
Trends in cervical disc arthroplasty and revisions in the Medicare database
Introduction
Anterior cervical discectomy and fusion (ACDF) was first introduced by Cloward in 1959 and has been considered the “gold standard” for patients suffering from cervical radiculopathy or myelopathy (1). Lied et al. found that ACDF was also an effective procedure in alleviating pain in patients suffering from cervical degenerative disc disease (DDD) (2). Despite all the benefits, patients undergoing primary ACDF have been shown to be susceptible to complications such as hypermobility, pseudarthrosis, dysphagia, and adjacent segment degeneration (ASD) (3). These complications along with the goal of restoring the motion segment have led to several new constructs and technologies. Cervical disc arthroplasty (CDA) has emerged as an option for mitigating these postoperative complications and as a solution for preserving the motion segment without adding stress onto adjacent segments (4-6). CDA accomplishes these goals by maintaining disc space height and by preserving natural physiological forces and motion (7-9). In a 2-year follow up study by Skovrlj et al., patients who underwent primary CDA had mean rate of reoperation of 1.0%, a revision rate of 0.2%, and a removal rate of 1.2% (10). Initially, one of the CDA implants was indicated for use in selective patient populations, specifically ages 18–60 (11). This study found better improvements in neck disability index (NDI) and visual analogue scale (VAS) scores for patients treated with CDA when compared to ACDF (11). The purpose of this study was to determine the trends in CDA utilization, the rates of CDA revision, and demographic considerations in CDA and revision CDA such as age and gender.
Methods
A retrospective review from 2005–2014 was performed using the Medicare Standard Analytical Files from the PearlDiver supercomputer (Pearl Diver Technologies, Fort Wayne, IN, USA). PearlDiver is a commercially available database which has been used extensively for orthopedic-related research. The database is compliant with the Health Information Portability and Affordability Act (HIPAA) and contains the records of over 100 million patients. Information such as diagnosis, procedures, complications, length of stay (LOS), charges, and reimbursements are available, in addition to other information. Patients were queried using the International Classification of Disease, ninth revision (ICD-9) and current terminology procedural (CPT) codes. All patients, in the database, who underwent primary CDA were queried using ICD-9 procedural codes 84.62 and CPT code 22856. Patients who underwent revision CDA were queried using ICD-9 procedure code 84.66. Following the methods by Law et al., the primary outcomes of this study were annual utilization of CDA, annual revision incidence (RI), and the burden of revision rates on the healthcare system (12). Revision burden (RB) was defined as the ratio of revisions to the sum of revision and primary procedures of CDA (12). Furthermore, age, gender, geographical location, Charlson-Comorbidity Index (CCI) and average LOS were also examined in the study. Lastly, average day of surgery costs and reimbursements were also analyzed and compared between the different age cohorts.
Statistical analysis was performed using the programming language R (University of Auckland, New Zealand), with data being primarily descriptive in addition to calculating the compound annual growth rate (CAGR) of primary and revision CDA procedures.
Results
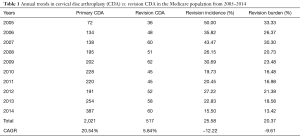
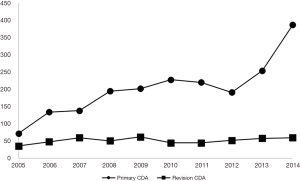
Between 2005–2014, a total of 2,016 and 517 primary CDA and revision CDA procedures were performed in the Medicare database, respectively. The data showed that the CAGR of primary and revision CDA procedures to be 20.54% and 5.84% (P<0.001), respectively. RI and RB demonstrated a CAGR of −12.22% and −9.61%, respectively (Table 1) (Figure 1).
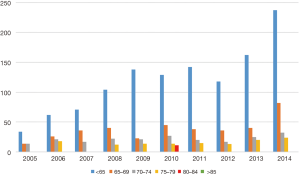
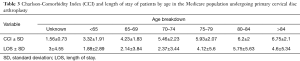
Full table
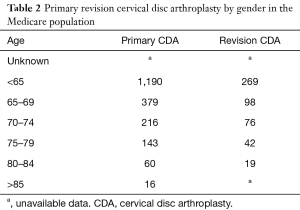
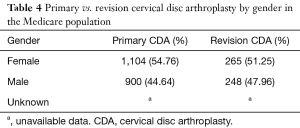
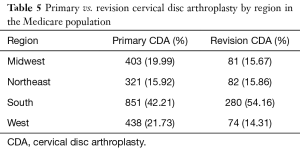
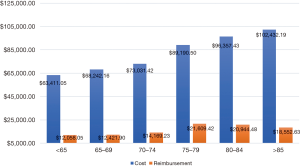
Patients younger than the age of 65, comprised majority of the patients undergoing primary (n=1,190; 57.64%) and revision CDA (n=269; 52.33%) procedures, respectively; however, rates of primary CDA decreased as patients aged (Figure 2) (Table 2). Average CCI and LOS increased with increasing age of patients (Table 3). Females represented majority of the gender undergoing primary (54.76%) and revision (51.25%) CDA procedures (Table 4). Primary CDA was most commonly performed in the South (42.21%), followed by the West (21.73%), Midwest (19.99%), and Northeast (15.92%); whereas revision rates for CDA showed that patients in the South (54.16%) had the highest incidence followed by Northeast (15.86%), Midwest (15.67%), and the West (14.31%) (Table 5). Cost data showed a correlation with age with patients under the age of 65 incurring a total cost of $63,411.05 compared to patients older than the age of 85 incurring a total cost of $102,432.19. Average day of surgery reimbursements in patients younger than 65 was $12,085.05 compared to patients over the age of 85 who incurred an average reimbursement of $18,552.63 (Figure 3).
Full table
Full table
Full table
Full table
Discussion
CDA is a relatively new procedure with landmark papers on CDA listing herniated nucleus pulposus (HNP), radiculopathy/myelopathy, spondylosis, and loss of disc height as the main indications for use of the implant (13-15). The purpose of this study was to examine the trends in CDA utilization and revision rates by analyzing a comprehensive Medicare database between 2005–2014. The study illustrates that CDA utilization has been increasing through the examined study period, whereas RI has decreased.
For years, ACDF has been the gold standard in treatment for symptomatic cervical disease (16). However, the process of fusion has been shown to impact cervical range of motion (ROM) in patients (17,18). Wu et al. found that patients who underwent primary ACDF had statistically significant reduced ROM postoperatively compared to preoperative measurements (18). Compared to ACDF, the literature has shown that patients undergoing CDA have either maintained or had improved ROM.
In a 5-year prospective study performed by Ryu et al., patients who underwent single level CDA placement had a slight increase of 2º in early postoperative ROM at the superior adjacent level (16). This increased ROM was constant at 5-year postoperatively (16). In another 2-year prospective randomized multicenter clinical trial, cervical ROM was compared to patients undergoing either CDA or ACDF. The 24-month outcome results illustrated that patients undergoing primary CDA had maintained their original ROM, whereas this was reduced in the ACDF group. No significant difference was noted between the groups on their NDI score or VAS scores for pain. Furthermore, one patient in the CDA group required a revision procedure, compared to four patients in the ACDF group. The trend towards low reoperation rates of patients undergoing primary CDA found in this study is consistent with the findings in the literature.
Skovrlj et al. reported that the rates of surgical interventions following primary CDA are low (mean, 2.4%; range, 0–4.1%) and these reoperations were mainly attributed to poor patient selection and surgical technique (10). In addition to minimizing postoperative complications, advancements in CDA have led to improved postoperative outcomes and should be considered as an intervention for patients with cervical DDD. Jawahar et al. found that patients above the age of 50 undergoing CDA had greater overall success, higher VAS scores and NDI scores when compared to ACDF (19). A meta-analysis performed by Xie et al. in comparing the safety and efficacy of CDA to ACDF in treating DDD found significant differences between these procedures in terms of neurological success, range of motion, VAS scores of the neck and arm, rates of adverse events, and reoperations (4). This would help to explain the increasing popularity of CDA use in the study with the disproportionate increase in revisions, potentially showing improved survivorship. Our data also demonstrates that CDA use in older patients is also increasing. Annual use has increased at an average rate of 17.97% in the 65–69 age bracket, 4.60% in the 70–74 age bracket, and 7.44% in the 75–79 age bracket. These findings suggest that surgeon comfort with performing CDA in the elderly population continues to rise as well. The results of this study are consistent with that of Lu et al. who found that from 2008–2010, the number of primary CDA procedures performed increased by 11.8% utilizing the Nationwide Inpatient Sample (NIS) database (20).
The study is not without limitations. Being a database analysis study, the validity of the study and results are reliant on the accuracy of procedural coding within the database (21). This translates to the fact that miscoding and noncoding by providers is a potential source of error. It is estimated that 1.3% of coding errors are currently present within the Medicare population (21). Secondly, the study utilized only a single insurer’s data in the analysis, and may not represent a true cross sectional representation of the number of patients undergoing primary and revision CDA in the United States (22). Additionally, comorbidities such as diabetes and smoking were not stratified as variables that could potentially impact the incidence of CDA revision rates (11). Lastly, a selection bias may also be present as patients in the study may enter or exit the database as a natural manifestation (22).
Conclusions
The study illustrates the increasing annual growth of CDA utilization within the Medicare database, indicating that there is an increased patient demand for and/or surgeon comfort with CDA in the United States. This may be attributable to the decreased postoperative complications seen in patients undergoing primary CDA compared to those undergoing ACDF, and improved clinical outcome measurements. The study illustrates recent trends in CDA utilization and increases the awareness of the procedure. Further prospective studies are warranted on determining the efficacy of this increasingly popular procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Due to the retrospective nature of the study, i.e., via a HIPAA compliant database without patient identifiers—no Institutional Review Board (IRB) approval was needed.
References
- Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310-7. [Crossref] [PubMed]
- Lied B, Roenning PA, Sundseth J, et al. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg 2010;10:10. [Crossref] [PubMed]
- Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine (Phila Pa 1976) 2005;30:2138-44. [Crossref] [PubMed]
- Xie L, Liu M, Ding F, et al. Cervical disc arthroplasty (CDA) versus anterior cervical discectomy and fusion (ACDF) in symptomatic cervical degenerative disc diseases (CDDDs): an updated meta-analysis of prospective randomized controlled trials (RCTs). Springerplus 2016;5:1188. [Crossref] [PubMed]
- Zhang J, Meng F, Ding Y, et al. Hybrid Surgery Versus Anterior Cervical Discectomy and Fusion in Multilevel Cervical Disc Diseases: A Meta-Analysis. Medicine (Baltimore) 2016;95. [Crossref] [PubMed]
- Zhong ZM, Li M, Han ZM, et al. Does cervical disc arthroplasty have lower incidence of dysphagia than anterior cervical discectomy and fusion? A meta-analysis. Clin Neurol Neurosurg 2016;146:45-51. [Crossref] [PubMed]
- Burkus JK, Haid RW, Traynelis VC, et al. Long-term clinical and radiographic outcomes of cervical disc replacement with the Prestige disc: results from a prospective randomized controlled clinical trial. J Neurosurg Spine 2010;13:308-18. [Crossref] [PubMed]
- Park JB, Watthanaaphisit T, Riew KD. Timing of development of adjacent-level ossification after anterior cervical arthrodesis with plates. Spine J 2007;7:633-6. [Crossref] [PubMed]
- Yang JY, Song HS, Lee M, et al. Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine (Phila Pa 1976) 2009;34:30-3. [Crossref] [PubMed]
- Skovrlj B, Lee DH, Caridi JM, et al. Reoperations Following Cervical Disc Replacement. Asian Spine J 2015;9:471-82. [Crossref] [PubMed]
- Vaccaro A, Beutler W, Peppelman W, et al. Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty: two-year results from a prospective, randomized, controlled, multicenter investigational device exemption study. Spine (Phila Pa 1976) 2013;38:2227-39. [Crossref] [PubMed]
- Law TY, Sabeh KG, Rosas S, et al. Trends in total ankle arthroplasty and revisions in the Medicare database. Ann Transl Med 2018;6:112. [Crossref] [PubMed]
- Leven D, Meaike J, Radcliff K, et al. Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med 2017;10:160-9. [Crossref] [PubMed]
- Vieweg U, Grochulla F. editors. Manual of Spine Surgery. Berlin Heidelberg: Springer, 2012.
- Murtagh R, Castellvi AE. Motion preservation surgery in the spine. Neuroimaging Clin N Am 2014;24:287-94. [Crossref] [PubMed]
- Pisano A, Helgeson M. Cervical disc replacement surgery: biomechanical properties, postoperative motion, and postoperative activity levels. Curr Rev Musculoskelet Med 2017;10:177-81. [Crossref] [PubMed]
- Kaiser MG, Haid RW Jr, Subach BR, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002;50:229-36; discussion 236-8. [PubMed]
- Wu XD, Wang XW, Yuan W, et al. The effect of multilevel anterior cervical fusion on neck motion. Eur Spine J 2012;21:1368-73. [Crossref] [PubMed]
- Jawahar A, Nunley P. Total disc arthroplasty and anterior cervical discectomy and fusion in cervical spine: competitive or complimentary? Review of the literature. Global Spine J 2012;2:183-6. [Crossref] [PubMed]
- Lu Y, McAnany SJ, Hecht AC, et al. Utilization trends of cervical artificial disc replacement after FDA approval compared with anterior cervical fusion: adoption of new technology. Spine (Phila Pa 1976) 2014;39:249-55. [Crossref] [PubMed]
- Cancienne JM, Dempsey IJ, Holzgrefe RE, et al. Is Hepatitis C Infection Associated With a Higher Risk of Complications After Total Shoulder Arthroplasty? Clin Orthop Relat Res 2016;474:2664-9. [Crossref] [PubMed]
- Burrus MT, Werner BC, Cancienne JM, et al. Shoulder arthroplasty in patients with Parkinson's disease is associated with increased complications. J Shoulder Elbow Surg 2015;24:1881-7. [Crossref] [PubMed]


