Sublaminar wire migration into the medulla oblongata: a case report
Introduction
Surgical procedures requiring fusion at the atlantoaxial level have been evolving in an effort to minimize complication rates and ensure solid fusion. Rheumatoid arthritis is commonly associated with atlantoaxial instability (1-3), however, this can also result from congenital, traumatic, neoplastic, and other causes (4). Several techniques were reported for stabilizing and fusing this level (5-7).
In 1939, Gallie fusion was developed to manage atlantoaxial instability (8). This technique involves harvesting an autograft from the iliac crest and reinforcing it with sublaminar wires between the posterior arch of the atlas (C1) and the spinous process of the axis (C2) (6,9). The original Gallie fusion has been criticized for being prone to rotational forces as well as the potential for neural structure damage when sublaminar wires are passed beneath the arch of C1 (7,10). Alternative procedures such as transarticular screw fixation (11) and Halifax interlaminar clamps (12) do not use sublaminar wires, and may bypass some of these aforementioned disadvantages. However, Halifax clamps have recently fallen out of favor due to their higher failure rate associated with poor adherence to counter anterior-posterior translation and rotational forces (13). Gallie fusion was reported to demonstrate a significantly greater atlantoaxial range of motion amongst these techniques (10). It was utilized in our case as the boney anatomy was not conducive to transarticular screw fixation, which was the mainstay of atlantoaxial instrumentation at that time.
We present a case that underwent Gallie fusion 10 years ago and presented recently with a dislodged titanium wire that had migrated into the medulla oblongata resulting in neurological sequelae.
Case presentation
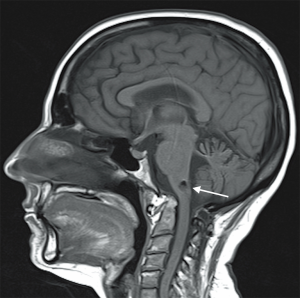
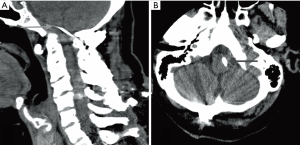
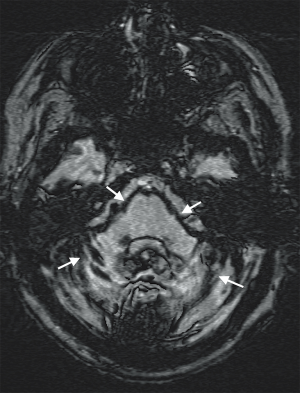
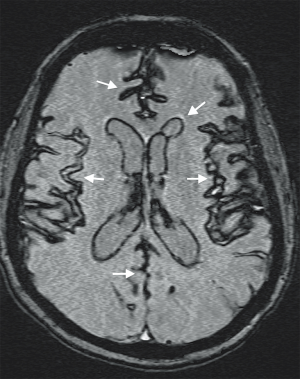
Our patient is a 52-year-old woman who presented in April 2013 with truncal ataxia and regurgitation of small amounts of food. Her past medical history consisted of multiple joint procedures in the limbs. She had also undergone a C1-C2 Gallie fusion over a decade ago. At the time of the original surgery, transarticular screw fixation was considered but discounted due to unfavorable osseous morphology. At the recent presentation, the patient demonstrated impaired cognition and short-term memory. Plain radiographs and a confirmatory computerized tomography (CT) scan revealed that a wire from her previous Gallie fusion procedure had migrated into the medulla oblongata (Figure 1). A lumbar puncture revealed extensive xanthochromia in cerebrospinal fluid (CSF). Susceptibility-weighted magnetic resonance imaging (MRI) noted hemosiderin staining diffusely throughout the cerebellar folia, pial surface of the brainstem (Figure 2) and along ependymal lining of ventricular system (Figure 3). MRI confirmed the migration of the wire into the medulla oblongata (Figure 4). The patient was determined to have ongoing instability at C1-C2 with displacement of a sublaminar wire that migrated into the medulla oblongata. An MR angiogram of the head showed no vascular abnormality. Hence, a surgical decision to remove the intramedullary wire and achieve stable fusion was undertaken.
The patient underwent foramen magnum decompression with C1 bilateral laminectomy and removal of a sublaminar wire. An intraoperative CSF leak was noted from the wire tract and was closed using a dural substitute and sutures, and reinforced with a dural sealant. Once the wire was removed, the occiput to C4 bilateral instrumented fusion was performed using C2 pedicle screws and lateral mass screws at C3 and C4 and contoured titanium rods. During surgery, the somatosensory evoked potentials (SSEP) and motor evoked potentials (MEP) were monitored with no intraoperative change in either modality. Six months following surgery, the patient presented with worsening gait, difficulty with swallowing and left hemiparesis. A CT scan showed pull out of all occipital screws. Another surgical procedure was then undertaken during which all of the cranial hardware was removed. New occipital screws and plate were used. The patient tolerated the procedure well and postoperatively, her gait steadily improved with the assistance of the rehabilitation team.
At her 1-month follow-up, the patient showed improvement in her gait but still had spastic quadriparesis and was able to ambulate short distances with assistance. Three months following surgery the patient experienced episodes of unresponsiveness lasting for approximately 20 s. These were considered to be seizures and she was treated medically with no ongoing seizures. Currently, the patient walks independently with significant improvement in her gait and motor power.
Discussion
There has been progressive improvement in developing surgical techniques to relieve atlantoaxial joint instability. The degree and etiology of atlantoaxial instability varies among cases, and should be evaluated on an individual basis. In our case, the initial plan in 2003 was to perform a transarticular screw plus Gallie-type fusion. However, preoperative imaging revealed significant rotation at C1 on C2 in addition to cranial settling. Transarticular screw fixation was deemed unsafe and a Gallie fusion alone was performed.
Rheumatoid arthritis has an early involvement of the cervical spine by causing chronic inflammatory autoimmune changes (2). The absence of intervertebral disks between the occipito-atlantal and atlantoaxial articulations may deem these joints susceptible for instability and therefore atlantoaxial subluxation (2). The patient’s progressive deterioration of the cervical spine from rheumatoid arthritis may have contributed to the ongoing postoperative atlantoaxial instability. The anterior subluxation was diagnosed 18 months prior to the 2003 Gallie fusion, and was first visualized operatively in the 2003 surgery when a rotatory component was also noted.
In our case, the wire was found protruding into the medulla oblongata several years after the initial Gallie fusion. MRI findings of superficial hemosiderosis were likely to be related to hemorrhage caused by the migrating wire protruding into the medulla oblongata.
Fraser et al. (14) report a broken wire fragment migrating anteriorly into the spinal cord and ventral dura 5 years after their patient underwent suboccipital craniectomy, C1 laminectomy and C1-C2 fusion. The corrective surgery involved a midline mandibulotomy and glossotomy approach. However, the visible wire was chosen not to be resected due to the concern that it may lacerate the spine. An uninfected pseudomeningocele was recognized postoperatively, likely caused by the broken wire penetrating the dura. The patient later underwent a revision surgery of occiput to C3 and C4 fusion with the wire not visible intraoperatively. Radiography demonstrated nine months later that the wire had not migrated further.
Yablon et al. (15) presented a case with a migrated metal rod through the foramen magnum and into the cerebellum four years after a C4-C5 Harrington rod hook fixation for anterior dislocation of C4. Preoperatively, the patient displayed persistent progressive neck pain and dizziness, however no complications occurred after operative correction. The authors report that despite the success of Harrington instrumentation, rod breakage and hardware migration have occurred (4) and advised that frequent follow-up is recommended due to possible spinal instability and instrument migration.
The degree of atlantoaxial instability and range of motion may also be dependent on the fusion technique. Considering the pathoanatomical circumstances of our case, Gallie fusion was deemed as the safest choice. Grob et al. (10) performed biomechanical evaluations of spinal flexibility on cadaveric specimens to determine the posterior atlantoaxial stabilizing capabilities of Gallie fusion, Brooks bilateral graft fusion, transarticular screw fixation and Halifax clamps. Gallie fusion displayed a significantly greater range of motion however less stability amongst the four techniques (10). Transarticular screw fixation was deemed an appropriate fusion technique as it provides stabilization of axial rotation and lateral bending, which are two primary movements of the atlantoaxial joint (10). Despite these results, the authors highlight the varying degree and direction of instability for individual cases and recommend surgeons to perform the technique that accommodates proper stabilization for the most severe instability (10). Our case report highlights the inherent variance among atlantoaxial instability cases, and the necessity for clinicians to base their diagnosis and surgical approach on an individual basis. Regular follow-up and imaging reports are recommended to ensure proper C1-C2 fusion and avoid any long-term complications or recurrence related to atlantoaxial instability.
Conclusions
The authors present a rare case of migration of a sublaminar wire into the medulla oblongata and discuss possible causes. Possible wire migration needs to be considered in the differential diagnosis in patients presenting with neurological sequelae and who have had surgical procedures involving sublaminar wire fusion techniques.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Del Grande M, Del Grande F, Carrino J, et al. Cervical spine involvement early in the course of rheumatoid arthritis. Semin Arthritis Rheum 2014;43:738-44. [Crossref] [PubMed]
- Kim DH, Hilibrand AS. Rheumatoid arthritis in the cervical spine. J Am Acad Orthop Surg 2005;13:463-74. [Crossref] [PubMed]
- Krauss WE, Bledsoe JM, Clarke MJ, et al. Rheumatoid arthritis of the craniovertebral junction. Neurosurgery 2010;66:83-95. [Crossref] [PubMed]
- Dickson JH, Harrington PR, Erwin WD. Results of reduction and stabilization of the severely fractured thoracic and lumbar spine. J Bone Joint Surg Am 1978;60:799-805. [Crossref] [PubMed]
- McGraw RW, Rusch RM. Atlanto-axial arthrodesis. J Bone Joint Surg Br 1973;55:482-9. [PubMed]
- Menendez JA, Wright NM. Techniques of posterior C1-C2 stabilization. Neurosurgery 2007;60:103-11. [Crossref] [PubMed]
- Vender JR, Rekito AJ, Harrison SJ, et al. The evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg Focus 2004;16:E9. [Crossref] [PubMed]
- Gallie WE. Fractures and dislocations of the cervical spine. Am J Surg 1939;46:495-9. [Crossref]
- Denaro V, Di Martino A. Cervical spine surgery: an historical perspective. Clin Orthop Relat Res 2011;469:639-48. [Crossref] [PubMed]
- Grob D, Crisco JJ 3rd, Panjabi MM, et al. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976) 1992;17:480-90. [Crossref] [PubMed]
- Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A. editors. Cervical spine I. 1st ed. Vienna: Springer-Verlag, 1987:(322-7).
- Tucker HH. Technical report: method of fixation of subluxed or dislocated cervical spine below C1-C2. Can J Neurol Sci 1975;2:381-2. [Crossref] [PubMed]
- Benzel EC. The Cervical Spine. Fifth Edition. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2012.
- Fraser AB, Sen C, Casden AM, et al. Cervical transdural intramedullary migration of a sublaminar wire. A complication of cervical fixation. Spine (Phila Pa 1976) 1994;19:456-9. [Crossref] [PubMed]
- Yablon IG, Cowan S, Mortara R. The migration of a Harrington rod after cervical fusion. Spine (Phila Pa 1976) 1993;18:356-8. [Crossref] [PubMed]