The effect of increasing body mass index on the pain and function of patients with adult spinal deformity
Introduction
Adult spinal deformity (ASD) is a condition of variable causes resulting in spinal malalignment in the frontal and/or sagittal plane. ASD is estimated to affect up to 30% of people aged over 50 years and 68% of those aged over 70 years (1). Despite this high rate, many patients may have little to no symptoms, but others can be severely symptomatic and debilitated (2). To date, a complete understanding of which factors influence patient symptoms remains unclear.
It is well recognised that sagittal balance directly affects functional outcomes in patients with ASD (3,4). But it is also known that many factors influence back pain and function in the general population, including geographic, psychosocial factors, physical and genetic factors (5-9). Yet the effect of these factors in ASD remain unclear. Of note, despite the rates of obesity increasing internationally, the effect of body mass index (BMI) on the pain and function of patients with ASD remains unknown (10,11). To date there is no literature examining the effect of BMI in this patient group, yet the authors of this study believe that BMI is a modifiable factor that may influence the pain, function and quality of life of patients affected by ASD.
Large data analytics on prospective patient cohorts allows us to develop a greater understanding of the factors involved in pain and functional outcomes of these patients. Thus, the purpose of this study was to examine a large multicentre European database to determine whether BMI has an independent effect on the pain and function of patients with ASD.
Methods
Study design
We performed a retrospective review of the prospectively collected data on patients presenting to six spine centres included in a multicentre European database from inception to 1 November 2018. Institutional review board approval was obtained at each site for patient enrolment and data collection. Inclusion criteria were patients with degenerative or idiopathic ASD presenting with at least one criterion: coronal Cobb ≥20°; sagittal vertical axis (SVA) ≥5 cm; thoracic kyphosis (TK) ≥60° or pelvic tilt (PT) ≥25°. Exclusion criteria were: patients under the age of 18 years or any prior spinal surgery. As this was a review of their initial presentation, pain and functional scores, no minimum follow-up was incorporated.
Patients were classified according to their BMI at presentation. Baseline demographics of age, sex, associated comorbidities, employment status and smoking status were recorded. Associated comorbidities included any other medical or surgical problem and patients were grouped into either having or not having comorbidities. Employment status was defined as either unemployed or other. Unemployed included all patients who were unemployed or permanently retired due to spinal pathology. Others included students, part or full time employed and the elderly who retired for other reasons. Smoking status was defined as either current, ex-smoker (if quit over a year prior) or never smoked.
The radiological parameters of major coronal cobb, coronal balance (C7 plumb line to central sacral vertical line), SVA, global tilt, and pelvic incidence minus lumbar lordosis (PI − LL) mismatch were also documented.
The patients’ initial Numerical Rating Scale (NRS) back and leg scores, Core Outcome Measures Index (COMI) back score, SRS22 total score, Short Form 36 (SF-36) [general health, physical component score (PCS) and mental component score (MCS)] score and Oswestry Disability Index (ODI) scores (including all domains) were recorded.
Statistical analysis
The BMI is analysed as a continuous measure with the mean and standard deviation provided for patient gender, whether patients had associated comorbidities, employment status and smoking status (12). The associations between these features and BMI were statistically tested using independent t-tests. Subsequently, Pearson’s correlation coefficients were used to describe the relationships between BMI and the pain and functional scores. Then, a multivariate linear regression analysis with patients’ baseline demographics (age, gender, comorbidities, smoking status and occupation) and radiological parameters (major coronal cobb, coronal balance, SVA, global tilt, and PI − LL mismatch) entered as covariates, was performed to determine the independent associations of BMI with the pain and functional outcomes.
A P value of less than 0.05 was considered significant.
Results
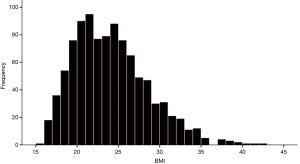
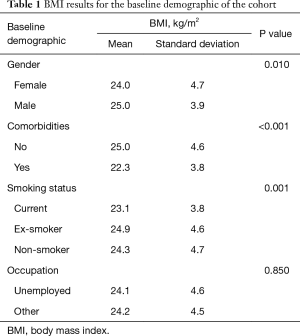
As of 1 November 2018, 2,523 adult patients were enrolled in the ESSG database. Of these 1,004 patients met our inclusion and exclusion criteria (166 male, 838 female). Figure 1 shows the BMI distribution for all patients, while Table 1 displays the BMI variance for the baseline demographics.
Full table
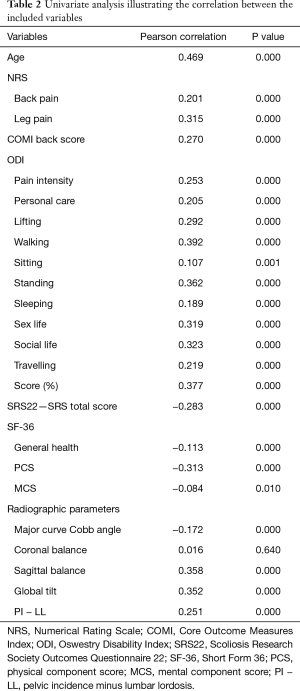
On univariate analysis (Table 2) statistically significant (P<0.05) weak to moderate correlations were identified between BMI and patient age, and all pain and functional outcomes with the exception of coronal balance (P=0.64).
Full table
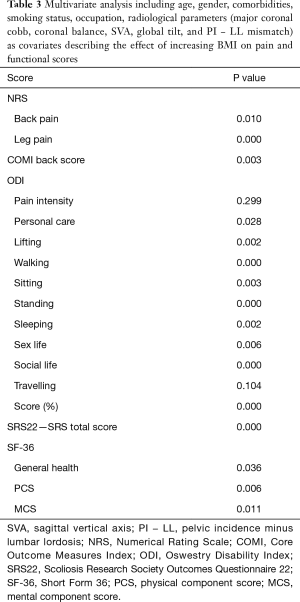
On multivariate analysis (Table 3) BMI remained significantly (P<0.05) related to all functional outcomes except ODI pain (P=0.299) and travelling (P=0.104).
Full table
Discussion
This study is, to our knowledge, the first to assess the effect of increasing BMI on the pain and function of patients presenting with ASD. This study reveals a clear correlation between increasing BMI and the patients’ pain and functional capacity, even when accounting for patient age, gender, occupational status, smoking status and the radiographic parameters known to relate to functional outcomes.
Multiple previous studies have assessed the effect of BMI on low back pain and recognised a relationship between increasing BMI and the prevalence of low back pain (13,14). However, the degree of pain and functional limitation in these patients is not known. Furthermore, in patients with ASD the degree of pain and functional limitation is known to be directly related to sagittal balance and is also likely affected by age, gender, medical comorbidities, psychosocial factors (such as smoking and occupational status) and other spinal alignment parameters (such as coronal cobb and global tilt) (3,4). Thus, to understand whether BMI has an independent effect on the pain and function of patients with ASD we performed a multivariate analysis accounting for these variables.
Our results show that increasing BMI is associated with poorer function in all ODI domains, except ODI pain and travelling. The reason why the ODI pain score failed to reach statistical significance, yet the NRS back and leg pain score did is uncertain. However, it is known that different scores may give varied results which may be the reason for this outcome. In particular, ODI pain is a composite of all pain (back and leg), in contrast to the NRS score that splits back and leg pain. The use of a combined back and leg score has been shown to have a higher correlation with health-related quality of life scores than individual scores (15). The reason why BMI is not associated with a poorer ODI travelling score is also unclear.
Our results also show that the correlation between BMI and the patients’ pain and function is statistically weak to moderate. However, it must be recognised that a high correlation is not likely because many factors influence these outcomes and therefore BMI is only likely to partially contribute. Further research into the effect of other variables is necessary to determine the specific contribution of each.
This study is limited by only assessing patient pain and function at presentation. It therefore does not assess interventional outcomes, most notably whether weight loss improves pain and function in patients with ASD. We also limited our review to patients who had never had previous spinal surgery and who were diagnosed with degenerative or idiopathic ASD. We did this to reduce confounders, but as a consequence the results cannot be extrapolated to other patient groups. Despite these limitations, this study illustrates that increasing BMI adversely affects the pain and function of patients with ASD.
Conclusions
Increasing BMI has a significant adverse effect on the pain and function of patients with ASD. Clinicians should recognise this association and treat patients accordingly.
Acknowledgments
Glynny Kieser for her editorial input. Prof Chris Frampton for his statistical input.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethical approval was obtained for the collection, analysis and publication of prospective registry data by the ESSG. Specific ethical approval was also obtained for this study from the ESSG (No. CE-GP-2019-16). Patients consent for the incorporation of their data into the registry and subsequent publication. The datasets generated and/or analysed during the current study are available in the ESSG repository. Registration: European spine study group (ESSG: BMI1).
References
- Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082-5. [Crossref] [PubMed]
- Acaroglu E, Yavuz AC, Guler UO, et al. A decision analysis to identify the ideal treatment for adult spinal deformity: is surgery better than non-surgical treatment in improving health-related quality of life and decreasing the disease burden? Eur Spine J 2016;25:2390-400. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-9. [Crossref] [PubMed]
- Boissière L, Takemoto M, Bourghli A, et al. Global tilt and lumbar lordosis index: two parameters correlating with health-related quality of life scores-but how do they truly impact disability? Spine J 2017;17:480-8. [Crossref] [PubMed]
- Lackner JM, Carosella AM. The relative influence of perceived pain control, anxiety, and functional self efficacy on spinal function among patients with chronic low back pain. Spine (Phila Pa 1976) 1999;24:2254-60; discussion 2260-1. [Crossref] [PubMed]
- Goldberg MS, Scott SC, Mayo NE. A review of the association between cigarette smoking and the development of nonspecific back pain and related outcomes. Spine (Phila Pa 1976) 2000;25:995-1014. [Crossref] [PubMed]
- Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med 2009;169:251-8. [Crossref] [PubMed]
- Lake JK, Power C, Cole TJ. Back pain and obesity in the 1958 British birth cohort. cause or effect? J Clin Epidemiol 2000;53:245-50. [Crossref] [PubMed]
- Livshits G, Popham M, Malkin I, et al. Lumbar disc degeneration and genetic factors are the main risk factors for low back pain in women: the UK Twin Spine Study. Ann Rheum Dis 2011;70:1740-5. [Crossref] [PubMed]
- Müller-Riemenschneider F, Reinhold T, Berghöfer A, et al. Health-economic burden of obesity in Europe. Eur J Epidemiol 2008;23:499-509. [Crossref] [PubMed]
- Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond) 2013;37:889-91. [Crossref] [PubMed]
- Zhang Z. Univariate description and bivariate statistical inference: the first step delving into data. Ann Transl Med 2016;4:91. [Crossref] [PubMed]
- Heuch I, Hagen K, Heuch I, et al. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine (Phila Pa 1976) 2010;35:764-8. [Crossref] [PubMed]
- Heuch I, Heuch I, Hagen K, et al. Body mass index as a risk factor for developing chronic low back pain: a follow-up in the Nord-Trøndelag Health Study. Spine (Phila Pa 1976) 2013;38:133-9. [Crossref] [PubMed]
- Cawley DT, Larrieu D, Fujishiro T, et al. NRS20: Combined Back and Leg Pain Score: A Simple and Effective Assessment of Adult Spinal Deformity. Spine (Phila Pa 1976) 2018;43:1184-92. [Crossref] [PubMed]