Forestier syndrome presenting with dysphagia: case report of a rare presentation
Introduction
Diffuse idiopathic skeletal hyperostosis (DISH) is a rheumatologic disease which can cause cervical osteophytes and lead to otolaryngological symptoms such as difficulty in swallowing, difficulty in breathing and loss of weight. Primarily involved structure is the anterior longitudinal ligament, ossification and calcification of which result in osteophyte formation (1). Clinical and radiological characteristics of the disease was defined by Forestier and Rotés-Querol for the first time in 1950 (2), and the disease was named as DISH in 1975, by Resnick et al. (3).
In DISH, cervical area is less affected compared to thoracic and lumbar vertebral segments. The most commonly affected area is C4–7 (i.e., lower cervical) segments which correspond to relatively more mobile regions of cervical vertebra (4). However, Forestier syndrome is very rarely seen in upper cervical region which is relatively less mobile (5,6). Here we report a very rare case of Forestier syndrome with upper cervical involvement presenting with dysphagia as a result of osteophyte at C2–3 level. The patient underwent anterior cervical osteophyte resection with no discectomy, fusion or stabilization. Clinical and radiological characteristics of the disease and our surgical approach were discussed through the review of the current literature.
Case presentation
A 77-year-old male patient was referred to our department with the complaints of difficulty in swallowing, difficulty in breathing and severe loss of weight (10 kg in 6 months). Medical history and physical examination were unremarkable. There was no neurological involvement. Laboratory tests including HLA-B27 were within normal limits. Extensive ossification of the anterior longitudinal ligament starting from anterior C2 extending to anterior C6 vertebrae encroaching the esophagus was detected in axial and sagittal reconstruction cervical computed tomography (CT) of the patient (Figure 1A,B). Hyperostosis with osteophytic formation was especially apparent at C2–3 level. In the cervical magnetic resonance imaging (MRI) scan, which was taken to exclude other possible causes, no pathology but hyperostosis was detected at C2–6 levels (Figure 1C).
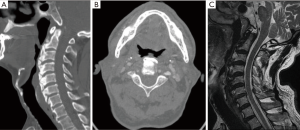
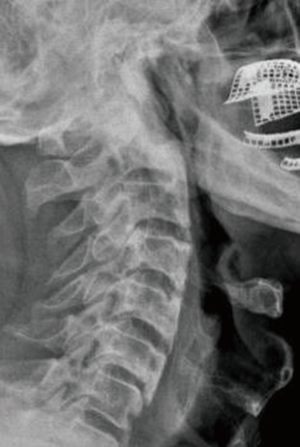
Due to severe symptoms such as difficulty in breathing, dysphagia and excessive loss of weight the patient was operated on. Cervical osteophyte resection was performed with the help of a high-speed tour (Midas Rex, Medtronic, Fort Worth, USA) between C2–6 via an anterolateral approach. Because of the advanced age, which might increase the risk of additional implant complications, and because of relatively stable cervical vertebrae, no fusion or instrumentation was added to the osteophyte resection. No preoperative or postoperative complication was encountered. Respiratory difficulty and difficulty in taking fluids resolved immediately after the surgery. Difficulty in swallowing solid foods declined but still existed in the early postoperative period. Postoperative cervical CT scan revealed that osteophytic formations compressing the esophagus had been sufficiently removed (Figure 2). The patient was discharged on the postoperative 4th day without any neurological deficit. Difficulty in swallowing solid foods gradually improved and was completely resolved at the end of the third month of operation. No evidence of recurrence was detected in lateral cervical X-ray and the patient was free of symptoms at 1-year follow-up examination (Figure 3).

Discussion
DISH is a rare pathology characterized by ossification and calcification of paravertebral ligaments and muscles (3). DISH is observed more frequently in males than females and its frequency increases with age (3,7). It has a prevalence of 8–10% over the age of 65 and, it is rarely seen under the age of 45 (3).
Etiology of the disease is not known exactly, however, it has been reported that DISH is associated with acromegaly, type II diabetes mellitus, obesity, genetic factors such as hypervitaminosis A, HLA-B27, HLA-B5, HLA-A11, ankylosing spondylitis and infectious diseases (1,5). The medical history of our case was unremarkable, no associated disease was detected and he was HLA-B27 negative.
Spine, pelvis, patella and calcaneus are the most frequently involved regions in DISH (8). Sacroiliac joint involvement is not observed in DISH (3). Throughout the spine; it is observed 97% in thoracic, 90% in lumbar, 78% in cervical vertebrae, and 70% in these three regions together (9). Anterior longitudinal ligament is the usual site of involvement in vertebral column. Due to immobility of the thoracic vertebrae, osteophytic structures extend continuously along the thoracic segments without any interruption. But in the cervical and lumbar areas, hyperostosis is rather horizontal (3). The most frequently involved region in the cervical vertebrae is the region between C4–7. On the other hand, involvement of the upper cervical vertebrae is very rare in DISH (10). In our case, the site of involvement was C2–5, which is very rarely reported in the literature. The osteophyte located anterior to vertebra corpus, at the level of C2–3, was the main cause of dysphagia.
The most frequently observed symptoms of DISH are neurovascular compression, restriction of movement, cervicalgia, stridor, hoarseness, and dysphagia (11-13). Dysphagia is observed in 0.6–1.0% of DISH cases, where cervical area is the primarily affected region (14). Dysphagia typically appears as a result of esophageal compression in lower cervical segments, most frequently at C4–5 level (10). Esophageal occlusion, recurrent laryngeal nerve damage, esophageal fibrosis, and inflammation have been considered among the reasons of dysphagia (15). In the case we are presenting, osteophytic structures were determined in anterior cervical area, between C2–5. Our case, which represents an upper cervical involvement, is a rare case containing C2–3 osteophyte leading to dysphagia.
DISH is diagnosed based on radiological examinations (12,13). There are three radiological diagnostic criteria: (I) formation of calcification and bone bridges in two adjacent vertebrae; (II) intervertebral disk height being normal or slightly reduced; (III) absence of ankylosis in the interapophysial joints (3,14). In lateral X-ray, hyperostosis is observed only on the anterior surface of the vertebra in the beginning of the disease, while in the latter stages, osteophytes are firmly adhered to the cortex, starting from anterior border to the intervertebral area (11). CT is the gold standard diagnostic tool (4). Especially sagittal, coronal and three-dimensional reconstructions of CT allow us to clearly identify the relation of osteophytes with the surrounding anatomical structures. Barium swallowing study is a useful method in determining the degree and the localization of esophageal compression (7). In our case; lateral X-ray, CT and barium swallowing studies were performed to make the diagnosis.
In symptomatic DISH cases, conservative treatment options are recommended if clinical findings are not very severe (11). Non-steroid anti-inflammatory drugs, steroids, myorelaxants, dietary changes, anti-reflux treatments are among the conservative treatment options (1,8). Surgical treatment should be considered in cases with severe symptoms such as progressive dysphagia, excessive loss of weight, difficulty in breathing and in patients who do not respond to the conservative treatment (12). In our case, surgery was indicated due to gradually progressing severe dysphagia, loss of weight and respiratory distress.
It is important to distinguish hyperostotic structures from osteoarthritic osteophytes since each has a different surgical treatment. Removal of hyperostotic structures is sufficient in surgical treatment of DISH; while additional stabilization of vertebra is required after removal of osteoarthritic osteophytes (3,9). Anterior cervical approach, posterolateral approach and transpharyngeal approaches are the surgical methods that can be preferred. Anterior cervical approach is considered safe and effective (10); however, it may lead to some complications such as recurrent laryngeal nerve injury, Horner syndrome, fistula formation and instability (1). Although posterolateral approach provides a wide surgical exposure, it has the risk of injury to internal carotid artery and sympathetic chain due to excessive retraction (14). Transpharyngeal approach is another surgical approach that can be preferred (10). The most important complication of this method is the infections that occur as a result of the contamination by the oropharyngeal flora. In our case, osteophytic structures were removed via an anterior cervical approach. It has been seen that sufficient exposure can be obtained between C2–5 with an anterior cervical approach.
The prognosis varies in the literature. Hirano et al. (9) reported 65% recurrence rate after a mean postoperative follow-up period of 4.5 years. Miyamoto et al. (15) reported seven patients with a mean postoperative follow-up period of 9 years and detected 100% recurrence of osteophytes, with a rate of approximately 1 mm/year. Recurrence was not detected during 1-year follow-up period of our case.
Conclusions
Forestier syndrome presenting with dysphagia is very rare. Surgery is indicated when the symptoms are severe and progressive. Despite the possibility of recurrence in long-term follow-up, resection of osteophytes via an anterior cervical approach is a reliable and effective surgical treatment modality in Forestier syndrome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Akhtar S, O'Flynn PE, Kelly A, et al. The management of dysphasia in skeletal hyperostosis. J Laryngol Otol 2000;114:154-7. [Crossref] [PubMed]
- Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis 1950;9:321-30. [Crossref] [PubMed]
- Resnick D, Shaul SR, Robins JM. Diffuse idiopathic skeletal hyperostosis (DISH): Forestier's disease with extraspinal manifestations. Radiology 1975;115:513-24. [Crossref] [PubMed]
- Özkırış M, Okur A, Kapusuz Z, et al. Forestier's syndrome: a rare cause of dysphagia. Kulak Burun Bogaz Ihtis Derg 2014;24:54-7. [Crossref] [PubMed]
- Mader R. Diffuse idiopathic skeletal hyperostosis: time for a change. J Rheumatol 2008;35:377-9. [PubMed]
- Solaroğlu I, Okutan O, Karakuş M, et al. Dysphagia due to diffuse idiopathic skeletal hyperostosis of the cervical spine. Turk Neurosurg 2008;18:409-11. [PubMed]
- Kiss C, O'Neill TW, Mituszova M, et al. Prevalence of diffuse idiopathic skeletal hyperostosis in Budapest, Hungary. Rheumatology (Oxford) 2002;41:1335-6. [Crossref] [PubMed]
- Andersen PM, Fagerlund M. Vertebrogenic dysphagia and gait disturbance mimicking motor neuron disease. J Neurol Neurosurg Psychiatry 2000;69:560-1. [Crossref] [PubMed]
- Hirano H, Suzuki H, Sakakibara T, et al. Dysphagia due to hypertrophic cervical osteophytes. Clin Orthop Relat Res 1982.168-72. [PubMed]
- Carrau RL, Cintron FR, Astor F. Transcervical approaches to the prevertebral space. Arch Otolaryngol Head Neck Surg 1990;116:1070-3. [Crossref] [PubMed]
- Ebo D, Goethals L, Bracke P, et al. Dysphagia in a patient with giant osteophytes: case presentation and review of the literature. Clin Rheumatol 2000;19:70-2. [PubMed]
- Hwang JS, Chough CK, Joo WI. Giant anterior cervical osteophyte leading to Dysphagia. Korean J Spine 2013;10:200-2. [Crossref] [PubMed]
- Kmucha ST, Cravens RB Jr. DISH syndrome and its role in dysphagia. Otolaryngol Head Neck Surg 1994;110:431-6. [Crossref] [PubMed]
- McCafferty RR, Harrison MJ, Tamas LB, et al. Ossification of the anterior longitudinal ligament and Forestier's disease: an analysis of seven cases. J Neurosurg 1995;83:13-7. [Crossref] [PubMed]
- Miyamoto K, Sugiyama S, Hosoe H, et al. Postsurgical recurrence of osteophytes causing dysphagia in patients with diffuse idiopathic skeletal hyperostosis. Eur Spine J 2009;18:1652-8. [Crossref] [PubMed]


