
Risk factors for delay in surgery for patients undergoing elective anterior cervical discectomy and fusion
Introduction
Anterior cervical discectomy and fusion (ACDF) is an established elective surgical procedure for the treatment of degenerative cervical spine disease that has demonstrated excellent long-term clinical outcomes (1-3). Outpatient care of cervical fusions is becoming increasingly popular as a number of studies have demonstrated satisfactory outcomes for appropriate candidates (4-7). Furthermore, outpatient care has demonstrated to be more cost effective for ACDF (4,7). However, the largest threat to both the cost savings and safety associated with outpatient ACDF is the risk for unplanned healthcare utilization, such as from higher rates of readmissions or surgical delay.
For numerous non-elective orthopedic surgeries, surgical delay after hospital admission is closely related to increased length of stay or increased rates of postoperative complications. Consequently, the incidence of, and risk factors for, delay of many common non-elective orthopedic procedures and the complications associated therewith have been evaluated thoroughly (8-14). However, surgical delay has not been carefully evaluated for the various elective orthopedic procedures of the spine. A recent analysis conducted by Wagner et al. [2018] examined the incidence of, and risk factors for, surgical delay in patients undergoing elective single level lumbar fusion. This study appears to be the first to examine risk factors for surgical delay in an elective procedure of the spine. To our knowledge there has not been an examination of risk factors for surgical delay in patients undergoing elective ACDF. The current study hopes to provide physicians with insight into factors that are predictive of surgical delay for patients undergoing elective ACDF. Providing additional evidence to describe risk factors for surgical delay may help reduce resource utilization associated with this event.
The object of the study was to identify risk factors for surgical delay in patients undergoing elective ACDF. Therefore, we utilized the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database to identify the incidence and risk factors of surgical delays in this setting. A secondary objective was to compare 30-day postoperative outcomes in patients with and without delays prior to surgery. Our null hypothesis was that pre-operative functional status and comorbidity burden are associated with an increase in surgical delay of ACDF.
Methods
Data source
We performed a retrospective cohort study using the ACS NSQIP® database. The ACS NSQIP is a national, multicenter database that utilizes a trained clinical reviewer at each site who collects preoperative, intraoperative, and 30-day postoperative data on randomly assigned patients. The data is periodically reviewed by the ACS to ensure validity and accuracy. The study was exempt from Institutional Review Board (IRB) approval due to the de-identified nature of the database.
Inclusion and exclusion criteria
The investigation was limited to non-emergency procedures. By excluding emergency procedures, infections, tumor cases, trauma, and revision surgeries, an elective patient population was isolated to reduce the potential for preoperative confounding variables with regard to surgical indications. Current procedural terminology (CPT) codes 22251, 22252, and 22554 were utilized to identify all patients over 18 in the NSQIP database undergoing elective anterior cervical surgery from 2006–2015. A surgical delay was defined as surgery that occurred one day or later after initial hospital admission. Patient characteristics and comorbidities were extracted from the registry to identify differences between the delayed and non-delayed groups. Patient characteristics included patient age, sex, American Society of Anesthesiology (ASA) class, body mass index (BMI), functional health (independent, partially or totally dependent), diabetes mellitus (DM), smoking status, steroid use for chronic condition, and several medical conditions, such as bleeding disorders, ascites, congestive heart failure (CHF), severe chronic obstructive pulmonary disease (COPD), and hypertension.
The NSQIP database provides 30-day post-operative outcomes for a number of complications. Complications assessed included cardiac arrest with cardiopulmonary resuscitation (CPR), myocardial infarction (MI), ventilator use >48 hours, unplanned intubation, acute renal failure (ARF), acute bleeding requiring transfusions, deep vein thrombosis (DVT)/thrombophlebitis, pulmonary embolism (PE), septic shock, sepsis, pneumonia, superficial surgical site infection (sSSI), wound disruption, deep incisional surgical site infection (dSSI), and urinary tract infection (UTI). Major complications included reintubation, ventilator use, peripheral nerve injury, ARF, sepsis and septic shock, PE, cardiac complications, cardiac arrest, pulmonary complications, deep wound infection, MI, stroke, and coma (15).
Statistical analysis
The objective of our statistical analysis was to identify patient characteristics that were associated with higher rates of surgical delay for patients undergoing ACDF surgery. In addition, an analysis was conducted to determine if surgical delay was associated with higher rates of 30-day mortality, post-operative complications, and length of stay. Chi-square tests were used for categorical variables and independent student t-tests for continuous variables. Multivariate logistic regression was then used to analyze associations between preoperative variables and postoperative complications that were found to be statistically significant based on univariate analysis. Calculated associations were reported as multivariate odds ratios with 95% confidence intervals, with a P<0.05 indicating significance. Statistical analysis was completed utilizing IBM SPSS® software.
Source of funding
There was no external source of funding.
Results
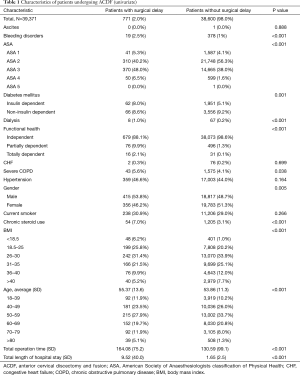
We identified 39,371 patients undergoing ACDF between 2006 and 2015. The rate of surgical delay was 2.0%, for a total of 771 patients experiencing a delay between the time of admission and surgery. Mean age was similar between the non-delayed and delayed cohort (53.86 compared to 55.37; P<0.001). Patients in the delayed group generally suffered from a higher comorbidity burden compared to patients in the non-delayed group. For instance, patients with an elevated ASA classification were more likely to experience a delay (P<0.001). Similarly, patients who were partially dependent or totally dependent on a caretaker for activities of daily living were more likely to experience a delay in surgery (P<0.001). Average operating time was 33.5 minutes longer for the delayed group compared to the non-delayed group (164.08 minutes compared to 130.59 minutes; P<0.001). The delayed cohort experienced a five-fold increase in total length of stay compared to the non-delayed cohort (9.52 days compared to 1.65 days; P<0.001).
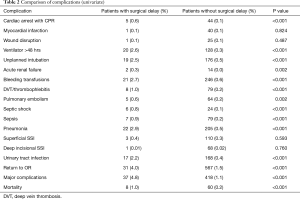
Based on univariate analysis, the following comorbidities were found to be associated with surgical delay: bleeding disorders, ASA classification, DM, dialysis use, functional health status, severe COPD, gender, chronic steroid use, BMI, and age (Table 1). Patients experiencing delay of surgery had higher rates of postoperative surgical and medical complications. The delayed group experienced higher rates of cardiac arrest with CPR, ventilator use >48 hours, unplanned intubation, ARF, acute bleeding requiring transfusions, DVT/thrombophlebitis, PE, septic shock, sepsis, pneumonia, UTI, return to OR, and overall major complications (Table 2). The mortality rate was five time higher for the delayed group compared to the non-delay group (1.0% compared to 0.2%; P<0.001).
Full table
Full table
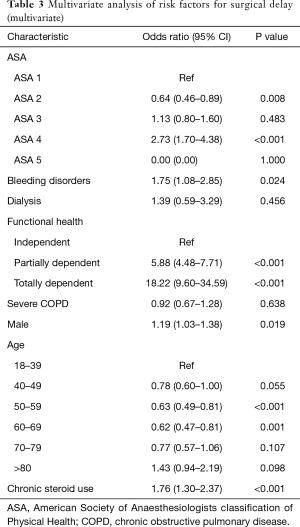
Multivariate analysis identified ASA class 4 (OR 2.73; 95% CI: 1.70–4.38; P<0.001), dependent functional status (OR 5.88; 95% CI: 4.48–7.71; P<0.001), totally dependent functional status (OR 18.22; 95% CI: 9.60–34.59; P<0.001), bleeding disorders (OR 1.75; 95% CI: 1.08–2.85; P=0.024), male sex (OR 1.19; 95% CI: 1.03–1.38; P=0.019), and chronic steroid use (OR 1.76; 95% CI: 1.30–2.37; P<0.001) as independent predictors of delayed surgery after hospital admission (Table 3).
Full table
Discussion
This study identifies risk factors that increase the likelihood of surgical delay for patients undergoing elective ACDF. Furthermore, we found through univariate analysis that surgical delay was associated with worse surgical outcomes, higher mortality rates, and an increased length of stay. These general findings support those previously determined in knee and hip arthroplasty literature (8-11,13,14). In addition, the results are in alignment with Wagner et al.’s findings, which found that patients undergoing elective single-level lumbar fusion who experienced a surgical delay were more likely to have worse postoperative outcomes, higher mortality rates, and incur greater hospital costs. The study performed by Wagner et al. serves as the best study for comparison, as their analysis was selected for elective cases on a specific surgical procedure of the spine that is also commonly performed. Furthermore, mean patient age was similar for the study conducted by Wagner et al. (59.3 years) compared to the current study (53.9 years), whereas the average age for patients undergoing total joint arthroplasty is over sixty-five (16,17).
The incidence of surgical delay in our study was 2.0%, which is consistent with the incidence reported by Phruetthiphat et al. for total hip arthroplasty (2.3%) and total knee arthroplasty (0.9%) (9,10). Wagner et al. reported a higher incidence rate of 5.5% (18), however, the percentage of patients with an ASA classification greater than two was noticeably higher in their cohort compared to ours. In our cohort, 39.8% of patients were ASA >2, whereas 47.2% of the patients in Wagner et al.’s study had an ASA class >2. A higher ASA classification has previously been found to be an independent risk factor for surgical delay (9,10,19). Therefore, this latter difference may partially explain the higher incidence rate of surgical delays in Wagner et al.’s analysis.
We were able to identify ASA class 4, male sex, and chronic steroid use as independent predictors of delayed surgery after hospital admission for ACDF. In a study of patients undergoing elective single-level lumbar fusion, Wagner et al. also identified male sex, ASA class 4, and steroid use as risk factors of surgical delay, but neither functional status nor bleeding disorders were included. We, however, found functional status and bleeding disorders as additional independent risk factors for delay. These latter two risk factors have also been identified as independent predictors for delay in patients undergoing elective knee arthroplasty and primary total hip arthroplasty (9,10).
In our study, surgical delay was associated with increased post-operative morbidity and mortality. This finding is in agreement with existing studies (9,10,13,14,18,20). Patients in the delayed group experienced higher rates of UTI, pneumonia, sepsis, septic shock, PE, DVT, bleeding transfusions, ARF, unplanned intubation, ventilator use >48 hours, cardiac arrest with CPR, and return to OR. There was a five-fold increase in mortality rate (1.0% compared to 0.2% in non-delayed; P<0.001) in patients who experienced a surgical delay in our study. Similarly, numerous studies have linked surgical delay to increased post-operative mortality in patients undergoing various orthopedic procedures (9,13,14,21,22). However, it is important to consider that an increase in post-operative morbidity and mortality in the delayed group was likely due to the patient’s health status and is only weakly associated with surgical delay as an event.
Length of hospital stay was significantly longer for the delayed group compared to the non-delayed group. The delayed cohort in the current study experienced a five-fold increase in total length of stay compared to the non-delayed cohort (9.52 days compared to 1.65 days; P<0.001).The difference in length of stay between the two cohorts is comparable to the difference reported by Wagner et al., who noted a three-fold increase in total length of stay for patients with a surgical delay (11.4 days compared to 3.7 days; P<0.001) (18). In our study, the higher rate of post-operative complications in the delay group was a likely contributor to this noticeable difference in length of stay. Consequently, in an increasingly cost-conscience healthcare landscape, surgeons should improve efforts to identify patients who are at risk of delay, as prolonged length of stay is correlated with higher resource utilization (22,23).
In addition to the retrospective nature of this analysis, there are a number of limitations to the conclusions provided that must be taken into consideration. First, while we identified risk factors for surgical delay, the precise reasons for delay were not consistently available within the data set. It is possible that the delay was initiated by the surgical team to optimize the patient prior to surgery. However, an explanation for such delays is not provided in the data set. Second, the database does not distinguish between complications occurring between admission and surgery, and complications occurring after surgery. Third, any patient who was delayed but not subsequently admitted to the hospital and sent home was not included in the study. Our study only included those who were admitted and received surgery in the same admittance period. Fourth, NSQIP postoperative information is limited to 30-days and therefore does not capture important health events that may have occurred at a later date, radiographic data, or patient reported outcomes measures. However, these limitations are accepted in exchange for the robust sample size available through the NSQIP and the novelty of this study. Furthermore, the NSQIP is a highly reputable database that reports patient characteristics and clinical factors that we believe provide an accurate evaluation of surgical delay in the setting of elective ACDF. Despite our attempt to control for baseline comorbidities, these were limited to those listed on NSQIP. It also avoids specific variabilities within these comorbidities. For example, it fails to distinguish severity, such as a patient with congestive heart failure and an ejection fraction greater or less than 35%.
Our study hopes to provide physicians with insight into factors that are predictive of surgical delay for patients undergoing elective ACDF. Unlike non-elective orthopedic operations, an elective operation provides time for the healthcare team (surgeon, anesthesiologist, nursing, and operating room staff) to perform the necessary clinical and laboratory workup prior to surgery, thereby optimizing the evaluation of medical co-morbidities. Physicians that are able to identify patients at high risk of experiencing surgical delay can more accurately counsel them regarding risks and perhaps recommend other less invasive alternatives, if warranted. Additionally, this may improve the overall efficiency of resource utilization. We would encourage care and outcomes assessment programs to stratify co-morbidities even further to allow physicians to improve optimization strategies to a greater degree. One consideration would be to improve classification of, or to stratify co-morbidities, to more accurately predict risk factors. For example, stratifying ejection fractions for CHF (i.e., less than 25%, 25–50%, 50–75%) (24,25), or HbA1c for DM (i.e., <6%, 6–8%, >8%, etc.) (26-28) would be a useful modification to the current NSQIP database and help to guide pre-operative medical surveillance and optimization.
Conclusions
Using a national multicenter database and a population of 39,371 patients, our study successfully identified a number of risk factors associated with surgical delay in ACDF. Impaired functional status, ASA class 4, bleeding disorders, male sex, and chronic steroid use were identified as independent predictors of delayed surgery after hospital admission. These results help physicians identify controllable risk factors that can be corrected before performing ACDF, thereby potentially reducing the risk of delay. Improved stratification of medical comorbidities could improve this optimization strategy even further.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Mayo BC, Massel DH, Bohl DD, et al. Anterior Cervical Discectomy and Fusion: The Surgical Learning Curve. Spine 2016;41:1580-5. [Crossref] [PubMed]
- Carreon LY, Anderson PA, Traynelis VC, et al. Cost-Effectiveness of Single-Level Anterior Cervical Discectomy and Fusion Five Years After Surgery. Spine 2013;38:471-5. [Crossref] [PubMed]
- Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine 2007;32:2310-7. [Crossref] [PubMed]
- Wohns R. Safety and cost-effectiveness of outpatient cervical disc arthroplasty. Surg Neurol Int 2010;1:77. [Crossref] [PubMed]
- Adamson T, Godil SS, Mehrlich M, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. J Neurosurg Spine 2016;24:878-84. [Crossref] [PubMed]
- McGirt MJ, Godil SS, Asher AL, et al. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus 2015;39:E9. [Crossref] [PubMed]
- McClelland S, Passias PG, Errico TJ, et al. Outpatient Anterior Cervical Discectomy and Fusion: An Analysis of Readmissions from the New Jersey State Ambulatory Services Database. Int J Spine Surg 2017;11:3. [Crossref] [PubMed]
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop 2008;79:168-73. [Crossref] [PubMed]
- Phruetthiphat OA, Gao Y, Vasta S, et al. Preoperative Risk Factors for, and Incidence of Delayed Surgery in Elective Primary Total Knee Arthroplasty After Hospital Admission: The ACS-NSQIP. J Arthroplasty 2016;31:1413-6. [Crossref] [PubMed]
- Phruetthiphat OA, Gao Y, Anthony CA, et al. Incidence of and Preoperative Risk Factors for Surgical Delay in Primary Total Hip Arthroplasty: Analysis From the American College of Surgeons National Surgical Quality Improvement Program. J Arthroplasty 2016;31:2432-6. [Crossref] [PubMed]
- Pape HC. Effects of changing strategies of fracture fixation on immunologic changes and systemic complications after multiple trauma: Damage control orthopedic surgery. J Orthop Res 2008;26:1478-84. [Crossref] [PubMed]
- Charlson M, Wells MT, Ullman R, et al. The Charlson comorbidity index can be used prospectively to identify patients who will incur high future costs. PLoS One 2014;9:e112479. [Crossref] [PubMed]
- Menendez ME, Ring D. Does the timing of surgery for proximal humeral fracture affect inpatient outcomes? J Shoulder Elbow Surg 2014;23:1257-62. [Crossref] [PubMed]
- Cantu RV, Graves SC, Spratt KF. In-hospital mortality from femoral shaft fracture depends on the initial delay to fracture fixation and Injury Severity Score: A retrospective cohort study from the NTDB 2002-2006. J Trauma Acute Care Surg 2014;76:1433-40. [Crossref] [PubMed]
- Chung AS, Campbell D, Waldrop R, et al. Metabolic Syndrome and 30-Day Outcomes in Elective Lumbar Spinal Fusion. Spine 2018;43:661-6. [Crossref] [PubMed]
- Crowninshield RD, Rosenberg AG, Sporer SM. Changing Demographics of Patients with Total Joint Replacement. Clin Orthop Relat Res 2006.266-72. [Crossref] [PubMed]
- Ravi B, Croxford R, Reichmann WM, et al. The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. Best Pract Res Clin Rheumatol 2012;26:637-47. [Crossref] [PubMed]
- Wagner SC, Butler JS, Kaye ID, et al. Risk Factors for and Complications After Surgical Delay in Elective Single-Level Lumbar Fusion. Spine (Phila Pa 1976) 2018;43:228-33. [Crossref]
- Ricci WM, Brandt A, McAndrew C, et al. Factors Affecting Delay to Surgery and Length of Stay for Patients With Hip Fracture. J Orthop Trauma 2015;29:e109-14. [Crossref] [PubMed]
- Weller I, Wai EK, Jaglal S, et al. The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br 2005;87:361-6. [Crossref] [PubMed]
- Vidán MT, Sánchez E, Gracia Y, et al. Causes and Effects of Surgical Delay in Patients With Hip Fracture: A Cohort Study. Ann Int Med 2011;155:226. [Crossref] [PubMed]
- O’Leary DP, Beecher S, McLaughlin R. Emergency surgery pre-operative delays - Realities and economic impacts. Int J Surg 2014;12:1333-6. [Crossref] [PubMed]
- Taheri PA, Butz DA, Greenfield LJ. Length of Stay Has Minimal Impact on the Cost of Hospital Admission. J Am Coll Surg 2000;191:123-30. [Crossref] [PubMed]
- Healy KO, Waksmonski CA, Altman RK, et al. Perioperative Outcome and Long-Term Mortality for Heart Failure Patients Undergoing Intermediate- and High-Risk Noncardiac Surgery: Impact of Left Ventricular Ejection Fraction. Congest Heart Fail 2010;16:45-9. [Crossref] [PubMed]
- Chassot PG, Delabays A, Spahn DR. Preoperative evaluation of patients with, or at risk of, coronary artery disease undergoing non-cardiac surgery. Br J Anaesth 2002;89:747-59. [Crossref] [PubMed]
- Liu J, Ludwig T, Ebraheim NA. Effect of the Blood HbA1c Level on Surgical Treatment Outcomes of Diabetics with Ankle Fractures: HbA1c and Diabetic Ankle Fractures. Orthop Surg 2013;5:203-8. [Crossref] [PubMed]
- Lamloum SM, Mobasher LA, Karar AH, et al. Relationship between Postoperative Infectious Complications and Glycemic Control for Diabetic Patients in an Orthopedic Hospital in Kuwait. Med Princ Pract 2009;18:447-52. [Crossref] [PubMed]
- Stryker LS, Abdel MP, Morrey ME, et al. Elevated Postoperative Blood Glucose and Preoperative Hemoglobin A1C Are Associated with Increased Wound Complications Following Total Joint Arthroplasty. J Bone Joint Surg Am 2013;95:808-14. [Crossref] [PubMed]


