
The prevalence of complications associated with lumbar and thoracic spinal deformity surgery in the elderly population: a meta-analysis
Introduction
The global prevalence of adult scoliosis ranges from 1% to 32% (1-3); however, the prevalence of spinal deformities increases with age (3,4) to an estimated 30% to 68% in the elderly population (5-7). Due to the prevalence and potential morbidity associated with an extensive surgical procedure, treatment of adult spinal deformities typically begins with a non-surgical approach (3,8). Non-surgical treatments include modification of physical activity, physical therapy, bracing, pain medication, anti-inflammatory medication, electrothermal therapy, and cortisone injections (9,10). Nevertheless, these treatments often fail to provide long-term, sustainable relief (9). For patients whose spinal deformity symptoms persist or worsen despite initial treatment, surgery may be a valid treatment option (3). Surgical treatment of spinal deformities is controversial for elderly patients due to the increased prevalence of surgical and medical complications in this population (7,11,12). Spinal surgery, even in younger patients with fewer co-morbidities, carries inherent risk due to the length of the procedure, potential for significant blood loss, extended hospitalization, and the possible need for reoperation. Furthermore, the poorer bone quality among elderly patients increases the risk for vertebral fractures and disease progression following surgery (10).
While elderly patients may experience a higher prevalence of complications due to their decreased physiological reserve (13), they may also stand to benefit more from surgery compared to their younger counterparts (3). Per the available literature, the overall prevalence of complications associated with spinal deformity surgery in the elderly population ranges widely, from 37% to 71% (7). While systematic reviews on this subject are available (10), no meta-analyses have been previously published on the topic.
The objective of this study was to perform a meta-analysis pooling the available data on the prevalence of complications associated with lumbar and thoracic spinal deformity surgery in patients 65 years old and older, thereby increasing the power of currently available prevalence estimates. With this information, physicians may be better able to counsel their elderly patients when considering surgery for treatment of spinal deformities.
Methods
Comprehensive search
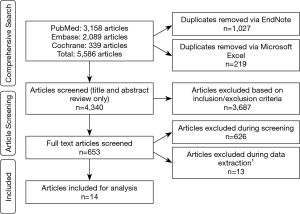
To identify relevant articles for inclusion in this meta-analysis, a comprehensive search was conducted using PubMed, Embase, and Cochrane databases, and included articles from the inception of each database through 01/21/2018. The structure of the search was based on four categories: population, indication for surgery, intervention, and reported results (Supplementary file). Search results from each database were imported to EndNote X7, which was then used to identify and remove any duplicate articles; a final listing was exported to Microsoft Excel. Additional duplicates were identified and removed manually in Excel.
Study selection
Study selection was determined based on pre-defined inclusion and exclusion criteria for study design, population, intervention, and outcomes (Table S1). For study design, randomized clinical trials, observational studies (retrospective and prospective), and case series that reported the prevalence of complications for spinal deformity surgery in the elderly population were included. Case reports, conference abstracts, articles using registry data, and articles reporting data for fewer than 5 patients were excluded. Note that registry data was excluded in order to avoid double-counting patients in the meta-analysis.

Full table
Studies describing patients ≥65 years old undergoing surgery for diagnosed thoracic and/or lumbar spinal deformity (scoliosis, kyphosis, kyphoscoliosis, spondylitis and Scheuermann’s disease) were included. Deformities related to sagittal imbalance, osteoporosis, and Parkinson’s disease were included only when the etiology of the spinal deformity met the previously stated requirements. Studies with data for patients undergoing spinal deformity surgery related to trauma, infection (ex: tuberculosis), spondylolisthesis, Kummell disease, spondyloarthropathy, Ankylosing spondylitis, spondylarthritis, tumors, metastatic lesions, and abscesses were excluded. Studies involving patients with cervical and/or sacral spinal deformity were also excluded, unless results were reported separately for thoracic and/or lumbar intervention only. Rationale for exclusions is listed in Table S1.
In terms of intervention, studies with data for spinal deformity surgery (including, but not limited to kypho- or vertebroplasty, decompression, coronal/sagittal or spinopelvic alignment, as well as wedge, pedicle subtraction, Ponte, Smith-Peterson, or spinal column osteotomies) involving 5 or more levels of the spine, including open, minimally-invasive, or hybrid approaches, and including both initial and repeat/revision procedures were included. Studies with data for procedures involving fewer than 5 levels of the spine, and/or procedures limited to discectomy, laminectomy, laminoplasty, total disc replacement, or percutaneous vertebroplasty, were excluded.
Studies must also have reported measurable prevalence of complications for spinal deformity surgery including, but not limited to, death, postoperative hemorrhage, blood loss, readmissions, reoperations, infection, pneumonia, embolism, stroke, thrombosis, pseudarthrosis, radiculopathy, neurological deficits, myocardial infarction, cardiovascular events, cerebrovascular events, and hardware failure.
Non-English articles were also excluded. Articles that included both eligible and ineligible patients were included only if sufficient patient-specific data were provided to extract the data for eligible patients.
Six investigators (C Smith, QA Vo, D Joshi, L Araujo-Lama, Z Ou, J Doucette, S Lim) reviewed the potential articles to determine eligibility for inclusion in this meta-analysis, with two investigators independently reviewing each article to ensure a consensus. Level 1 selection was based upon title and abstract review only. Studies that passed Level 1 selection were then reviewed at Level 2, which included a full text review. The reason for exclusion of any of the articles during Level 2 review was documented. Any disagreements were resolved through group discussion, or brought to three expert investigators (RA Mekary, H Zaidi and LS Aglio) when consensus could not be reached.
Data extraction
Seven investigators (C Smith, QA Vo, D Joshi, L Araujo-Lama, J Doucette, S Lim) extracted data for articles that met study selection criteria. Two investigators extracted the data independently for each article to ensure consistency and accuracy. Any disagreements were resolved through group discussion, or brought to clinicians (H Zaidi, and LS Aglio) for resolution when a consensus could not be reached.
The following study characteristics, when available, were extracted: publication year, journal impact factor, country, single or multiple centers, total number of patients, and number of patients to be included for meta-analysis specifically. For patient characteristics, age, body mass index (BMI), gender, spinal deformity type(s) and location(s), as well as comorbidities were extracted. Surgical approach, number of levels of the spine involved, surgery setting, and duration of follow-up were extracted for intervention characteristics. The following outcomes, when available, were extracted: mean, standard deviation, and number of patients experiencing blood loss; number of patients with events and the total number of patients for death, readmission, prolonged hospitalization, postoperative hemorrhage, hardware failure, reoperation, infection, pneumonia, cardiovascular event, myocardial infarction, deep vein thrombosis, pulmonary embolism, pseudarthrosis, neurological deficit, cerebrovascular event, stroke, radiculopathy, and/or any other reported complication types.
Quality score was derived for each article using the Newcastle-Ottawa Scale for non-randomized studies (14). For case control studies, the quality score was based on case definition, representativeness of the cases, selection and definition of controls, comparability of cases and controls on the basis of the design or analysis, ascertainment of exposure, and non-response rate. For cohort studies, the quality was calculated based on representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at the start of the study, comparability of cohorts based on the design or analysis, assessment of outcome, sufficient duration of follow-up, and the adequacy of follow-up of cohorts. Regarding case series, the Newcastle-Ottawa Scale was modified to reflect the non-comparative nature of the studies and the quality score was derived based on the clarity of the study objective(s)/question(s), protocol definition, explicit inclusion/exclusion criteria, specified time interval for patient recruitment, consecutive patient enrollment, clinically relevant outcomes, prospective outcome data collection, and follow-up rate.
Data analysis
Comprehensive Meta-Analysis Version 3 (copyright 1998–2017, Biostat, Inc., USA) was utilized for statistical analysis. Results for the selected articles were combined statistically. Pooled estimates for each complication type were calculated using the random effects model, which accounted for both within-study and between-study variances. The DerSimonian and Laird approach (15) was used to estimate variance between studies. Forest plots were generated to report the estimates for the individual studies as well as the pooled studies, with associated confidence intervals included.
To assess heterogeneity among the studies, the Cochran Q statistic was calculated for the chi-square test for heterogeneity, with a P value of <0.10 indicating significant heterogeneity. In addition, the I-squared statistic was calculated to reflect the percentage of variation due to between-study heterogeneity rather than chance alone. An I-squared value <40%, 40–75%, and >75% was considered indicative of low, moderate, or high heterogeneity, respectively. To further explore heterogeneity, sensitivity analyses were performed by excluding studies in which the number of spine levels involved was not explicitly stated, and including only those that confirmed 5 or more levels. Meta-regression was also performed to determine if the study quality score, gender, or mean age were potential sources of heterogeneity across studies. Country of origin could not be included in the heterogeneity analysis because the majority of studies were from the United States, and the remainder were from various other countries.
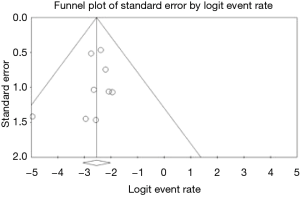
The investigators attempted to minimize bias through systematic adherence to a pre-defined protocol for the study search, selection, data extraction, and analysis. Potential publication bias was identified using a funnel plot for visual determination of asymmetry, as well as Begg’s and Egger’s test for statistical significance (16,17).
Results
The comprehensive search returned a total of 5,586 articles, of which 1,246 were duplicates and subsequently removed. Level 1 screening of the title and abstract resulted in exclusion of 3,689 articles based on the pre-defined inclusion/exclusion criteria. Level 2 screening of the full article text was performed for the remaining 653 articles and 626 were excluded. The primary reasons for exclusion during Level 2 screening were patient ages <65 (n=342), indications for surgery involving deformities that did not meet eligibility criteria (n=13), and surgeries encompassing fewer than 5 levels of the spine (n=47), with all of these lacking an appropriate sub-group to parse out eligible patients. Further reasons for exclusion were studies that contained only registry data (n=177) or in which complications were not reported (n=11).
A total of 27 articles were identified for data extraction, but upon further review and based on the pre-defined eligibility criteria, 10 articles were subsequently excluded, with reasons listed in Figure 1. In addition, 3 out of the 4 articles written by the same lead author in 2017–2018 were also excluded during the data extraction process; only the article with the highest number of eligible patients was selected for inclusion to prevent double-counting patient data (18-20). In total, 14 articles were included in the final analysis ( Figure 1) (21-34).
The 14 articles selected for meta-analysis consisted of retrospective (n=7) and prospective (n=5) case series, retrospective cohort (n=1), or case-control (n=1) studies. One of the articles (21) reported results separately for early versus late ambulation after surgery, allowing for these data to be treated as two separate studies for data analysis without double-counting patients. Quality scores across these articles ranged from 6 to 8. Across studies reporting patient age, the mean age of patients ranged from 68.6 to 76.6 years. Patient populations were predominately female, with a range of 11.1% to 60.0% male. Types of spinal deformities included scoliosis, kyphosis, proximal and distal junctional kyphosis, and adjacent level disease. Surgical approaches varied across studies and included both minimally-invasive and traditional procedures. For articles that reported the number of levels of the spine involved in surgery, the mean ranged from 5.9 to 11.4 ( Table 1).
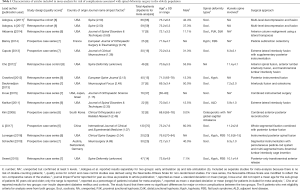
Full table
There were 14 complication types reported, with at least 2 studies for each complication: reoperation (prevalence 19%; 95% CI, 9–36%; 5 studies; 107 patients; I2=56.6%; P-heterogeneity =0.06), hardware failure (11%; 95% CI, 5–25%; 4 studies; 52 patients; I2=0%; P-heterogeneity =0.52), infection (7%; 95% CI, 4–12%; 9 studies; 262 patients; I2=0%; P-heterogeneity =0.86), pseudarthrosis (6%; 95% CI, 3–12%; 6 studies; 149 patients; I2=0%; P-heterogeneity =0.76), radiculopathy (6%; 95% CI, 1–33%; 4 studies; 116 patients; I2=69.3%; P-heterogeneity =0.02), cardiovascular event (5%; 95% CI, 1–32%; 4 studies; 121 patients; I2=73.5%; P-heterogeneity =0.01), neurological deficit (5%; 95% CI, 2–15%; 7 studies; 248 patients; I2=62.7%; P-heterogeneity =0.01), deep vein thrombosis (3%; 95% CI, 1–7%; 5 studies; 230 patients; I2=0%; P-heterogeneity =0.53), pulmonary embolism (3%; 95% CI, 1–7%; 4 studies; 210 patients; I2= 0%; P-heterogeneity =0.44); pneumonia (3%; 95% CI, 1–11%; 4 studies; 210 patients; I2= 40.7%; P-heterogeneity =0.17), cerebrovascular or stroke event (2%; 95% CI, 0–9%; 2 studies; 85 patients; I2= 0%; P-heterogeneity =0.65), death (2%; 95% CI, 1–9%; 4 studies; 113 patients; I2=0%; P-heterogeneity =0.76), myocardial infarction (2%; 95% CI, 1–6%; 4 studies; 210 patients; I2=0%; P-heterogeneity =0.64) and postoperative hemorrhage (1%; 95% CI, 0–10%; 2 studies; 85 patients; I2=0%; P-heterogeneity =0.45).
Of the 14 primary analyses of complication type, 12 demonstrated that the true prevalence was different from zero with 95% confidence: cardiovascular event, death, deep vein thrombosis, hardware failure, infection, myocardial infarction, neurological deficit, pneumonia, pseudarthrosis, pulmonary embolism, radiculopathy, and reoperation. Conversely, the true prevalence of two complication types (cerebrovascular event or stroke and postoperative hemorrhage) could have been zero, with 95% confidence.
Heterogeneity was low for the majority of the complication types, but moderate to significant for cardiovascular event, neurological deficit, radiculopathy, and reoperation (Table 2). Sensitivity analyses including studies that confirmed involvement of 5 or more levels of the spine, in addition to meta-regression on study quality, mean age, and percent male are shown in Table 2. Aside from death, for which the true prevalence could have been zero, with 95% confidence (prevalence =2%, 95% CI: 0–10%), there were no other major changes in the complication rates upon restriction to only those studies that confirmed inclusion of 5 or more spine levels. For meta-regression, the only significant result was study quality for radiculopathy, which showed a prevalence increase of 3.12 for every 1 unit increase in study quality score (P <0.01).

Full table
Due to the limited number of articles for each complication type, publication bias could only be assessed for infection ( Figure 2) . The symmetry of the funnel plot suggested a lack of publication bias and was confirmed by the Begg test Kendall’s tau (2-tailed, without continuity correction, P value =0.83) and Egger test (2-tailed, P value =0.45). In addition, the high fail-safe N of 181 indicated there would be 181 null studies needed to drive the results towards the null.
Discussion
The present study identified a total of 14 complication types in the elderly following spinal surgery, with 12 of these occurring at a rate greater than zero. Of these, the most common complications included reoperation, hardware failure and infection. When limiting analysis to patients undergoing surgery involving at least 5 levels of the spine, the prevalence for 6 of the complication types remained similar with reoperation, hardware failure, and neurological deficit being the most common. These results were consistent with our hypothesis that there would be a high prevalence for complications among the elderly population undergoing thoracic and/or lumbar spinal deformity surgery.
While no prior meta-analyses have been conducted on this topic, a number of retrospective series have assessed the types and rates of complications in elderly patients undergoing spinal deformity surgery. The overall rates of any complication following spinal surgery in this group have ranged from 37% to 71% (3,35,36). This wide range is, in part, due to variability among studies in terms of patient co-morbidities, pre-operative functional status, and the details of the surgical procedure being performed, such as the number of levels fused (3,35,36). While we were unable to report the overall prevalence of any complication in our pooled analysis due to the risk of double-counting patients, we were able to determine the prevalence of a total of 14 individual complications. The results of our meta-analysis suggest that the most common complications, all with a prevalence greater than zero, include reoperation, hardware failure, and infection, occurring at prevalence of 19%, 11%, and 7%, respectively.
Reoperation prevalence after spinal deformity surgery in the general population is consistently reported as over 20% (37-39), which is consistent with the rate of 19% found in this study’s pooled analysis on elderly patients. The studies by Caputo et al. (24) and Scheufler et al. (33) reported the lowest rates of reoperation at 6% and 8%, respectively. Caputo et al. used a minimally invasive lateral technique for deformity correction that has been implicated to have fewer complications than the more traditional anterior/posterior or posterior-only approaches (29). Similarly, Scheufler et al. utilized a less invasive, image-guided technique in all of their patients (33). The application of these minimally invasive techniques could, at least in part, explain why the reoperation rates in these studies were notably lower than previously reported in the literature and among the other studies in our analysis. Moreover, Inoue et al. specifically focused on spinal fusion surgeries that included the sacrum, a known prevalence factor for unexpected second operations, possibly explaining this group’s higher reoperation rate of 38% (28). Thus, while the results of our analysis demonstrate that there was a non-negligible prevalence of reoperation for elderly patients undergoing spinal deformity surgery, the variability in rates across studies suggests additional factors, such as surgical technique and extent, should be considered when deciding whether surgery was the optimal choice for such patients.
The complication rate secondary to hardware failure ranged from 3% to 22% (27,31,35,37). Notably, the study with the highest complication rate of 22%, by Akbarnia et al., involved the use of a novel lateral surgical technique instead of the more traditional posterior-based approach. The novelty of this procedure may have contributed to the higher rates of hardware failure observed in this study (27,31,35,37). Interestingly, the study reporting the lowest rate of hardware failure in elderly patients was still higher than that found in the non-elderly patients in the same study at 6.7% vs. 4%, respectively (31). One possible explanation for this may be related to the higher rate of osteoporosis in the elderly. Studies have shown that low bone quality may lead to screw loosening and delayed bone fusion, resulting in hardware failure and impacting the success of surgical correction in osteoporotic patients (40,41). Overall, the results of this study suggested a significant prevalence of hardware failure in elderly patients undergoing spinal surgery. The risk for hardware failure may, in part, depend on surgical technique and potentially be increased in elderly patients due to their higher rates of co-morbid bone diseases (42).
The included studies demonstrated that the elderly were at both a higher prevalence of developing post-operative infection, as well as for subsequent sequelae from infection. Prevalence of infection ranged from 0% to 13% across the included studies in our meta-analysis (26-28,31,32,34,36,37). Two studies included patients less than 65 years of age with all post-operative infections occurring in the elderly subset of patients (31,34). While these studies were not intended to be matched cohort studies, the data suggested an increased vulnerability to infections in the elderly population; this observation may be explained by the decline in immune function known to occur with aging (43). With respect to studies that reported low or equal rates of infections regardless of age, consequences of infection were higher in the elderly population. For example, age greater than 65 and the presence of infection increased the prevalence of delirium by almost nine-fold (44).
Per the present analysis, complication rates for cerebrovascular events, post-operative hemorrhage, and stroke were non-significant in the elderly population based on two studies that provided data on these outcomes (31,36). One of the studies specifically excluded patients with any cardiovascular co-morbidity (36), a known prevalence factor for cerebrovascular event and stroke (45), and thus is a possible explanation for their reported lower rates of this complication. The other study included only 15 patients (31), thus potentially being underpowered to detect a significant prevalence. Further studies including a greater number and wider range of patients are needed to better understand the prevalence of cerebrovascular events and stroke in this population following spinal surgery.
Examination of individual studies revealed additional factors that affected complication rates in the elderly following spinal deformity surgery. Adogwa et al. highlighted how the post-operative period influenced outcomes by demonstrating that elderly patients who were walking within 24 hours of surgery had a significantly lower rate of complications, as well as reduced hospital stay and improved functional status (21). Furthermore, they showed that early ambulation led to a lower prevalence of myocardial infarction, deep vein thrombosis, neurological deficits, pneumonia, and pulmonary embolism (21).
The studies included in this meta-analysis reported conflicting results with respect to the correlation between comorbidities and spinal surgery complications. For example, in one study, no difference in complication rates following spinal surgery in matched controls with and without diabetes mellitus was reported (30); in contrast, hypertension was found to be predictive of a major complication in another study (40). Interestingly, others reported no association between the presence of a comorbidity and complication rates (41). Due to the inconsistently reported data in our included studies, sub-group analyses based on comorbidities could not be performed. To better understand the influence of these co-morbidities, future studies should aim to stratify patients by status of other common serious illnesses.
The data from this study indicated there was a non-negligible prevalence of complications following spinal deformity surgery in the elderly population, yet there existed a wide variability in the incidence of complications. Therefore, clinicians should carefully weigh the risks and benefits when deciding upon a treatment recommendation and give due consideration to individual patient characteristics, such as co-morbidities and pre-operative functional status, as well as the type and extent of surgery. Moreover, it is important to remember that even when prevalence for particular complications appeared to be low, or no different than the prevalence in younger patients, the elderly were more likely to experience longer recovery times, further complications, and functional decline secondary to a complication (46). Given these considerations and new evidence showing that spinopelvic parameters need to be tailored for age groups, with less stringent criteria in elderly patients, current literature suggests a “less is more” approach for spinal deformity surgery in the elderly population (47). Specifically, smaller surgeries with less correction of spinopelvic parameters appear to be the most beneficial for the elderly population.
The results of this study should be considered in the context of its limitations. There was heterogeneity among studies in terms of surgical technique (minimally invasive vs. traditional open; lateral vs. posterior-only vs. anterior/posterior approach), as well as indications for and extent of surgery. Due to the small number of patients in each category, sub-group analysis based on technique alone could not be performed. While the included patients did present with different indications for surgery, the investigators attempted to limit heterogeneity by narrowing the inclusion criteria to a specific set of spinal deformities and excluding those undergoing spinal deformity surgery for a variety of other causes. Finally, to address the extent of surgery, the investigators performed sub-group analyses to identify differences in results between studies that confirmed 5 or more levels of spine involvement versus those that did not specify. Patient comorbidities may play a role in operative outcomes and therefore the investigators attempted to extract data on these from each study. However, sub-group analyses could not be performed given that these data were reported inconsistently across studies. For example, some studies included information on all patients in their study, while only a subset met eligibility criteria. Moreover, a number of studies did not report data on co-morbidities at all.
Despite the limitations, this meta-analysis had several strengths. Meta-analyses of the complication rates in elderly patients undergoing lumbar or thoracic spinal fusion surgery have not previously been published. Moreover, the investigators were able to quantitatively analyze complications across 14 different categories and perform sub-group analyses based on several factors. Furthermore, sources of bias were assessed via meta-regression. The results of this meta-analysis offer evidence that elderly patients face a more than minimal risk of several complications following spinal deformity surgery and provide rationale for clinicians to carefully consider the risk-benefit ratio before offering surgical intervention to this group of patients.
Conclusions
In elderly patients undergoing thoracic or lumbar spinal deformity surgery, the most commonly reported complications included reoperation, hardware failure, and infection. Future studies should investigate individual risk factors in this population to optimize decision-making regarding when to recommend spinal surgery.
Supplementary
Search terms
PubMed
(“Aged”[Mesh] OR “Aging”[Mesh] OR aged[tw] OR aging[tw] OR elder*[tw] OR geriatric*[tw] OR 65 year old*[tw] OR senium[tw] OR senior citizen[tw])
AND
(“Scoliosis”[Mesh] OR “Kyphosis”[Mesh] OR “Spondylitis”[Mesh:NoExp] OR spinal deformit*[tw] OR spine deformit*[tw] OR column deformit*[tw] OR spinal deformati*[tw] OR spine deformati*[tw] OR column deformati*[tw] OR spinal malform*[tw] OR spine malform*[tw] OR column malform*[tw] OR spinal anomaly[tw] OR spine anomaly[tw] OR column anomaly[tw] OR bent spin*[tw] OR bent column[tw] OR scoliosis[tw] OR kyphosis[tw] OR kyfosis[tw] OR kyphoscoliosis[tw] OR kyfoscoliosis[tw] OR Scheuermann disease[tw] OR spondylitis [tw])
AND
(“Spinal Fusion”[Mesh] OR “Spinal Curvatures/surgery”[Mesh] OR “scoliosis/surgery”[Mesh] OR “Kyphosis/surgery”[Mesh] OR “Vertebroplasty”[Mesh] OR spine surger*[tw] OR spinal surger*[tw] OR column surger*[tw] OR spine stabiliz*[tw] OR spinal stabiliz*[tw] OR column stabiliz*[tw] OR spine align*[tw] OR spinal align*[tw] OR column align*[tw] OR spine operation[tw] OR spinal operation[tw] OR column operation[tw] OR spine correction[tw] OR spinal correction[tw] OR column correction[tw] OR fuse*[tw] OR fusion[tw] OR kyphoplasty[tw] OR vertebroplasty[tw] OR coronal align*[tw] OR sagittal align*[tw] OR spinopelvic align*[tw] OR spondylosyndesis[tw] OR spondylodesis[tw] OR pedicle subtraction osteotomy[tw] OR ponte osteotomy[tw] OR wedge osteotomy[tw] OR Smith-Peterson osteotomy[tw] OR spinal column osteotomy[tw])
AND
("Postoperative Complications"[Mesh] OR “Death”[Mesh] OR “Blood Loss, Surgical”[Mesh] OR “Postoperative Hemorrhage”[Mesh] OR “Patient Readmission”[Mesh] OR “Reoperation”[Mesh] OR “Infection”[Mesh] OR “Pneumonia”[Mesh] OR “Pulmonary Embolism”[Mesh] OR “Stroke”[Mesh] OR “Thrombosis”[Mesh] OR “Pseudarthrosis”[Mesh] OR “Radiculopathy”[Mesh] OR “Neurologic Manifestations”[Mesh] OR “Myocardial Infarction”[Mesh] OR complicat*[tw] OR death*[tw] OR fatal*[tw] OR postoperative hemorrhage*[tw] OR postoperative haemorrhage*[tw] OR blood loss[tw] OR readmission[tw] OR readmit*[tw] OR reoperat*[tw] OR surgical revision*[tw] OR revision surger*[tw] OR repeat surger*[tw] OR infect*[tw] OR pneumonia[tw] OR embolism[tw] OR stroke[tw] OR thrombos*[tw] OR pseudarthrosis[tw] OR radiculopathy[tw] OR neurolog*[tw] OR myocardial infarction[tw] OR cardiovascular event[tw] OR cerebrovascular event[tw] OR hardware failure[tw])
Total Hits: 3158 (January 21, 2018)
Embase
aged/ OR (aged OR aging OR elder* OR geriatric* OR 65 year old* OR senium OR senior citizen).tw.
AND
spine malformation/ OR scoliosis/ OR kyphoscoliosis/ OR kyphosis/ OR Scheuermann disease/ OR spondylitis/ OR (spinal deformit* OR spine deformit* OR column deformit* OR spinal deformati* OR spine deformati* OR column deformati* OR spinal malform* OR spine malform* OR column malform* OR spinal anomaly OR spine anomaly OR column anomaly OR bent spin* OR bent column OR scoliosis OR kyphosis OR kyfosis OR kyphoscoliosis OR kyfoscoliosis OR Scheuermann disease OR spondylitis).tw.
AND
exp spine fusion/ OR spine stabilization/ OR Kyphoplasty/ OR (spine surger* OR spinal surger* OR column surger* OR spine stabiliz* OR spinal stabiliz* OR column stabiliz* OR spine align* OR spinal align* OR column align* OR spine operation OR spinal operation OR column operation OR spine correction OR spinal correction OR column correction OR fuse* OR fusion OR kyphoplasty OR vertebroplasty OR coronal align* OR sagittal align* OR spinopelvic align* OR spondylosyndesis OR spondylodesis OR pedicle subtraction osteotomy OR ponte osteotomy OR wedge osteotomy OR Smith-Peterson osteotomy OR spinal column osteotomy).tw.
AND
exp postoperative complication/ OR death/ OR exp fatality/ OR operative blood loss/ OR postoperative hemorrhage/ OR exp hospital readmission/ OR exp reoperation/ OR exp surgical infection/ OR pneumonia/ OR exp embolism/ OR cerebrovascular accident/ OR thrombosis/ OR pseudarthrosis/ OR radiculopathy/ OR exp heart infarction/ OR (complicat* OR death OR fatal* OR postoperative hemorrhage OR postoperative haemorrhage OR blood loss OR readmission OR readmit* OR reoperat* OR surgical revision* OR revision surger* OR repeat surger* OR infect* OR pneumonia OR embolism OR stroke OR thrombos* OR pseudarthrosis OR radiculopathy OR neurolog* OR myocardial infarction OR cardiovascular event OR cerebrovascular event OR hardware failure).tw.
Total Hits: 2089 (January 21, 2018)
Cochrane
(“aged” OR “aging” OR elder OR geriatric OR 65 year old OR “senium” OR “senior citizen”) as Title, abstract and keywords
AND
((“scoliosis” OR "kyphosis" OR “kyfosis” OR “kyphoscoliosis” OR “kyfoscholiosis” OR “Scheuermann Disease” OR “spondylitis” OR spinal deformity OR spine deformity OR column deformity OR spinal deformation OR spine deformation OR column deformation OR spinal anomaly OR spine anomaly OR column anomaly OR spinal malformation OR spine malformation OR column malformation OR “bent spine” OR “bent spinal” OR “bent column”) as Title, Abstract and Keywords) OR (MeSH descriptor: [Scoliosis] explode all trees OR MeSH descriptor: [Kyphosis] explode all trees OR MeSH descriptor: [Spondylitis] this term only))
AND
((spinal surgery OR spine surgery OR column surgery OR spinal stabilization OR spine stabilization OR column stabilization OR spinal alignment OR spine alignment OR column alignment OR spinal operation OR spine operation OR column operation OR spinal correction OR spine correction OR column correction OR fuse OR fusion OR “kyphoplasty” OR “vertebroplasty” OR coronal alignment OR sagittal alignment OR spinopelvic alignment OR “spondylosyndesis” OR “spondylodesis” OR “pedicle subtraction osteotomy” OR “ponte osteotomy” OR “wedge osteotomy” OR “Smith-Peterson osteotomy” OR “spinal column osteotomy”) as Title, Abstract and Keywords) OR (MeSH descriptor: [Spinal Fusion] explode all trees OR MeSH descriptor: [Spinal Curvatures] explode all trees and with qualifier(s): [Surgery - SU] OR MeSH descriptor: [Scoliosis] explode all trees and with qualifier(s): [Surgery - SU] OR MeSH descriptor: [Kyphosis] explode all trees and with qualifier(s): [Surgery - SU] OR MeSH descriptor: [Vertebroplasty] explode all trees))
AND
((complication OR fatal OR death OR postoperative hemorrhage OR postoperative haemorrhage OR “blood loss” OR readmission OR readmit OR reoperate OR surgical revision OR revision surgery OR repeat surgery OR infection OR pneumonia OR embolism OR stroke OR thrombosis OR pseudarthrosis OR radiculopathy OR neurologic deficit OR neurological deficit OR myocardial infarction OR cardiovascular event OR cerebrovascular event OR hardware failure) as Title, Abstract and Keywords) OR (MeSH descriptor: [Postoperative Complications] explode all trees OR MeSH descriptor: [Death] explode all trees OR MeSH descriptor: [Blood Loss, Surgical] explode all trees OR MeSH descriptor: [Postoperative Hemorrhage] explode all trees OR MeSH descriptor: [Patient Readmission] explode all trees OR MeSH descriptor: [Reoperation] explode all trees OR MeSH descriptor: [Infection] explode all trees OR MeSH descriptor: [Pneumonia] explode all trees OR MeSH descriptor: [Pulmonary Embolism] explode all trees OR MeSH descriptor: [Stroke] explode all trees OR MeSH descriptor: [Thrombosis] explode all trees OR MeSH descriptor: [Pseudarthrosis] explode all trees OR MeSH descriptor: [Radiculopathy] explode all trees OR MeSH descriptor: [Neurologic Manifestations] explode all trees OR MeSH descriptor: [Myocardial Infarction] explode all trees))
Total Hits: 339 (January 21, 2018)
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Francis RS. Scoliosis screening of 3,000 college-aged women. The Utah Study--phase 2. Phys Ther 1988;68:1513-6. [PubMed]
- Grevitt M, Khazim R, Webb J, et al. The short form-36 health survey questionnaire in spine surgery. J Bone Joint Surg Br 1997;79:48-52. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine (Phila Pa 1976) 2011;36:817-24. [Crossref] [PubMed]
- Kebaish KM, Neubauer PR, Voros GD, et al. Scoliosis in adults aged forty years and older: prevalence and relationship to age, race, and gender. Spine (Phila Pa 1976) 2011;36:731-6. [Crossref] [PubMed]
- Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082-5. [Crossref] [PubMed]
- Robin GC, Span Y, Steinberg R, et al. Scoliosis in the elderly: a follow-up study. Spine (Phila Pa 1976) 1982;7:355-9. [Crossref] [PubMed]
- Jain A, Hassanzadeh H, Puvanesarajah V, et al. Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine 2017;27:534-9. [Crossref] [PubMed]
- Glassman SD, Berven S, Kostuik J, et al. Nonsurgical resource utilization in adult spinal deformity. Spine (Phila Pa 1976) 2006;31:941-7. [Crossref] [PubMed]
- Drazin D, Al-Khouja L, Lagman C, et al. Scoliosis surgery in the elderly: complications, readmissions, reoperations and mortality. J Clin Neurosci 2016;34:158-61. [Crossref] [PubMed]
- Cloyd JM, Acosta FL Jr, Ames CP. Complications and outcomes of lumbar spine surgery in elderly people: a review of the literature. J Am Geriatr Soc 2008;56:1318-27. [Crossref] [PubMed]
- Hassanzadeh H, Jain A, El Dafrawy MH, et al. Clinical results and functional outcomes of primary and revision spinal deformity surgery in adults. J Bone Joint Surg Am 2013;95:1413-9. [Crossref] [PubMed]
- Lapp MA, Bridwell KH, Lenke LG, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine (Phila Pa 1976) 2001;26:973-83. [Crossref] [PubMed]
- Worley N, Marascalchi B, Jalai CM, et al. Predictors of inpatient morbidity and mortality in adult spinal deformity surgery. Eur Spine J 2016;25:819-27. [Crossref] [PubMed]
- Wells G. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. 2004. Accessed February 22, 2019. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [Crossref] [PubMed]
- Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ 1998;316:469-author reply 470-1. [Crossref] [PubMed]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Lydon E, et al. The prevalence of undiagnosed pre-surgical cognitive impairment and its post-surgical clinical impact in elderly patients undergoing surgery for adult spinal deformity. J Spine Surg 2017;3:358-63. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Sergesketter AR, et al. Relationship among koenig depression scale and postoperative outcomes, ambulation, and perception of pain in elderly patients (≥65 years) undergoing elective spinal surgery for adult scoliosis. World Neurosurg 2017;107:471-6. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Vuong VD, et al. Association between baseline cognitive impairment and postoperative delirium in elderly patients undergoing surgery for adult spinal deformity. J Neurosurg Spine 2018;28:103-8. [Crossref] [PubMed]
- Adogwa O, Elsamadicy AA, Fialkoff J, et al. Early ambulation decreases length of hospital stay, perioperative complications and improves functional outcomes in elderly patients undergoing surgery for correction of adult degenerative scoliosis. Spine (Phila Pa 1976) 2017;42:1420-5. [Crossref] [PubMed]
- Akbarnia BA, Mundis GM Jr, Moazzaz P, et al. Anterior column realignment (ACR) for focal kyphotic spinal deformity using a lateral transpsoas approach and ALL release. J Spinal Disord Tech 2014;27:29-39. [Crossref] [PubMed]
- Barrey C, Perrin G, Michel F, et al. Pedicle subtraction osteotomy in the lumbar spine: indications, technical aspects, results and complications. Eur J Orthop Surg Traumatol 2014;24 Suppl 1:S21-30. [Crossref] [PubMed]
- Caputo AM, Michael KW, Chapman TM, et al. Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis. J Clin Neurosci 2013;20:1558-63. [Crossref] [PubMed]
- Cho W, Lenke LG, Bridwell KH, et al. Comparison of spinal deformity surgery in patients with non-insulin-dependent diabetes mellitus (NIDDM) versus controls. Spine (Phila Pa 1976) 2012;37:E978-84. [Crossref] [PubMed]
- Crawford CH 3rd, Carreon LY, Bridwell KH, et al. Long fusions to the sacrum in elderly patients with spinal deformity. Eur Spine J 2012;21:2165-9. [Crossref] [PubMed]
- Deukmedjian AR, Ahmadian A, Bach K, et al. Minimally invasive lateral approach for adult degenerative scoliosis: lessons learned. Neurosurg Focus 2013;35:E4. [Crossref] [PubMed]
- Inoue S, Khashan M, Fujimori T, et al. Analysis of mechanical failure associated with reoperation in spinal fusion to the sacrum in adult spinal deformity. J Orthop Sci 2015;20:609-16. [Crossref] [PubMed]
- Karikari IO, Nimjee SM, Hardin CA, et al. Extreme lateral interbody fusion approach for isolated thoracic and thoracolumbar spine diseases: initial clinical experience and early outcomes. J Spinal Disord Tech 2011;24:368-75. [Crossref] [PubMed]
- Kim WJ, Lee ES, Jeon SH, et al. Correction of osteoporotic fracture deformities with global sagittal imbalance. Clin Orthop Relat Res 2006.75-93. [Crossref] [PubMed]
- Li D, Zhang J, Hu M, et al. Whole segmental pedicle screw fixation combined with posterior lumbar fusion for treating lumbar spinal stenosis associated with degenerative scoliosis in elderly patients. Int J Clin Exp Med 2017;10:15737-42.
- Lonergan T, Place H, Taylor P. Acute complications after adult spinal deformity surgery in patients aged 70 years and older. Clin Spine Surg 2016;29:314-7. [Crossref] [PubMed]
- Scheufler KM, Cyron D, Dohmen H, et al. Less invasive surgical correction of adult degenerative scoliosis. Part II: Complications and clinical outcome. Neurosurgery 2010;67:1609-21; discussion 1621. [Crossref] [PubMed]
- Sweet FA, Sweet A. Transforaminal anterior release for the treatment of fixed sagittal imbalance and segmental kyphosis, minimum 2-year follow-up study. Spine Deform 2015;3:502-11. [Crossref] [PubMed]
- Acosta FL Jr, McClendon J Jr, O'Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: Complications and predictive factors. J Neurosurg Spine 2011;15:667-74. [Crossref] [PubMed]
- Daubs MD, Lenke LG, Cheh G, et al. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine (Phila Pa 1976) 2007;32:2238-44. [Crossref] [PubMed]
- Mok JM, Cloyd JM, Bradford DS, et al. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine (Phila Pa 1976) 2009;34:832-9. [Crossref] [PubMed]
- Gerling MC, Leven D, Passias PG, et al. Risk Factors for reoperation in patients treated surgically for degenerative spondylolisthesis: a subanalysis of the 8-year data from the sport trial. Spine (Phila Pa 1976) 2017;42:1559-69. [Crossref] [PubMed]
- Sato S, Yagi M, Machida M, et al. Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: minimum 5-year follow-up. Spine J 2015;15:1536-44. [Crossref] [PubMed]
- Gazzeri R, Roperto R, Fiore C. Surgical treatment of degenerative and traumatic spinal diseases with expandable screws in patients with osteoporosis: 2-year follow-up clinical study. J Neurosurg Spine 2016;25:610-9. [Crossref] [PubMed]
- Park SB, Chung CK. Strategies of spinal fusion on osteoporotic spine. J Korean Neurosurg Soc 2011;49:317-22. [Crossref] [PubMed]
- Gheno R, Cepparo JM, Rosca CE, et al. Musculoskeletal disorders in the elderly. J Clin Imaging Sci 2012;2:39. [Crossref] [PubMed]
- Montecino-Rodriguez E, Berent-Maoz B, Dorshkind K. Causes, consequences, and reversal of immune system aging. J Clin Invest 2013;123:958-65. [Crossref] [PubMed]
- Postoperative delirium in older adults: best practice statement from the American Geriatrics Society. J Am Coll Surg 2015;220:136-48.e1. [Crossref] [PubMed]
- Sacco RL, Benjamin EJ, Broderick JP, et al. American heart association prevention conference. IV. prevention and rehabilitation of stroke. risk factors. Stroke 1997;28:1507-17. [Crossref] [PubMed]
- Tahiri M, Sikder T, Maimon G, et al. The impact of postoperative complications on the recovery of elderly surgical patients. Surg Endosc 2016;30:1762-70. [Crossref] [PubMed]
- Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 2016;41:62-8. [Crossref] [PubMed]


