
Spine surgery registries: hope for evidence-based spinal care?
Short communications
Orthopedic registries have been kept for half a century (1,2). They have created a powerful model for evidence-based arthroplasty and surveillance. Spine surgery is widespread and the numbers are increasing. There is the little research into the harm or benefit of spine surgery. The few available randomized trials have been criticized for poor generalizability (3). Registries are pragmatic, long-term observational studies with large numbers. This study aimed to describe the perceptions of decision-makers in major orthopedic centers regarding the value, implementation and use of spine surgery registries.
A 33-item survey was sent to CEOs and heads of spine surgery of the International Society of Orthopedic Centers (ISOC). ISOC includes 21 hospitals worldwide with a special focus on high-quality musculoskeletal care (4).
Participants were asked whether centers have a prospective spine registry; its format (hardcopy, electronic, or a combination); whether it is an internal, external, or combined registry (and if yes, which registry); and from when; which types of questionnaires and information are included; number of surgeons and staff involved; whether non-surgeon personnel are assigned to the registry (e.g., IT, data collection, data insertion); how many hours of work (person-hours) are dedicated to the registry; the degree of satisfaction of the medical staff relative to the participation in the registry; and the perceived quality, research usefulness, management value, and global value of the registry.
For centers without a spine registry, questions included reasons why a registry has not been implemented (organizational, funding, small numbers, difficulty with follow-up); willingness to participate in a registry; degree of priority; the limiting factors (e.g., economical, organizational); perception of the cost of implementation and operation; and CEOs’ availability to allocate resources.
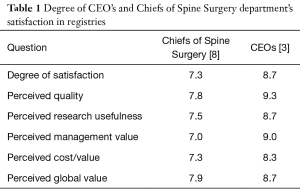
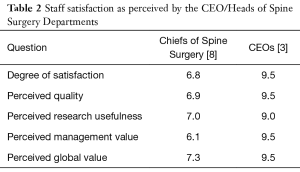
Twelve out of 20 member centers (60%) replied to the survey. Seven have working registries; 5 in Europe and 2 in North America. The oldest one started in Sweden in 1993 and the most recent in Italy in 2015 (Table 1). Allocated human resources (person-hours per week) varied from 0–5 in the Swedish registry, to more than 50 hours in the Italian registry. Most registries allocated 10 to 40 person-hours weekly. Five registries were combined electronic and paper; two were only electronic. Six were a combination of internal and external registries; 1 institution had an external registry (Table 2).
Full table
Full table
Five institutions reported not having a spinal registry. The reasons were funding (4), reduced case-load (2), organizational difficulties (3). Two institutions considered a spine registry a priority in the short-middle term, whereas 3 institutions considered it a priority for the long term. Finally, 2 institutions estimated the launching cost to be around $10,000, whereas 2 institutions estimated the cost to be $50,000. The estimations for the cost/year were distributed more evenly: $10,000 [2], $20,000 [1], $50,000 [1].
The perceived value of the spinal registry was high among both CEOs and Heads of Spine Surgery. Interestingly, clinicians perceived that their staff were less satisfied with the registry than they were, while the CEOs felt the staff was more satisfied than they were. This could reflect a more realistic perception (from clinicians) of the burden of work related to a registry. More experienced registries were less resource-consuming, though all registries consumed specific human resources. Limiting factors to implementation of registries were cost and organizational difficulties. The perceived cost of registries (reflecting the willingness to allocate resources) was modest (around $10,000 per year).
Surgery registries, and specifically spine registries, provide high levels of evidence in an area in which RCTs are often difficult to execute or unfeasible for ethical reasons (5). The cost of implementing a registry is limited in comparison to RCTs, whereas the information obtained from the registries is of high quality and generalizable (6). Understanding the specific advantages and disadvantages of keeping a spine registry and the cooperation with institutions that already have registries will help to further develop registries not only as valuable research tools but also as a means to achieve the highest standard of care.
Spinal disease is a burden. Society cannot afford unnecessary surgery nor renounce to cure patients with effective treatments. Spine registries can pragmatically fill our knowledge gap by turning every operated patient into a study participant.
Acknowledgements
The authors thank Grazia Fontaneto (MSc) and Rachel Applefield (MSc) for their assistance in the collection of data.
Funding: This project is financed by the National Health System of Italy (Project Code: CO-2016-02364645).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Herberts P, Ahnfelt L, Malchau H, et al. Multicenter clinical trials and their value in assessing total joint arthroplasty. Clin Orthop Relat Res 1989.48-55. [PubMed]
- Ahnfelt L, Herberts P, Malchau H, et al. Prognosis of total hip replacement. A Swedish multicenter study of 4,664 revisions. Acta Orthop Scand Suppl 1990;238:1-26. [PubMed]
- Aebi M. Vertebroplasty: about sense and nonsense of uncontrolled "controlled randomized prospective trials". Eur Spine J 2009;18:1247-8. [Crossref] [PubMed]
- Drago L, Lidgren L, Bottinelli E, et al. Mapping of Microbiological Procedures by the Members of the International Society of Orthopaedic Centers (ISOC) for Diagnosis of Periprosthetic Infections. J Clin Microbiol 2016;54:1402-3. [Crossref] [PubMed]
- Jacobs WC, Kruyt MC, Verbout AJ, et al. Effect of methodological quality measures in spinal surgery research: a metaepidemiological study. Spine J 2012;12:339-48. [Crossref] [PubMed]
- van Hooff ML, Jacobs WC, Willems PC, et al. Evidence and practice in spine registries. Acta Orthop 2015;86:534-44. [Crossref] [PubMed]


