Thoracic juxtafacet cyst (JFC): a cause of spinal myelopathy
Introduction
Juxtafacet cysts (JFCs) are common in mobile segments of the spine as part of the degenerative process. Expansion from the degenerated facet joint can be intraspinal or extraspinal. Intraspinal cysts can compress the nerve roots passing adjacent to the facet joint and cause compression and radicular symptoms. Diagnosis is typically made with confidence by appearance on MR scan. Contrasted studies and CT can be helpful as well (1). JFC are most commonly encountered in the lumbar spine (2,3). They are less commonly encountered in the thoracic spine, perhaps due to the decreased mobility of this region. There is limited literature on symptomatic thoracic JFC (4,5). We present an interesting case report of a patient with symptoms of myelopathy due to the location of the cyst in a less mobile thoracic segment of the spine that was effectively treated by a surgical excision of the lesion.
Case presentation
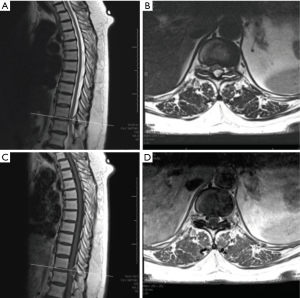
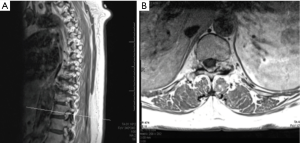
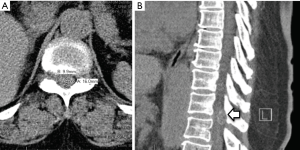
A 67-year-old right hand dominant woman was referred by her neurologist with a complaints of lower extremity symptoms. She had chronic lower back pain and pain in her thighs but was able to walk several blocks and maintain her overall function. About 3 weeks prior to presentation she noticed sudden onset of numbness in bilateral lower extremities, left more than the right, associated with weakness and difficulty walking. The symptoms started suddenly on awakening one morning but did not progress. She complained of difficulty walking and maintaining balance, requiring a cane for support. Her symptoms were worse with standing; and sitting was associated with mild back pain. She was most comfortable lying down. She denied upper extremity symptoms, although she complained of some urinary dysfunction. She denied fever, recent travel, accident or injury or change in activity at the time of the onset. Her history included arthritis, treated breast cancer, hypothyroidism, hyperlipidemia, and varicose veins. Her neurological exam was significant for loss of touch and proprioception in a stocking distribution in her bilateral lower extremities, worse on the left. She was hyperreflexic in her left lower extremity without ankle clonus. She had unsteady tandem gait and positive Romberg sign. Based on her history and exam, MR scans of the thoracic and lumbar spine without contrast were performed. These revealed an extradural, well-delineated lesion along the dorsal aspect of the spinal canal at the T11–12 level along the medial aspect of the left T11–12 facet joint. The ligamentum flavum was disrupted along the medial aspect of the facet and left dorsal lateral aspect of the lesion. The central component of the lesion was T1 hypointense and T2/STIR hyperintense (Figure 1A and B). A day later, an MRI scan with contrast was performed; T1 post-contrast images revealed a left T11–12 facet cyst with hypointense center with a peripheral ring enhancement pattern (Figure 1C and D). The lesion extended into the left T11–12 neural foramina (Figure 2A and B). It measured 16x10mm causing canal stenosis and spinal cord compression. Additionally, a CT scan of the thoracic and lumbar spine was performed showing mild scoliosis, multilevel spondylosis, and marked degenerative facet changes at T11–12 with a minimal anterolisthesis of T11 over T12. It showed minimal peripheral calcification of the cyst (Figure 3A and B).
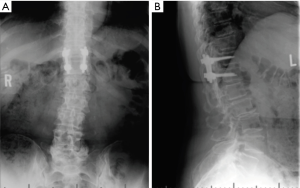
Based on her myelopathy and thoracic spinal cord compression we recommended laminectomy with resection of the lesion. Given the degenerative nature of disease, fluid in the facet joints, and need for wide decompression, we recommended fusion to minimize the risk of recurrence. General anesthesia was administered, SSEP and MEP leads placed and she was positioned prone on the Jackson table. A standard midline approach was undertaken. T11–T12 laminectomy was performed. The dorsal, left-sided adherent cystic structure was encountered and using microsurgical techniques the cyst was progressively dissected free of the dura. The cyst was completely removed and the dura remained intact. The cyst was sent to pathology. We then performed a posterior instrumented fusion with pedicle screws at T11 and T12 and arthrodesis with local morselized auto-graft. Neuromonitoring remained stable throughout the procedure. Postoperatively, the patient noticed immediate improvement with some residual numbness in the medial aspect of her left leg and the sole of the foot. She was discharged postoperative day 3 with residual decreased light touch, 2-point discrimination, vibration, and proprioception in left lower extremity. Her motor strength was 4/5 in iliopsoas, quadriceps, and 4+/5 in extensor hallucis longus, and tibialis anterior muscles. She was prescribed narcotics for symptomatic pain control with Gabapentin to manage her radicular symptoms. At one month follow up visit she reiterated partial improvement in her numbness and balance, and symptoms continued to improve but did not resolve completely by her three month documented visit. Her X-rays at 3 months show a well-aligned spinal construct (Figure 4A and B). At six-month follow-up all pre-operative myelopathic symptoms resolved with some lower back pain most likely relating to her underlying lumbar spondylosis and spondylolisthesis.
Discussion
Intraspinal facet synovial cysts, better described by the term JFCs, were first described in 1974 by Kao et al. through a histopathological diagnosis after a successful excision in the cervical spine (6). JFCs are common in degenerative facet joints where the likely pathology is the result of herniation of the synovial membrane through a defect in the joint capsule. One proposed theory is an initial loss of disc height leads to increased facet joint capsule pressures in lateral bending and axial rotation resulting in segmental instability (i.e., spondylolisthesis) finally culminating into a JFC (7). Proposed etiologies include spondylosis, spondylolisthesis, and trauma. During degeneration, there is an increase in the production of hyaluronic acid along with proliferation of mesenchymal cells which contributes to the formation of these cysts. The molecular cascade starts with an acute flare of the inflammatory process under the mechanical load that leads to the induction and release of chemokines [interleukins-1 and 6, platelet-derived growth factor (PDGF), basic fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), and substance P] resulting in neovascularization, exudation of fluid, synovial membrane hyperplasia, protrusion through the anatomical defect, and finally formation of the JFC (4,8). In some cases, after reduction of mechanical load and resolution of the inflammatory process, spontaneous reduction in size of the JFC has been observed (4,9).
The highest incidence of JFC is in the lumbar spine where most JFC are observed at the L4/5 level. This may be due to facet orientation and articulation allowing the greatest amount of AP translation and having the most segmental motion within the lumbar spine. This is followed by cervical and less frequently in the thoracic segment of the spine (10). Our literature review revealed a few cases in the thoracic spine. In 2004, a case series of 9 cases affecting the thoracic spine out of 16,000 (0.06% of the total) between 1987–2004 was published by Cohen-Gadol et al. Definitive treatment was a decompressive procedure (11). The likely cause in the thoracolumbar (T10–L1) segment of spine was postulated to be a transitional zone between a relatively immobile thoracic spine and highly mobile lumbar spine. Therefore, most of the documented thoracic cysts have been observed in this transitional zone. All cases have been described in patients more than 70 years of age apart from one case of 24 years described in 2000 by Lynn et al., (12).
Clinical presentation of JFC ranges from symptoms and signs of isolated radiculopathy due to an encroachment of the lateral recess or foramen, to neurogenic claudication, resulting from spinal canal stenosis, and caudal equina compression (13,14). Rarely, a large JFC can cause contralateral symptoms (15). At times, symptoms wax and wane depending on the size of cyst and change in overall size based on the mechanical load. JFC can also cause nocturnal pain and pain with recumbency, which is thought to be caused by the stretching of spinal nerve root.
MR is the imaging modality of choice. A JFC usually appears as a well-demarcated epidural mass with iso-intense or hyper-intense signal on T1- and T2-weighted images. The slight hyper-intensity seen could be due to small amounts of paramagnetic hemorrhagic breakdown products in the cyst fluid (16,17). Occasionally, JFC can appear hypo-intense on both T1- and T2-weighted images due to calcification. At times, MR scan may show signal void due to vacuum phenomenon; a CT scan is helpful to delineate the intracystic air (1). Contrast imaging with the gadolinium may be helpful to confirm diagnosis or identify other etiologies such as tumor or abscess (13). Typically, there is a small communication between actual cyst wall and the facet joint which is hard to delineate even on MR imaging (16). This communication may explain the dynamic nature of these lesions with expansion and decompression of the cyst due to postural changes and the mechanical stresses of the spine (10).
Treatment of JFC depends on the degree of symptoms, location, and the size of the cyst. It ranges from several non-operative treatments to more aggressive surgical excision. Non-operative treatments may be indicated for smaller cysts with controlled or improving symptoms. There are a few reports of spontaneous remission of the radicular symptoms presumably due to spontaneous cyst wall collapse or resolution of the inflammation. Epidural steroid injections can be used to reduce the inflammation and provide temporary relief (18-20). Alternatively, CT-guided aspiration is also commonly employed in the lumbar spine for cysts with only radicular pain symptoms. However, JFC in the thoracic spine is a different entity given the narrow caliber of the canal and presence of the spinal cord and concern for myelopathy. In the setting of cord compression and myelopathy, surgical decompression is recommended (21). Due to paucity on of data on treatment of JFC, the optimal surgical procedure is still controversial. Historically, an open laminectomy with medial facetectomy followed by the excision of the cyst is a commonly adopted procedure. As far as the transitional segments are concerned, decompression alone can cause iatrogenic instability. The symptoms, signs, location size of the cyst, and the presence of segmental instability are important factors considered. Patients with bilateral symptoms or central canal stenosis with segmental instability or at the transitional segment of the spine will likely benefit from decompression and fusion (21). When comparing decompression versus decompression with fusion, Bydon et al. performed a systematic review of 82 studies of 966 patients with JFC in which 84% of patients underwent decompression without fusion and the remaining 16% of patients underwent decompression with fusion. More than 91% of patients in both cohorts documented symptoms relief of back and leg pain. Interestingly, recurrence of back and leg pain was 21.9% and 12.7%, respectively, with 60 reoperations (6.2%) due to instability and back pain; 1.8% cyst recurrence in the decompression cohort and no recurrence was observed in the decompression and fusion cohort (22). In a retrospective study of 167 patients by Xu et al. the outcome from decompression with or without fusion was studied. A statistically significant increased rate of cyst recurrence was observed in the decompression only cohort when compared to the instrumented fusion cohort (3 of 39 patients versus 0 of 56 patients, respectively) (23).
The surgeon may decide to perform an instrumented fusion in addition to the decompression based on assessment of instability, degree of degeneration of the segment, and associated axial pain. This increased complexity and scope of surgery may be offset by decreased recurrence rate and need for revision surgery. Because over 90% of patients report resolution of back pain or radicular symptoms with 2% cyst recurrence rate with only decompression; augmenting with instrumentation and fusion appears to be a convincing part of the procedure in increasing the overall outcome. Therefore, surgical decompression, medial facetectomy, and cyst excision along with instrumented fusion is currently a widely accepted procedure.
Conclusions
JFC is an uncommon cause of the myelopathy in the thoracic spine but imaging with contrasted MR and CT scan should offer a good indication pre-operatively of the likely pathology and guide treatment. Surgical resection with consideration for fusion is the definitive treatment modality with potential for good neurologic and functional recovery when identified and treated expeditiously.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Apostolaki E, Davies AM, Evans N, et al. MR imaging of lumbar facet joint synovial cysts. Eur Radiol 2000;10:615-23. [Crossref] [PubMed]
- Tai PA, Li TC. Lumbar Intradural Ganglion Cyst. World Neurosurg. 2016;88:691.e1-4. [Crossref] [PubMed]
- Kouyialis AT, Boviatsis EJ, Korfias S, et al. Lumbar synovial cyst as a cause of low back pain and acute radiculopathy: a case report. South Med J 2005;98:223-5. [Crossref] [PubMed]
- Dahuja A, Dahuja G, Kaur R. Rare Thoracolumbar Facet Synovial Cyst Presenting as Paraparesis. Korean J Spine 2015;12:193-5. [Crossref] [PubMed]
- Daentzer D, Stüder D. Thoracic juxtafacet cyst (JFC) as a rare cause of myelopathy--an additional reference to support the instability theory. Joint Bone Spine 2010;77:178-80. [Crossref] [PubMed]
- Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg 1974;41:372-6. [Crossref] [PubMed]
- Park WM, Kim K, Kim YH. Effects of degenerated intervertebral discs on intersegmental rotations, intradiscal pressures, and facet joint forces of the whole lumbar spine. Comput Biol Med 2013;43:1234-40. [Crossref] [PubMed]
- Oliveira HA, Jesus AC, Prado RC, et al. Synovial cyst of the thoracic spine: case report. Arq Neuropsiquiatr 2007;65:838-40. [Crossref] [PubMed]
- Colen CB, Rengachary S. Spontaneous resolution of cervical synovial cyst. Case illustration. J Neurosurg Spine 2006;4:186. [Crossref] [PubMed]
- Bozzao A, Floris R, Fraioli C, et al. "Relapsing-remitting" bilateral synovial cysts of the lumbar spine: a case report. Neuroradiology 2001;43:1076-8. [Crossref] [PubMed]
- Cohen-Gadol AA, White JB, Lynch JJ, et al. Synovial cysts of the thoracic spine. J Neurosurg Spine 2004;1:52-7. [Crossref] [PubMed]
- Lynn B, Watkins RG, Watkins RG IV, et al. Acute traumatic myelopathy secondary to a thoracic cyst in a professional football player. Spine (Phila Pa 1976) 2000;25:1593-5. [Crossref] [PubMed]
- Liu SS, Williams KD, Drayer BP, et al. Synovial cysts of the lumbosacral spine: diagnosis by MR imaging. AJR Am J Roentgenol 1990;154:163-6. [Crossref] [PubMed]
- Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg 1999;91:193-9. [PubMed]
- Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg 2000;93:53-7. [PubMed]
- Tillich M, Trummer M, Lindbichler F, et al. Symptomatic intraspinal synovial cysts of the lumbar spine: correlation of MR and surgical findings. Neuroradiology 2001;43:1070-5. [Crossref] [PubMed]
- Jackson DE, Atlas SW, Mani JR, et al. Intraspinal synovial cysts: MR imaging. Radiology 1989;170:527-30. [Crossref] [PubMed]
- Jackson DE Jr, Atlas SW, Mani JR, et al. Intraspinal synovial cysts: MR imaging. Radiology 1989;170:527-30. [Crossref] [PubMed]
- Hagen T, Daschner H, Lensch T. Juxta-facet cysts: magnetic resonance tomography diagnosis. Radiologe 2001;41:1056-62. [Crossref] [PubMed]
- Bjorkengren AG, Kurz LT, Resnick D, et al. Symptomatic intraspinal synovial cysts: opacification and treatment by percutaneous injection. AJR Am J Roentgenol 1987;149:105-7. [Crossref] [PubMed]
- Boody BS, Savage JW. Evaluation and Treatment of Lumbar Facet Cysts. J Am Acad Orthop Surg 2016;24:829-42. [Crossref] [PubMed]
- Bydon A, Xu R, Parker SL, et al. Recurrent back and leg pain and cyst reformation after surgical resection of spinal synovial cysts: Systematic review of reported postoperative outcomes. Spine J 2010;10:820-6. [Crossref] [PubMed]
- Xu R, McGirt MJ, Parker SL, et al. Factors associated with recurrent back pain and cyst recurrence after surgical resection of one hundred ninety-five spinal synovial cysts: Analysis of one hundred sixty-seven consecutive cases. Spine (Phila Pa 1976) 2010;35:1044-53. [Crossref] [PubMed]


