSI (26,27). However, MIS might pose higher rate of recurrent disc herniation (28). Our survey demonstrates more neurosurgeons are using minimally invasive spine techniques (tubular retractors) in their practice (33.3% compared to 12.2%) (Figure 2).
The majority of Canadian neurosurgeons in our survey do not consider back pain as an indication to perform lumbar discectomy (89.7%), not significantly different from the last survey (92.9%) (Figure 3). There is a common belief among neurosurgeons that lumbar discectomy is not an effective treatment to treat low back pain in the absence of sciatica. This is contrary to several studies in the literature who investigated this question. In a prospective pilot study by Chin et al., patients with low back pain and sciatica with and without Modic changes were followed after lumbar discectomy. It was reported that both sciatica and low back pain have improved significantly at 6 months and 1 year follow-up in term of VAS and ODI (29).
Our survey has several limitations. Firstly, only neurosurgeons practicing in Canada were surveyed so the results are not necessarily generalizable to other countries. Secondly, the response rate was 43% therefore non-responders bias should be considered when interpreting the results of the survey. In our study, a 17-item questionnaire was used in order to ascertain practise patterns among Canadian neurosurgeons regarding the peri-operative management of lumbar microdiscectomy. We also intended to detect possible changes in practice over a period of 10 years. A trend toward earlier home discharge, sooner return to work and more utility of tubular retractor systems have been identified as changes over the past decade. Thus, having the impact of lumbar discectomy surgery lessened on a person’s life. Randomized controlled trails would be helpful to provide evidences regarding which practice is associated with better outcomes and help standardize the lumbar discectomy procedure.
Acknowledgments
Portions of this work were presented in abstract form at the annual meeting of the North American Spine Society (NASS), September 2018.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-519
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jss-20-519
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-519). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The research was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Research ethics approval was not required as per our institutional research ethics board. Participants have completed and submitted the survey implied consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parker SL, Xu R, McGirt MJ, et al. Long-term back pain after a single-level discectomy for radiculopathy: incidence and health care cost analysis. J Neurosurg Spine 2010;12:178-82. [Crossref] [PubMed]
- Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014;14:180-91. [Crossref] [PubMed]
- Lurie JD, Tosteson TD, Tosteson AN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. 2015;40:E59. Spine (Phila Pa 1976) 2014;39:3-16. [Crossref] [PubMed]
- Cenic A, Kachur E. Lumbar discectomy: a national survey of neurosurgeons and literature review. Can J Neurol Sci 2009;36:196-200. [Crossref] [PubMed]
- Rohde V, Meyer B, Schaller C, et al. Spondylodiscitis after lumbar discectomy: incidence and a proposal for prophylaxis. Spine (Phila Pa 1976) 1998;23:615-20. [Crossref] [PubMed]
- Mangram AJ, Horan TC, Pearson ML, et al. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control 1999;27:97-132. [Crossref] [PubMed]
- Kanayama M, Hashimoto T, Shigenobu K, et al. Effective prevention of surgical site infection using a Centers for Disease Control and Prevention guideline–based antimicrobial prophylaxis in lumbar spine surgery. J Neurosurg Spine 2007;6:327-9. [Crossref] [PubMed]
- Zoia C, Bongetta D, Poli JC, et al. Intraregional differences of perioperative management strategy for lumbar disc herniation: is the Devil really in the details? Int J Spine Surg 2017;11:1. [Crossref] [PubMed]
- Perera AP, Chari A, Kostusiak M, et al. Intramuscular local anesthetic infiltration at closure for postoperative analgesia in lumbar spine surgery: A systematic review and meta-analysis. Spine (Phila Pa 1976) 2017;42:1088-95. [Crossref] [PubMed]
- Yörükoğlu D, Ates Y, Temiz H, et al. Comparison of low-dose intrathecal and epidural morphine and bupivacaine infiltration for postoperative pain control after surgery for lumbar disc disease. J Neurosurg Anesthesiol 2005;17:129-33. [Crossref] [PubMed]
- Janssen ME, Bertrand SL, Joe C, et al. Lumbar herniated disk disease: comparison of MRI, myelography, and post-myelographic CT scan with surgical findings. Orthopedics 1994;17:121-7. [PubMed]
- Wittenberg RH, Lütke A, Longwitz D, et al. The correlation between magnetic resonance imaging and the operative and clinical findings after lumbar microdiscectomy. Int Orthop 1998;22:241-4. [Crossref] [PubMed]
- Kumar SS, Mourkus H, Farrar G, et al. Magnifying loupes versus microscope for microdiscectomy and microdecompression. J Spinal Disord Tech 2012;25:E235-9. [Crossref] [PubMed]
- Basques BA, Golinvaux NS, Bohl DD, et al. Use of an operating microscope during spine surgery is associated with minor increases in operating room times and no increased risk of infection. Spine (Phila Pa 1976) 2014;39:1910-6. [Crossref] [PubMed]
- Miscusi M, Polli FM, Forcato S, et al. The use of surgical sealants in the repair of dural tears during non-instrumented spinal surgery. Eur Spine J 2014;23:1761-6. [Crossref] [PubMed]
- Jankowitz BT, Atteberry DS, Gerszten PC, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J 2009;18:1169-74. [Crossref] [PubMed]
- Oitment C, Aref M, Almenawar S, et al. Spinal dural repair: a Canadian questionnaire. Global Spine J 2018;8:359-64. [Crossref] [PubMed]
- Chin KR, Bassora R, Yu WD. Safety and usefulness of free fat grafts after microdiscectomy using an access cannula: a prospective pilot study and literature review. Am J Orthop (Belle Mead NJ) 2014;43:66-9. [PubMed]
- Dobran M, Brancorsini D, Costanza MD, et al. Epidural scarring after lumbar disc surgery: Equivalent scarring with/without free autologous fat grafts. Surg Neurol Int 2017;8:169. [Crossref] [PubMed]
- Akinduro OO, Miller BA, Haussen DC, et al. Complications of intraoperative epidural steroid use in lumbar discectomy: a systematic review and meta-analysis. Neurosurg Focus 2015;39:E12. [Crossref] [PubMed]
- Stienen MN, Joswig H, Chau I, et al. Efficacy of intraoperative epidural triamcinolone application in lumbar microdiscectomy: a matched-control study. J Neurosurg Spine 2018;28:291-9. [Crossref] [PubMed]
- Bono CM, Leonard DA, Cha TD, et al. The effect of short (2-weeks) versus long (6-weeks) post-operative restrictions following lumbar discectomy: a prospective randomized control trial. Eur Spine J 2017;26:905-12. [Crossref] [PubMed]
- Carragee EJ, Helms E, O'Sullivan GS. Are postoperative activity restrictions necessary after posterior lumbar discectomy?: a prospective study of outcomes in 50 consecutive cases. Spine (Phila Pa 1976) 1996;21:1893-7. [Crossref] [PubMed]
- Daly CD, Lim KZ, Ghosh P, et al. Perioperative care for lumbar microdiscectomy: a survey of Australasian neurosurgeons. J Spine Surg 2018;4:1-8. [Crossref] [PubMed]
- Khan MH, Rihn J, Steele G, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006;31:2609-13. [Crossref] [PubMed]
- Evaniew N, Khan M, Drew B, et al. Minimally invasive versus open surgery for cervical and lumbar discectomy: a systematic review and meta-analysis. CMAJ Open 2014;2:E295-305. [Crossref] [PubMed]
- McClelland S 3rd, Goldstein JA. Minimally Invasive versus Open Spine Surgery: What Does the Best Evidence Tell Us? J Neurosci Rural Pract 2017;8:194-8. [Crossref] [PubMed]
- Belykh E, Giers MB, Preul MC, et al. Prospective Comparison of Microsurgical, Tubular-Based Endoscopic, and Endoscopically Assisted Diskectomies: Clinical Effectiveness and Complications in Railway Workers. World Neurosurg 2016;90:273-80. [Crossref] [PubMed]
- Chin KR, Tomlinson DT, Auerbach JD, et al. Success of lumbar microdiscectomy in patients with modic changes and low-back pain: a prospective pilot study. J Spinal Disord Tech 2008;21:139-44. [Crossref] [PubMed]