Functional outcomes of laminectomy and laminotomy for the surgical management lumbar spine stenosis
Introduction
The gradual, degenerative process of lumbar spinal stenosis (LSS) is highly prevalent in the increasingly aging population. LSS results in circumferential compression of the dural sac and spinal nerves producing neurogenic claudication, back and leg pain with associated disability. Conventionally, surgical management aims to decompress and is reserved for selected patients with persistent, severe symptoms (1). Optimal management of LSS is still under debate, with the controversies and diversity highlighted by an interactive survey at the Eurospine Congress 2014 (2). Traditionally, open laminectomy has been effectively employed, although increasingly other strategies are being utilised, such as laminotomy. Both approaches aim to improve radicular leg pain, subsequently improving functional ability and as noted by a recent study has the potential to significantly improve back pain and quality of life (3).
The Spine Tango Registry [2014] report detailing patient outcome following decompression surgery has identified that general complications were higher for laminectomy when compared to laminotomy. Laminectomy for LSS in comparison to newer and less invasive surgeries, such as laminotomy, is associated with greater blood loss, postoperative wound pain, prolonged hospital-stay, paraspinal muscle devascularization and risk of iatrogenic segmental spinal instability requiring instrumented fusion or stabilization (4-6).
Primum non nocere ‘above all, do no harm’ is a fundamental of medical practice. When applied to surgery, adherence to this maxim, requires an assessment of the relative risks and benefits of any proposed surgical procedure. Laminectomy for LSS is considered the standard surgical option to which other techniques are compared. Ascertaining superiority of a decompression technique necessitates establishing if any differences exist in the complication rates and the functional and symptomatic outcomes. This study aims to to establish if any differences exist in the clinical outcomes of laminectomy versus laminotomy surgery at our institute, including a consideration of the impact on both leg and lower back pain (LBP) symptoms as well as disability.
Methods
Patient selection
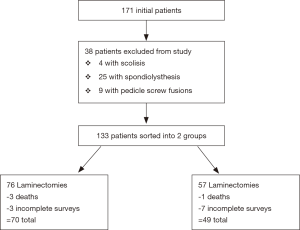
Over a period of 6 years (2006 to 2012), all patients [171] with confirmed LSS (both lateral and/or central) on MR imaging who had failed conservative management, were considered for operative management. Patients with spondylolisthesis, or scoliosis and those who had undergone fusion, discectomies or further revisions were excluded from the study. Following exclusions, 133 patients were enrolled; 76 underwent a laminectomy without fusion and 57 underwent either a bilateral or unilateral laminotomy. Inpatient exclusion and inclusion criteria are presented in a consort diagram, see Figure 1.
Data collection
This study was a retrospective review of prospectively collected data. All patients provided informed consent and completed an Oswestry Disability Index (ODI) and visual analogue scale (VAS) pre-operatively and in follow-up clinics at 6 weeks and 1 year. Prior to attendance questionnaires were distributed by mail and any issues resolved in the clinic. All questionnaires and forms were collected and checked for completeness by a lead researcher. For outstanding issues, patients were contacted directly. Patients who had not attended clinic were contacted with a letter and return form.
Operative procedure
The same surgeon performed all surgeries according to normal protocol. Laminectomy was performed in patients with severe stenosis in the mid zone of foramen and laminotomy performed for predominantly central and foraminal entry zone stenosis
Laminotomy
Laminotomy was performed using a minimally invasive approach. With or without magnification, part of the lamina and ligamentum flavum was excised as necessary to visualise the stenotic area and safely undercut the medial facet as necessary. Patients mobilised the morning after surgery. Patient controlled analgesia was routinely offered as patient seemed to experience more immediate post-operative pain.
Laminectomy
The entire lamina and spinous process was removed to visualise the dura. Care is made to preserve the facet joints, removing only the osteophytes medially. Patients mobilised the morning after surgery. Patient controlled analgesia was not routine but prescribed to patients requiring it. Each patient was given a soft lumbar support for 6 weeks, to discourage flexion.
Outcome measures
The primary outcome investigated back and leg pain for both the laminectomy and laminotomy groups at the given time intervals. Establishing if any differences exist between patients groups subdivided by LBP severity (defined by pre-operative VAS scores of less than 5 or 5 or more) was performed.
Secondary outcomes detailed the change in each patient’s disability and complications in the two surgical procedures. Further subgroup analysis of bilateral laminotomy patients was performed.
Statistical analysis
Four patients at 6 weeks and a further six patients at 1 year did not respond. These patients were excluded from the analysis as were four patients who died during the study time period. One patient died immediately post-operatively (an autopsy report failed to identify a cause of death) and the three other deaths were unrelated to the spinal surgery. Statistical analysis was carried by an independent statistician. Pre- and post-operative scores in the laminotomy and laminectomy groups were compared using the unpaired two-sample t-test, with a P value of <0.05 considered to be significant.
Results
After exclusions, see Figure 1, 119 patients were analysed, 55% were females (n=65) and 45% males (n=54) with a mean age of 68.7 years. Of these patients, 98 had central and 21 had lateral spinal stenosis. Forty-nine patients underwent laminotomy with 59% having bilateral laminotomy (n=29) and the rest unilateral laminotomy (n=20). In the laminectomy group, 1 person underwent a left sided hemilaminectomy for left sided lateral recess stenosis. The most frequent level of pathology was L4/5.
Considering all surgeries, a statistically significant reduction in VAS back between pre-op and 6 weeks was seen (4.99 to 3.00, P<0.0001), see Table 1. Overall, significant reductions in LBP was sustained to 1 year (P<0.001), average LBP increased by 0.33 units between week 6 and 1 year (3.00 to 3.33). This trend was mirrored in both surgery groups with minimal differences between laminectomy and laminotomy. That is statistically significant reductions in VAS back scores were seen at 6 weeks and 1 year, with the greater improvement seen at 6 weeks. Laminectomy vs. bilateral laminotomy demonstrated no significant differences in the reduction of LBP at 6 weeks (P=0.22) or 1 year (P=0.45).
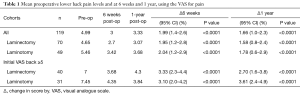
Full table
A different trend is noted when a subdivision of patients with preoperative VAS back scores of 5 or above were analysed. Statistically similar reductions in LBP are seen after 6 weeks between laminectomy vs. laminotomy (an unpaired two-sample t-test gave P<0.0001). However, laminectomy patients experienced an increase in LBP of 0.63 units between 6 weeks and 1 year (3.68 to 4.30), whilst laminotomy patient’s LBP further decreased by 0.51 units (4.35 to 3.84). An unpaired two-sample t-test showed a P value of 0.063, indicating non-statistical significance at the 5% level.
Both laminectomy and laminotomy groups had statistically significant improvements in VAS leg pain scores after 6 weeks (mean reductions of 4.36 and 4.32, both P<0.0001), as seen in Table 2. A greater improvement in leg pain at 1 year was seen in laminectomy vs. laminotomy patients (3.64 vs. 2.90, P=0.24). Laminectomy vs. bilateral laminotomy demonstrated no significant difference in the reduction of leg pain at 6 weeks (P=0.37) or 1 year (P=0.43).
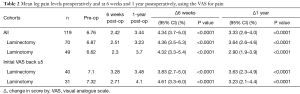
Full table
Establishing if any differences exist for leg pain outcomes was performed for the 71 patients with VAS back greater than 5. Similar improvements in leg pain were observed after 6 weeks for each group. However, a greater increase in VAS leg pain scores were seen for laminotomy vs. laminectomy between 6 weeks and 1 year, without reaching statistical significance (1.39 vs. 0.20, P=0.11).
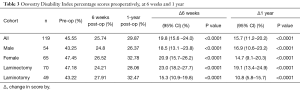
The average pre-operative ODI score for all patients was 45.55%, reducing to 25.74% at 6 weeks and was 29.87% after 1 year, see Table 3. These reductions in disability are statistically significant at a 5% level, with the final ODI scores indicative of mild disability. The degree of disability was found to be independent of gender. Although a greater improvement in ODI was seen for patients at 1 year for laminectomy vs. laminotomy (19.1% vs. 10.8%), such differences were not found to be statistically significant. Similarly, laminectomy vs. bilateral laminotomy demonstrated no significant difference in the reduction of ODI scores at 6 weeks (P=0.25) or 1 year (P=0.13).
Full table
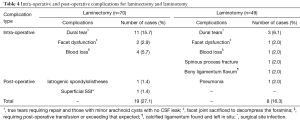
Twice as many patients had intraoperative complications in the laminectomy group compared with the laminotomy group, 24.3% (n=17) vs. 14.3% (n=7); with dural tears being the most frequent complication, 15.7% (n=11) vs. 6.1% (n=3). Comparable post-operative complications rates were seen for laminectomy and laminotomy, viz. 2.9% and 2.0% respectively, as seen in Table 4.
Full table
Discussion
Laminectomy decompression although effective is associated with significant blood loss, postoperative wound pain, prolonged hospital-stay, extensive soft tissue dissection, paraspinal muscles devascularization and the risk of iatrogenic segmental spinal instability requiring instrumented fusion or stabilization (4-6). As a result, various less invasive adaptations have been described, with the aim to preserve the posterior elements of the spine and soft tissue stripping and hence reduce the risk of iatrogenic segmental instability whilst maintaining favourable outcomes. These adaptations include techniques such as spinous process splitting laminoplasty (7) laminectomy preserving spinous process, hemilaminectomy, laminotomy, and microsurgical and endoscopic undercutting laminotomies (8,9). Furthermore, the approach of whether the surgery is direct, lateral, unilateral (‘cross-over’) or slalom has been scrutinised to try and reduce the adverse effects of surgery (10-12).
The Spine Tango Registry [2014] report detailing patient outcome following decompression surgery has identified that general complications were higher for laminectomy when compared to laminotomy. In particular an increased risk of requiring fusion or stabilisation following a laminectomy was noted. Furthermore, a significant increase in surgical and general complications is seen when laminectomy with instrumented fusion was compared with laminotomy (8,9). Our study demonstrated more complications in laminectomy than laminotomy which is in keeping with the Spine Tango Registry report (8,9). Our results demonstrate in both groups ODI scores improved by an average of 15% (pre-operatively to a year) with minimal differences, suggesting each operation had a similar effect upon disability.
Varying degrees of LBP and leg pain symptoms are seen in LSS patients being considered for decompression surgery. Currently, little evidence exists that advocates employing one surgical approach over another to target those with greater back than leg pain and vice versa. There was a reduction in LBP and leg pain with both operations which is consistent with the findings of Jones et al. (3) Greater reductions leg pain than back pain were seen, 3.33 (2.6–4.0) vs. 1.66 (1.0–2.3) at 1 year. Although differences in scores were noted between the surgeries, none were statistically significant. Whilst not statistically significant (P=0.24), larger reductions in leg pain were demonstrated in the laminectomy compared with laminotomy patients at 1 year. Less symptomatic benefit may be seen in laminotomy patient’s leg pain as, while laminotomy is a less invasive procedure, it has an increased likelihood of disease recurrence and need for revision. The Spine Tango Registry data supported this conclusion; showing worsening leg pain in patients who underwent laminotomy and that revision was more likely (7,8). Laminotomy, due to its minimal invasiveness has a lower complication rate than laminectomy but it may come at the cost of needing revision.
In our study, patients with pre-operative VAS back scores ≥5, showed similar improvement at 6 weeks in both the laminectomy and laminotomy groups. However, at 1 year, LBP increased in laminectomy patients whilst it continued to decrease in laminotomy patients. Although not statistically significant (P=0.063) and further data is required; equivalence between these groups cannot be assumed.
This study had good external validity; it was a prospective study of consecutive clinic patients, followed over a 12-month period. It is reproducible and standard operation techniques and procedures were followed. The allocation of surgery by stenosis zone represents common practice. There were several limitations of this study including; patient selection bias as a result of a single hospital and surgeon cohort, a relatively small number of patients, high attrition rates, and a short term follow up. In addition, whilst ODI addresses walking distance (item four), specific outcomes measures for neurogenic claudication were not collected.
Conclusions
This descriptive study demonstrated functional outcomes for laminectomy and laminotomy procedures were comparable in our institute. Both surgeries were equally effective in improving leg and LBP, and disability. Although not statistically significant, a finding that merits further study, was that differences in LBP improvement were seen in patients with greater LBP pre-operatively. Laminectomy is known to have higher general complication rates compared to alternative decompression methods. On the basis of functional outcomes laminectomy remains a feasible approach in the treatment of LSS. The authors publish these non-differentiating findings in order to add to collective data.
Acknowledgements
We would like to thank Mr. Michael Bodnarchuk of Imperial College London for his help and support with the statistical analysis and seeing this paper through.
Footnote
Conflicts of Interest: The authors have no conflict of interest to declare.
Ethical statement: This study does not require ethical committee approval according to the NHS National research ethics service guide because it is an observational study, which does not involve a medical device evaluation or exposure to ionising radiation. Furthermore, the surgical procedures performed is well recognised as the treatment of the pathology. All patients provided informed consent.
References
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ 2016;4;352:h6234.
- Eurospine. 'App Voting system', an interactive presentation at the Eurospine congress. 2014 Oct 1-3; Lyon: France.
- Jones AD, Wafai AM, Easterbrook AL. Improvement in low back pain following spinal decompression: observational study of 119 patients. Eur Spine J 2014;23:135-41. [Crossref] [PubMed]
- MacNalty A. Sir Victor Horsley: his life and work. Br Med J 1957;1:910-6. [Crossref] [PubMed]
- Mahadewa TG, Sri Maliawan S, Sudewi R, et al. A comparative study of bilateral laminotomy and laminectomy with fusion for lumbar stenosis. Neurol Asia 2010;15:153-8.
- Feffer HL, Wiesel SW, Cuckler JM, et al. Degenerative spondylolisthesis. To fuse or not to fuse. Spine (Phila Pa 1976) 1985;10:287-9. [Crossref] [PubMed]
- Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 1991;73:802-8. [Crossref] [PubMed]
- Shetty AP, Kanna RM, Avadhani A, et al. Lumbar spinous process split decompression. Eur Spine J 2010;19:357-8. [Crossref] [PubMed]
- Munting E, Röder C, Sobottke R, et al. Patient outcomes after laminotomy, hemilaminectomy, laminectomy and laminectomy with instrumented fusion for spinal canal stenosis: a propensity score-based study from the Spine Tango registry. Eur Spine J 2015;24:358-68. [Crossref] [PubMed]
- Munting E, Roder C, Sobottke R, et al. Patient outcomes after laminotomy, hemilaminectomy, laminectomy and laminectomy with instrumented fusion for spinal canal stenosis or degenerative spondylolisthesis. Eur Spine J 2013;22:S653-84. [PubMed]
- Mayer HM, Heider F. Selektive, mikrochirurgische „Cross-over“-Dekompression mehrsegmentaler lumbaler Spinalstenosen. Oper Orthop Traumatol 2013;25:47-62. [Crossref] [PubMed]
- Matsudaira K, Yamazaki T, Seichi A, et al. Spinal stenosis in grade I degenerative lumbar spondylolisthesis: a comparative study of outcomes following laminoplasty and laminectomy with instrumented spinal fusion. J Orthop Sci 2005;10:270-6. [Crossref] [PubMed]