Spondylolisthesis with spondylolysis in a 17-month-old: a case report
Introduction
Spondylolysis is frequently seen in adolescents, typically at the L5 vertebral level. It is especially seen in those who participate in certain athletics, including gymnastics, football, and rowing (1). While considering that there may be congenital predisposition for spondylolysis, it has long been suggested that the defect results from a fatigue or stress fracture of the pars interarticularis (2). Spondylolisthesis may result from a bilateral spondylolytic defect and is frequently asymptomatic (3). There is a paucity of literature on infant and toddler spondylolysis, as the focus is primarily on school-aged children, typically those over ten years of age. This case report presents an incidentally discovered L5 spondylolysis with spondylolisthesis in a 17-month-old female. The patient’s guardian provided written informed consent for publication of this article.
Case presentation
The patient is a 17-month-old female who presented to the emergency department with multiple facial abrasions and bruises. The reported mechanism of injury was that she was struck by her 4-year-old sister. She was admitted to the hospital for a non-accidental trauma work-up. With the exception of the facial abrasions and bruises, her physical examination was otherwise within normal limits, with no neurological deficits noted. Her past medical history included a hospitalization four months prior for a prior non-accidental trauma work-up after she was discovered to have a distal radius buckle fracture. The mechanism of injury was reportedly a thirty foot fall from a window. At that time no skeletal survey was obtained for comparison, and the buckle fracture healed uneventfully with cast immobilization. Otherwise, her medical history, birth history, and social history are unremarkable.
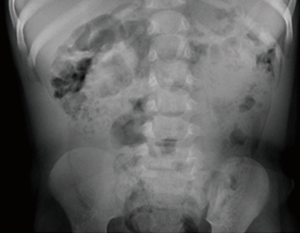
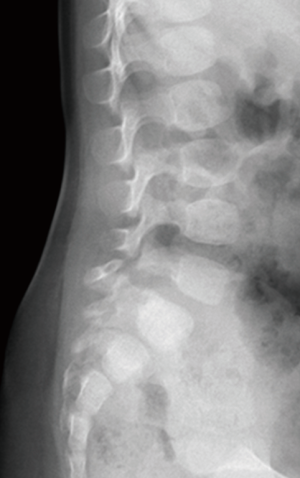
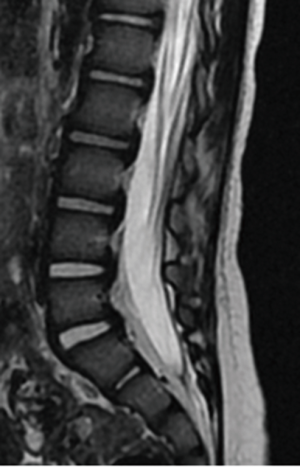
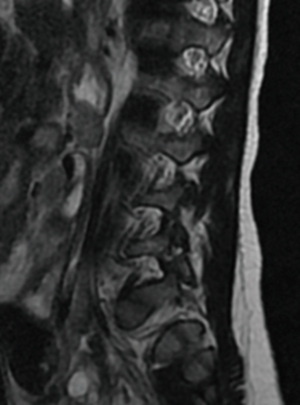
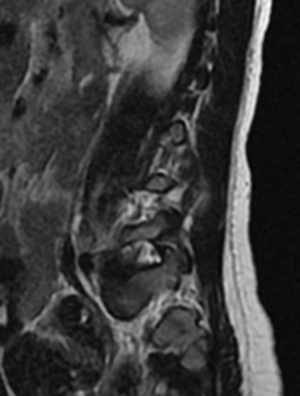
A routine non-accidental trauma work-up was performed, including a skeletal survey. Review of the skeletal survey demonstrated L5 bilateral pars defect with Myerding grade 2 spondylolisthesis (Figures 1-3). The rest of the non-accidental trauma work-up was negative. An MRI of the lumbar spine was performed, again demonstrating the L5 bilateral pars defect with position dependent reduction of the spondylolisthesis. There was no surrounding bony edema, and no other pathology was noted. There was no indication for orthopedic intervention, and she was discharged from the hospital through the Department of Social Services.
The patient was seen back in the orthopedic office three months later, which is her latest follow-up. Dynamic plain films of the lumbar spine were unchanged from previous imaging, without evidence of instability or slip progression (Figures 4,5).
Discussion
Low back pain is infrequently seen in the pediatric orthopedic population, but when it is encountered, spondylolysis and spondylolisthesis should be high on the differential diagnosis, along with Scheuermann disease (1). These conditions, however, are typically asymptomatic in young children and can be discovered incidentally, as demonstrated by Fredrickson et al. (4). Spondylolysis as well as spondylolisthesis have rarely been reported in the literature for children under the age of 5. It is frequently taught that these conditions do not occur prior to a child weight-bearing in the erect posture (5). Interestingly, there is a case report from 1955 of spondylolysis with spondylolisthesis diagnosed in a 4-month-old who presented with a kyphotic deformity (6).
Spondylolisthesis is most commonly classified by the etiology as per the Wiltse-Newman system: dysplastic, isthmic, degenerative, traumatic, and neoplastic. It can further be graded by listhetic severity by the Myerding classification: <25%, 25–50%, 50–75%, 75–100%, and spondyloptosis.
The pathogenesis of spondylolysis, while disputed, is thought to be multifactorial. It has been postulated, that along with family history, the vertebra may be congenitally weak due to genetic factors or have a dysplastic pars interarticularis; and when subjected to repetitive microtrauma, especially lumbar hyperextension, a stress fracture may result (7). This is further supported by the fact that approximately 90% of cases of spondylolysis are at the L5 level, where the vertebrae is under tremendous static and dynamic stresses (8). As a result of the abnormal posterior elements and possible resultant spinal instability or hypermobility from spondylolysis, spondylolisthesis may develop. It has been demonstrated that slip progression is most likely to occur in the immature spine, and notably slows with aging (4).
The treatment for spondylolysis and spondylolisthesis are symptom based. Asymptomatic patients with low grade slips are typically observed. If they develop symptoms, therapy may be prescribed. Bracing is reserved for those that fail therapy, or have acute spondylolysis (i.e., non-sclerotic bone margin at site of defect). Surgical management, whether pars interarticularis repair or segment fusion, is reserved for low grade slips that fail non-operative modalities; those with neurologic deficits or documented slip progression; and those with high grade slips (typically >50% or grade 3).
Conclusions
This case is quite unique in that the patient was 17 months of age, with very few reports in the literature of children less than 5 years of age with spondylolysis. The pathology was diagnosed incidentally, but there is suspicion that the spondylolysis may have been associated with the trauma that occurred 4 months prior to presentation (thirty foot fall from a window). Given the patient’s normal neurological examination and lack of symptoms, close observation with repeat imaging was performed. Further progression of her slip should warrant consideration for further treatment, whether it be cast immobilization or surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: WF Lavelle has grants in which monies are paid to the institution with the following companies: DePuy, Medtronic, IntegraLife, Sigmus, Inc., Spinal Kinetics, Inc., K2M, Inc., Providence Technologies, Stryker Spine and Vertebral Technologies, Inc. The other authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Bhatia NN, Chow G, Timon SJ, et al. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop 2008;28:230-3. [Crossref] [PubMed]
- Wiltse LL, Widell EH Jr, Jackson DW. Fatigue fracture: the basic lesion is inthmic spondylolisthesis. J Bone Joint Surg Am 1975;57:17-22. [Crossref] [PubMed]
- Sairyo K, Katoh S, Ikata T, et al. Development of spondylolytic olisthesis in adolescents. Spine J 2001;1:171-5. [Crossref] [PubMed]
- Fredrickson BE, Baker D, McHolick WJ, et al. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 1984;66:699-707. [Crossref] [PubMed]
- Garg S, Erickson M. Spondylolysis and isthmic spondylolisthesis. In: Patel VV, Patel A, Harrop JS, et al. editors. Spine Surgery Basics. New Delhi: Springer-Verlag Berlin Heidelberg, 2014:311-24.
- Borkow SE, Kleiger B. Spondylolisthesis in the newborn. A case report. Clin Orthop Relat Res 1971.73-6. [Crossref] [PubMed]
- Sakai T, Goda Y, Tezuka F, et al. Characteristics of lumbar spondylolysis in elementary school age children. Eur Spine J 2016;25:602-6. [Crossref] [PubMed]
- Grogan JP, Hemminghytt S, Williams AL, et al. Spondylolysis studied with computed tomography. Radiology 1982;145:737-42. [Crossref] [PubMed]