
Efficacy and complications of the use of Gardner-Wells Tongs: a systematic review
Introduction
Originally employed by Alfred S. Taylor in 1929 for cervical fractures, skull-based traction for spinal injuries, as well as other traction devices, have continued to increase following World War II (1). Introduced in 1973 by Dr. James Gardner, Gardner-Wells Tongs (GWT) have become a popular method of spinal traction (2,3). There are several uses for GWT, including the treatment of cervical spine fractures, patient positioning inside the operating room, and skeletal traction during spinal deformity surgery. Aside from GWT, different apparatuses have been utilized for skeletal traction, including Crutchfield’s caliper, Cone’s caliper, Blackburn’s caliper, and halo traction (3,4). Skeletal traction may be utilized in an emergent setting, as in the reduction of facet joint fractures and dislocations (2-4). Furthermore, it plays a role in the non-operative management of these injuries. As Kepler et al. demonstrated, nearly 65% of their injuries underwent successful closed reduction with GWT (4).
GWT have many advantages that have led to their increased popularity and usage. These include the relative ease of use, sterile technique, lack of incisions, reduced screw pullout, and elimination of burr holes (5). However, GWT usage is not without risks and complications, as several case reports have demonstrated (3,5,6). In addition, GWT are bulky in the coronal plane and may cause issues with patient positioning and turning, impeding nursing care (6).
Cervical traction, produced by various means, has been the initial step in definitive management of cervical spine fractures and dislocations for over 70 years (1). As cervical fractures become more common with increasing automobile use, skeletal traction has been increasingly utilized to treat such injuries (1). Fractures, dislocations, and fracture-dislocations of the cervical spine can all be managed with a form of cervical traction (1,7). Skeletal traction is also utilized during spinal deformity surgeries (scoliosis) (8). Intraoperatively, traction has been shown to serve three purposes: deformity correction, spinal stabilization, and head elevation, thereby permitting a safer surgical correction of spinal deformities (8).
The GWT consist of a rigid bar that follows the coronal contour of the skull with a hole on each end that accommodates placement of a screw into the outer table of the skull. These screws are tilted in the vector of the pull, minimizing screw pullout during traction. This change in screw angle offered the GWT an advantage over prior cervical traction devices (9,10). On one end, a retractable spring is present that is calibrated to display the pressure in pounds (lbs) (2). In one study, a vector of 45 degrees and 15 lbs allowed the head of the patient to have minimal contact with the face cushion, thereby limiting the occurrence of facial ulcers during long procedures performed with the patient in a prone position (8). This type of positioning may also decrease intraocular pressure and thus prevent blindness, a rare yet devastating complication of lengthy spine surgery performed in a prone position (11).
To the authors’ knowledge, a systematic review of the complications of GWT has not been performed, although various case reports have been described (3,5,6). With increasing frequency of cervical traction utilization due to automobile accidents, as well as increasing popularity of GWT utilization in the United States, our goal was to perform a systematic review of the literature to assess the risks and complications associated with the use of GWT (1-3).
Methods
A comprehensive search of PubMed, Wiley Online Library, and SCOPUS was performed in accordance with PRISMA guidelines for all literature examining the efficacy, risks, and complications associated with the use of GWT. The initial search utilized the following key terms: gardner wells, gardner-wells, gardner tong, and/or complications. References from retrieved studies were further reviewed to identify additional articles of interest.
First, inclusion and exclusion criteria were independently applied to study titles and abstracts by two reviewers (Hesham Saleh, Ahmed Saleh) to identify potentially eligible studies. Studies discussing the efficacy, rates of success, complications, advantages/disadvantages of GWT were included. Studies that tangentially mentioned the use of GWT but focused on other topics, such as surgical procedures, were excluded. Those studies considered potentially eligible were retrieved in full for review. Again, two reviewers independently applied inclusion and exclusion criteria (Hesham Saleh, Ahmed Saleh). All study methods—including prospective, retrospective, case reports, case series, and biomechanical—were included, as well as review articles pertaining to the use of GWT. The search methodology for relevant articles is summarized in Figure 1. Studies that met inclusion criteria were systematically reviewed for methodology (i.e., year of publication, sample size, study type/clinical report, inclusion/exclusion criteria), demographics (i.e., age, gender), and clinical outcomes (i.e., injury status, neurological status, follow-up period).
Results
Our original search of the literature returned 108 articles. After application of our inclusion and exclusion criteria, 23 articles were included in this systematic review for final analysis. There were eight case reports, one case series, three prospective studies, three retrospective studies, four biomechanical studies, and four review papers. As per PRISMA guidelines, it is necessary to assess the biases in the studies utilized in this review. The designs of many of these studies carry inherent biases. Case reports and case series, for example, are subject to publication bias and lack generalizability, as the authors have chosen these patients due to significant findings which are often rare in the medical community. By design, retrospective studies are unable to establish cause-effect relationships. However, these study designs are limited by the incidence of observed complications of GWT.
There is paucity in the literature regarding complications associated with the use of GWT. These complications will be discussed in this section, along with any available rates of incidence. Table 1 provides a summary of the studies included in this systematic review and the complications observed.
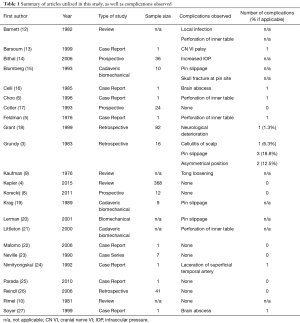
Full table
One study in the literature reported a complication rate of skull traction. In a study of 16 patients, complications were observed in 6 (37.5%) patients (3). These complications included loosening of the pins (3; 18.8%), asymmetrical positioning of the pins (2; 12.5%), and superficial infection (1; 6.3%) (3). However, this author concluded that “no serious complication was noted, but the marked protrusion of the screws made turning to the full lateral position difficult” (3).
Perhaps the most serious complication observed is perforation of the pins through the skull. Incidence rates of this complication are not available in the literature, but rather, cases are sporadically reported. The first such case occurred in 1984; on day 35 of traction, the patient felt sudden, severe pain at the pin entry site (5). Radiography performed revealed that one of the pins had perforated the inner table of the skull by 5 millimeters (mm). However, the patient did not develop any neurological deficits or infections, but was treated prophylactically with antibiotics (25). Another similar case was reported in 1996; on day 37 of traction, the pin entry site appeared mildly inflamed (6). On day 42, the patient reported a headache, vomiting, and fever. Radiography revealed that the pin had penetrated 5 mm into the inner table of the skull. Shortly thereafter, the patient had transient episodes of contralateral weakness and numbness. Neurology was consulted, and these symptoms were attributed to a transient ischemic attack, with complete resolution by his four-month visit (21). There were no studies of cranial perforation during acute reduction (18). One study utilized cadaveric samples to examine the force necessary to penetrate the inner table of the skull. They reported that the average weight necessary for perforation of a properly placed pin was 162 lbs (20) far exceeding the 140 lb maximum weight utilized clinically.
Whereas perforation is uncommon, loss of attachment of the pins appears to be more common and more widely cited in the literature. It was reported that loss of attachment, or “pull-off,” generally occurred days to weeks following initial traction (19). This phenomenon may be due to resorption of the bone underlying the pin due to pressure or infection (26). One study investigated the mean weight needed to pullout the pins. For a stainless steel pin, an average of 225 lbs was necessary, which is significantly more than the acceptable weight for clinical settings (15). Pull-out was observed with MRI-compatible tongs at mean weights of 75 lbs (4).
Brain abscess is another rare complication of GWT. Although an incidence rate pertaining specifically to the use of these tongs is unavailable in the literature, it is estimated that abscesses occur in 0.4–0.7% of cases utilizing any method of cervical traction (16). The abscess is usually caused by a superficial skin infection which tracts through the pin entry site, thus causing a brain abscess (27). This may occur when the pins loosen and are retightened, as this allows entry of bacteria through the pin entry site (27). Sterile dressing and pin site care are considered good preventive measures (27).
Neurovascular complications, although rare, have been reported in the literature as well. There is one case report available regarding the development of a transient Abducens Nerve (CN VI) palsy following cervical traction with GWT during surgery (13). Following surgery, the patient complained of diplopia and was found to have a CN VI palsy. His symptoms completely resolved 6 months post-operatively (13). Complications with other cranial nerve palsies, including CN IX, XI, and XII, have been reported with other types of cervical traction (i.e., halo), but not with GWT (13).
Vascular injury with GWT has also been reported. One case report describes a laceration of the superficial temporal artery (24). Cervical traction was applied during surgery with GWT; 10 weeks post-operatively, the pin insertion site did not heal, and the patient experienced intermittent pulsatile bleeding through the eschar (24). It was determined that he had suffered a laceration to the superficial temporal artery, likely secondary to improper placement of the pin. The tongs are generally placed 1–2 cm posterior to the course of the superficial temporal artery, just above the pinna. Bleeding is not unusual with the use of GWT, but it often subsides spontaneously in a short amount of time.
Discussion
GWT have become popular in the United States due to their ease of use, and effectiveness in reducing cervical dislocations in a traumatic setting. Several advantages over previous traction devices include the lack of skin incisions, antiseptic instead of aseptic technique, and the lack of drill holes (3,5,6). GWT have been shown to be effective in the reduction of cervical dislocations with up to 140 lbs of traction being utilized. In addition to their effectiveness in reducing cervical dislocations, GWT have also been utilized in spinal surgery when patients are in prone position (28).
According to the manufacturer’s recommendation, the tongs should be adjusted to produce 1 mm stem protrusion. As there is no indicator line, one study showed that on average, orthopedic surgeons placed the stem with 0.68 mm protrusion, resulting in an average pull-off strength of 112 lbs, or a decrease of 19% in the strength of the tongs (18,21,26).
Early closed reduction is safe and effective, and helps promote neurological recovery following cervical spine injuries (18). Variable rates of successful reduction utilizing GWT have been reported in the literature, ranging from 30–100% (4,26). This wide range of success may possibly be attributed to differences in pin positioning, surgeon experience, and patient population size. One study of 82 patients reported that closed reduction was successfully achieved in 96.7% of patients (15). On average, this occurred within 2.1 hours from the time of arrival in the emergency department, with a mean of 30% of the patient’s body weight (15).
The handful of case reports/series and limited literature regarding complications associated with GWT testifies to the safe use of this traction device. Publication bias certainly plays a role in the decision to publish such reports. Complications from GWT are indeed a rare phenomenon. Only one study provided a complication rate—37.5% (3). The small sample size (n=16) may have contributed to the inflation of this rate. In addition, this was a select group of patients, all with traumatic tetraplegia, limiting the generalizability of this study to our standard patients. Lastly, 2/16 (12.5%) of the complications included are asymmetric pin positioning. It is possible that improper positioning of the pins contributed to these complications. Despite these complications, the authors recognized that no serious complications was noted (3).
GWT have also been shown to be safe and effective for use by special populations. One study demonstrated that Gardner tongs placed by skilled nurses on patients with cervical spine injuries who were transmitted by aircraft from one hospital to another is a safe and effective method of cervical traction (23). One patient who had sustained significant subluxation at C6–C7 was stabilized utilizing GWT for a 3.5-hour flight, without complications (13). Another case report described a pregnant patient who sustained a C4–C5 anterior subluxation and was subsequently stabilized in GWT. This patient went into spontaneous labor with the tongs in place, and ultimately had a normal parturition and full neurological recovery (22).
Conclusions
While GWT have become popular, partly due to the lack of a skin incision and ease of use, documented rates of complications are not readily available (8). In our review of the efficacy and complications associated with the use of GWT, we found a paucity of published literature on the topic with most papers consisting of case reports. The lone study that reported complication rates cited a complication rate of 37.5%, consisting of loosening pins, asymmetric pins, and infection (3). However, this rate is limited by small sample size, study patient selection, and proper pin placement. These complications were minor, however, and the authors conceded that no serious complications were observed. Despite the sparse available literature, the complication rate is low, and often associated with only minor and transient complications which can be easily managed. We conclude that GWT are safe to use with no serious complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Loeser JD. History of skeletal traction in the treatment of cervical spine injuries. J Neurosurg 1970;33:54-9. [Crossref] [PubMed]
- Gardner WJ. The principle of spring-loaded points for cervical traction: technical note. J Neurosurg 1973;39:543-4. [Crossref] [PubMed]
- Grundy DJ. Skull traction and its complications. Injury 1983;15:173-7. [Crossref] [PubMed]
- Kepler CK, Vaccaro AR, Chen E, et al. Treatment of isolated cervical facet fractures: a systematic review. J Neurosurg Spine 2015.1-8. [Epub ahead of print]. [PubMed]
- Feldman RA, Khayyat GF. Perforation of the skull by a Gardner Wells tong. Case report. J Neurosurg 1976;44:119-20. [Crossref] [PubMed]
- Choo JH, Liu WY, Kumar VP. Complications from the Gardner-Wells tongs. Injury 1996;27:512-3. [Crossref] [PubMed]
- McKenzie KG. Fracture, Dislocation, and Fracture-Dislocations of the cervical spine. Can Med Assoc J 1935;32:263-9. [PubMed]
- Koreckij J, Price N, Schwend R. Vectored Cranial-Cervical Traction Limits Facial Contact Pressure from Prone Positioning During Posterior Spinal Deformity Surgery. Spine (Phila Pa 1976) 2011;36:E993-7. [Crossref] [PubMed]
- Kaufman HH. Modification for the gardner wells skull traction tongs. Surgical Neurology 1976;6:220. [PubMed]
- Rimel RW, Butler AB, Winn HR. Modified skull tongs for cervical traction: technical note. J Neurosurg 1981;55:848-9. [Crossref] [PubMed]
- Su AW, Lin SC, Larson AN. Perioperative vision loss in spine surgery and other orthopaedic procedures. J Am Acad Orthop Surg 2016;24:702-10. [Crossref] [PubMed]
- Barnett GH, Hardy RW. Gardner tongs and cervical traction. Med Instrum 1982;16:291-2. [PubMed]
- Barsoum WK, Mayerson J, Bell GR. Cranial nerve palsy as a complication of operative traction. Spine (Phila Pa 1976) 1999;24:585-6. [Crossref] [PubMed]
- Bithal PK, Pandia MP, Chaturvedi A, et al. Lidocaine infiltration of the scalp does not completely abolish increased intraocular pressure due to skull pin insertion. J Clin Neurosci 2006;13:730-2. [Crossref] [PubMed]
- Blumberg KD, Catalano JB, Cotler JM, et al. The pullout strength of titanium alloy MRI-compatible and stainless steel MRI-incompatible Gardner-Wells tongs. Spine (Phila Pa 1976) 1993;18:1895-6. [Crossref] [PubMed]
- Celli P, Palatinsky E. Brain abscess as a complication of cranial traction. Surg Neurol 1985;23:594-6. [Crossref] [PubMed]
- Cotler JM, Herbison GJ, Nasuti JF, et al. Closed reduction of traumatic cervical spine dislocation using traction weights up to 140 pounds. Spine (Phila Pa 1976) 1993;18:386-90. [Crossref] [PubMed]
- Grant GA, Mirza SK, Chapman JR, et al. Risk of early closed reduction in cervical spine subluxation injuries. J Neurosurg 1999;90:13-8. [PubMed]
- Krag MH, Byrt W, Pope M. Pull-off strength of gardner-Wells tongs from cadaveric crania. Spine (Phila Pa 1976) 1989;14:247-50. [Crossref] [PubMed]
- Lerman JA, Dickman CA, Haynes RJ. Penetration of cranial inner table with Gardner-Wells tongs. J Spinal Disord 2001;14:211-3. [Crossref] [PubMed]
- Littleton K, Curcin A, Novak VP, et al. Insertion force measurement of cervical traction tongs: a biomechanical study. J Orthop Trauma 2000;14:505-8. [Crossref] [PubMed]
- Malomo AO, Emejulu JK, Odukogbe AA, et al. Cervical spinal cord injury in pregnancy. Conservative management of 3 consecutive cases in Ibadan, Nigeria. African Journal of Neurological Sciences 2006;25:6-12.
- Neville S, Watts C, Loos L, et al. Use of traction in cervical spine fractures during interhospital transfer by aircraft. J Spinal Disord 1990;3:67-76. [Crossref] [PubMed]
- Nimityongskul P, Bose WJ, Hurley DP Jr, et al. Superficial temporal artery laceration. A complication of skull tong traction. Orthop Rev 1992;21:761-764-5. [PubMed]
- Parada SA, Arrington ED, Kowalski KL, et al. Unilateral cervical facet dislocation in a 9-year-old boy. Orthopedics 2010;33:929. [PubMed]
- Reindl R, Ouellet J, Harvey EJ, et al. Anterior reduction for cervical spine dislocation. Spine (Phila Pa 1976) 2006;31:648-52. [Crossref] [PubMed]
- Soyer J, Iborra JP, Fargues P, et al. Brain abscess as a complication of cranial traction by Gardner-Wells tongs. Chirurgie 1999;124:432-4. [Crossref] [PubMed]
- Wang MY, Prusmack CJ, Green BA, et al. Minimally invasive lateral mass screws in the treatment of cervical facet dislocations: technical note. Neurosurgery 2003;52:444-7. [Crossref] [PubMed]



