
Cervical sagittal alignment and the impact of posterior spinal instrumented fusion in patients with Lenke type 1 adolescent idiopathic scoliosis
Introduction
Clinical decision making, preoperative planning, and surgical correction for adolescent idiopathic scoliosis (AIS) has traditionally focused on obtaining the maximum coronal plane correction to improve cosmesis and function (1,2). More recently, restoring sagittal alignment has also received increasing attention in AIS patients, correlating with positive health-related quality of life (HRQOL) outcomes in multiple studies (3,4). Additionally, it has been suggested that a dynamic inter-play may exist between the degree of thoracic kyphosis and nearby cervical and lumbar curvatures (1,2,5-11). Multiple studies have emphasized the importance of restoring thoracic kyphosis in the hypo-kyphotic AIS patients to maintain a normal lumbar lordosis (3,12,13). In the long-term, iatrogenic loss of lumbar lordosis has been shown to correlate with marked morbidity and disability (14). Therefore, surgical correction techniques in AIS have gradually evolved to include restoration of the sagittal balance, and this became a primary focus for many surgeons.
In this realm, cervical sagittal alignment (CSA) has also emerged as one of the variables that may correlate with clinical and functional outcomes in AIS patients undergoing surgical correction (5,6,8,10,11). Previous studies have noted a prevalence of cervical kyphosis in the AIS population, and that thoracolumbar fusion results in alternations in cervical sagittal profile (15-17). However, it is unclear whether this kyphosis would change following surgical correction and how it may affect clinical and patient-reported outcomes. Several studies have focused on studying the cervical sagittal plane parameters in patients with deformity, while few have investigated the impact of surgical correction on CSA.
In this study, we aimed to capture the baseline cervical sagittal characteristics and evaluate the changes in CSA in a cohort of AIS patients with Lenke type I curves following posterior spinal instrumented fusion (PSIF).
Methods
Patient selection
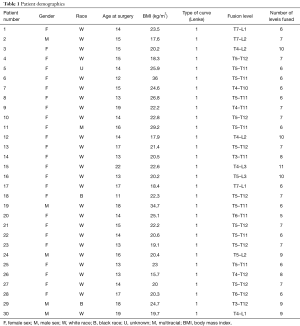
Following institutional review board (IRB) approval, we evaluated the prospectively collected single-institute database of patients who had surgical correction for AIS between January 1, 2015 and September 1, 2017 aged between 10 to 25 years old. The initial search yielded 270 patients who were treated with PSIF for AIS. Among those patients, we applied the following inclusion criteria to identify the study cohort: (I) patients who had Lenke type 1 curves, (II) patients with adequate pre-operative and post-operative radiographs (posterior-anterior and lateral), (III) patients who had a minimum radiographic follow-up of 6 months, and (IV) patients who were treated with the same standard rod instrumentation system. In addition, the following exclusion criteria were applied: (I) patients with neuromuscular disorders, (II) patients with prior spine surgery, and (III) those who received greater than Schwab-2 osteotomies. Applying these criteria yielded a total of 30 patients that were included in our final analysis. These patients had a mean age of 15 years (range, 11 to 19 years). There were 25 girls and 5 boys. Mean body mass index (BMI) was 22.5 kg/m2 (range, 15.7 to 36 kg/m2). On average, 7 spinal segments were fused (range, 5 to 11 levels; Table 1). In all surgeries, a single, standard pedicle screw and rod system was utilized. Three board certified orthopaedic surgeons performed all surgeries at a major academic medical center. Immediate pre-operative radiographs and 6-month post-operative radiographs were measured.
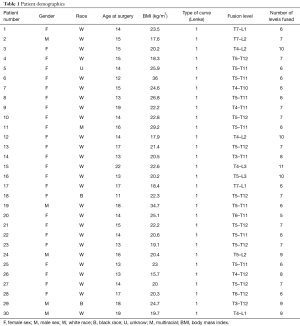
Full table
Study endpoints
The C2 to C7 angle, C0 to C2 angle, C2 to C7 sagittal vertical axis (SVA), McGregor slope (McGS), and the T1 slope angle were measured preoperatively and at final follow-up on lateral cervical standing radiographs. C2–C7 lordosis was defined as the Cobb angle between the lower endplates of C2 and C7. C0–C2 lordosis was measured as the angle between the line from the anterosuperior border of the atlas to the inferior end of the occiput and lower endplates of C2. C2–C7 SVA was measured as the distance from the posterosuperior corner of C7 and the vertical line from the center of the C2 body. The McGS and T1 slope (18) were defined as the angle of the McGregor line and T1 superior end plate against a horizontal line, respectively. Kyphotic measurements were assigned negative values, while positive values were used to describe lordotic measurements. For every patient, two senior authors performed the measurements twice independently. For every patient, two senior authors performed the measurements twice independently. Basic descriptive statistical analysis was used.
Data analysis
Statistical analysis was mainly descriptive. Patient data was entered into an Excel spreadsheet (Excel, Microsoft Corporation, Redmond, Washington, USA) after removing patient identifiers. Pre-operative and post-operative measurements in each category were compared using the paired sample t-test. All statistical analysis was performed using SPSS version 24 (IBM Corporation, Armonk, New York, USA). A cutoff P value of 0.05 was set to determine statistical significance.
Results
Overall, CSA improved in all patients post-operatively, with 19/30 (63%) resulting in improved lordosis. Pre-operatively, mean C2–C7 cervical lordosis was −4.3°, which improved to −0.5° postoperatively (P=0.075), with a mean difference of 3.7°. Simultaneously, mean C0–C2, C2–C7 SVA, McGS, and T1 slope changed from 17° (range, −18° to 41°), 26.5 mm (range, 10 to 45 mm), 4° (range, −7.5° to 25°), and 17.4° (range, 1° to 42°) to 16° (range, 0° to 34.4°, mean difference =1.01°, and P=0.548), 28.2 mm (range, 9 to 57 mm, mean difference =2 mm, and P=0.244), 4.03°, (range, −7.8° to 25°, mean difference =0.16, and P=0.916), and 18° (range, 5.4° to 42°, mean difference =0.37, and P=0.761) (mean change of C2–C7 angle of 3.76°). These results are illustrated in Tables 2,3.
Full table
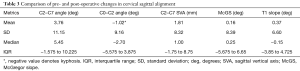
Full table
Discussion
Despite the increasing appreciation in sagittal plane alignment with surgical correction for AIS, our current knowledge on CSA changes in these patients, particularly those with a major thoracic or proximal curve, is lacking. In this study, we aimed to evaluate changes in CSA and the effect of PSIF on cervical alignment in a cohort of AIS patients with Lenke type 1 curves. Our results demonstrated that CSA trended towards improved lordosis, primarily with an improvement in sub-axial cervical lordosis and slight improvement in McGregor and T1 slopes. AIS patients with Lenke type 1 curves are frequently hypo-kyphotic, which has been shown to correlate with compensatory cervical kyphosis. Cervical kyphosis has been associated with chronic neck pain, disability, and worse HRQOL (19).
There are several limitations to this study. The main limitation is the small sample size, which may have precluded our analysis from reaching a point of statistical significance in the pre- to post-test cohort analysis. However, the consistent findings in our results may point to a degree of internal validity. Additionally, the relatively short follow-up may not reflect the true long-term results. However, we mainly aimed to evaluate patients at 6 months to capture immediate post-surgical changes in sagittal alignment while allowing for settling and resolution of pain and muscle spasm in the early post-operative period. Furthermore, other thoracic sagittal plane parameters were not measured, including the degree of thoracic kyphosis. Nevertheless, all patients had the same curve type and we mainly aimed to study changes in the cervical region, which have not been well-studied in previous published reports.
Previous studies mainly investigated the effect of AIS deformity on CSA. Lee et al. (15) performed an analysis of 181 asymptomatic children to determine normal sagittal spine parameters. They found significant variability in their study. Cervical kyphosis was found in 40% of their study patients. Mean cervical lordosis was −4.8±12.0 degrees. Similarly, Yu et al. (16) analyzed the CSA in 120 AIS patients. They categorized patients into four categories: cervical non-kyphosis, cervical kyphosis, cervical-middle-thoracic kyphosis, and cervical-lower-thoracic kyphosis. They found that 40% of their study patients exhibited cervical kyphosis and that the cervical angles and cervicothoracic angles were highly correlated. Despite this deformity in cervical alignment, global sagittal balance was still well maintained in this population.
Only few studies have attempted to quantify the effect of AIS surgical correction on CSA. Roussouly et al. (17) evaluated pre- and post-operative radiographic parameters in 132 AIS and adult scoliosis patients to evaluate various changes in global sagittal alignment including cervical lordosis by corrective surgery. They found that cervical hypolordosis and thoracic hypokyphosis were prevalent in the AIS population they studied. They also noted that thoracolumbar fusion significantly changed global sagittal alignment. Specifically, improvements in cervical lordosis and thoracic kyphosis were associated with pre-operative thoracic kyphosis. Patients with pre-operative thoracic hypokyphosis had improved cervical lordosis and thoracic kyphosis post-operatively, whereas the inverse appeared to be true in patients with normal pre-operative thoracic kyphosis. In a recent study by Cho et al. (11), the authors investigated CSA changes in 318 patients who underwent surgical correction for AIS and compared the pre- and post-operative parameters according to the curve type (double major, single thoracic, and double thoracic curves) in two cohorts with either pre-operative cervical kyphosis or lordosis. Regardless of the curve type, they reported an increase in C2–C7 lordosis (range, −5.8° to −1.1°; P<0.001) and a decrease in C2–C7 SVA (range, 24.2 to 20.0 mm; P<0.001) postoperatively.
Additionally, Youn et al. (20) studied the relationship between CSA and HRQOL in AIS. They measured pre- and post-operative CSA and administered the Korean version of the Scoliosis Research Society Outcomes Questionnaire (SRS-22) and the Short Form Health Survey (SF-36) at last follow-up visits in 67 patients. They reported significant changes in cervical sagittal parameters in their study population and found that T1 slope and C2–C7 SVA were significant predictors of HRQOL. Similarly, Bao et al. evaluated the neck—disability index in asymptomatic and symptomatic adult patients and found that the C2–C7 SVA, McGS, and the slope of line of sight differed the most between these groups; C2–C7 angle did not show a statistical difference (21).
Conclusions
In conclusion, this study highlighted the changes in CSA in AIS patients and demonstrated a trend toward cervical lordosis restoration in these patients, reinforcing previous studies. Despite the limitations, we believe it will expand our current knowledge and provide an impetus for future studies. Larger, prospective, multi-center studies will help us further appreciate the impact of PSIF in AIS patients on the cervical sagittal profile, the effect of cervical sagittal profile on patient reported outcomes, and, potentially, ways to address cervical sagittal malalignment when undertaking the surgical correction for specific curve types in AIS.
Acknowledgements
None.
Footnote
Conflicts of Interest: TE Mroz: Cervical Spine Research Society: Board or committee member; North American Spine Society: Board or committee member; Pearl Diver, Inc.: Stock or stock Options; SpineLine, Editor. Global Spine Journal, Deputy Editor: Editorial or governing board; Stryker: IP royalties; Paid consultant. MP Steinmetz: AANS/CNS Section on Disorders of the Spine and Peripheral Nerves: Board or committee member; Biomet: IP royalties; Council of State Neurosurgical Societies: Board or committee member; Elsevier: Publishing royalties, financial or material support; Globus Medical: Paid consultant; Paid presenter or speaker; Intellirod: Paid presenter or speaker; Stryker: Paid presenter or speaker; World Neurosurgery and Operative Neurosurgery: Editorial or governing board. RC Goodwin. K2M: Paid consultant; Orthpediatrics: Paid consultant; Stryker: Paid consultant. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of the Cleveland Clinic Foundation (# 17-1135) and informed consent was waived.
References
- Lehman RA, Lenke LG, Keeler KA, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976) 2008;33:1598-604. [Crossref] [PubMed]
- Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005;30:1602-9. [Crossref] [PubMed]
- Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8. [Crossref] [PubMed]
- Le Huec JC, Faundez A, Dominguez D, et al. Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 2015;39:87-95. [Crossref] [PubMed]
- Wang L, Liu X. Cervical sagittal alignment in adolescent idiopathic scoliosis patients (Lenke type 1–6). J Orthop Sci 2017;22:254-9. [Crossref] [PubMed]
- Legarreta CA, Barrios C, Rositto GE, et al. Cervical and Thoracic Sagittal Misalignment After Surgery for Adolescent Idiopathic Scoliosis. Spine (Phila Pa 1976) 2014;39:1330-7. [Crossref] [PubMed]
- Zhao J, Chen Z, Yang M, et al. Does spinal fusion to T2, T3, or T4 affects sagittal alignment of the cervical spine in Lenke 1 AIS patients. Medicine (Baltimore) 2018;97. [Crossref] [PubMed]
- Hayashi K, Toyoda H, Terai H, et al. Cervical lordotic alignment following posterior spinal fusion for adolescent idiopathic scoliosis: reciprocal changes and risk factors for malalignment. J Neurosurg Pediatr 2017;19:440-7. [Crossref] [PubMed]
- Sucato DJ, Agrawal S, O’Brien MF, et al. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine (Phila Pa 1976) 2008;33:2630-6. [Crossref] [PubMed]
- Zhu C, Yang X, Zhou B, et al. Cervical kyphosis in patients with Lenke type 1 adolescent idiopathic scoliosis: the prediction of thoracic inlet angle. BMC Musculoskelet Disord 2017;18:220. [Crossref] [PubMed]
- Cho JH, Hwang CJ, Choi YH, et al. Cervical sagittal alignment in patients with adolescent idiopathic scoliosis: is it corrected by surgery? J Neurosurg Pediatr 2018;21:292-301. [Crossref] [PubMed]
- Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine 2012;16:547-64. [Crossref] [PubMed]
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30:2024-9. [Crossref] [PubMed]
- Barry JJ, Yucekul A, Theologis AA, et al. Spinal Realignment for Adult Deformity: Three-column Osteotomies Alter Total Hip Acetabular Component Positioning. J Am Acad Orthop Surg 2017;25:125-32. [Crossref] [PubMed]
- Lee CS, Noh H, Lee DH, et al. Analysis of Sagittal Spinal Alignment in 181 Asymptomatic Children. J Spinal Disord Tech 2012;25:E259-63. [Crossref] [PubMed]
- Yu M, Silvestre C, Mouton T, et al. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: a morphological classification of 120 cases. Eur Spine J 2013;22:2372-81. [Crossref] [PubMed]
- Roussouly P, Labelle H, Rouissi J, et al. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J 2013;22 Suppl 2:S203-15. [Crossref] [PubMed]
- Schwab F, Lafage V, Patel A, et al. Sagittal Plane Considerations and the Pelvis in the Adult Patient. Spine (Phila Pa 1976) 2009;34:1828-33. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2015;76 Suppl 1:S14-21; discussion S21.
- Youn MS, Shin JK, Goh TS, et al. Relationship between cervical sagittal alignment and health-related quality of life in adolescent idiopathic scoliosis. Eur Spine J 2016;25:3114-9. [Crossref] [PubMed]
- Bao H, Varghese J, Lafage R, et al. Principal Radiographic Characteristics for Cervical Spinal Deformity: A Health-related Quality-of-life Analysis. Spine (Phila Pa 1976) 2017;42:1375-82. [Crossref] [PubMed]


