Minimally invasive fully endoscopic two-level posterior cervical foraminotomy: technical note
IntroductionOther Section
The surgical treatment of cervical radiculopathy is very successful, with reported success rates greater than 90% for anterior cervical discectomy and fusion as well as for posterior cervical decompression without fusion (1-5). Anterior cervical discectomy is often performed with a fusion and has the downside of exposing patients to a risk of adjacent segment disease over time as well as dysphagia, dysphonia, and neck viscera injury (6). Posterior foraminotomy for cervical radiculopathy carries with it an often painful postoperative course because of the cervical musculature that must be traversed in order to reach the compressive pathology (although minimally invasive approaches likely lessen that pain) and a 3% recurrence rate for symptoms that can ultimately necessitate a subsequent surgery that is an anterior fusion (7). Both anterior and posterior approaches are equally effective (8-10). A minimally invasive posterior cervical approach typically entails sequential dilation down to a 16 to 20 mm tubular retractor through which (I) the target surgical pathology is visualized, and (II) instruments are passed. Here we present a technique for a fully endoscopic 2-level posterior cervical foraminotomy performed through a 1 cm incision using a 1 cm working channel high definition endoscope with a 6 mm working channel. The technique is presented to illustrate a surgical approach that is more minimally invasive than a microendoscopic approach and possibly superior in its visualization of the target pathology.
Case presentationOther Section
History and presentation
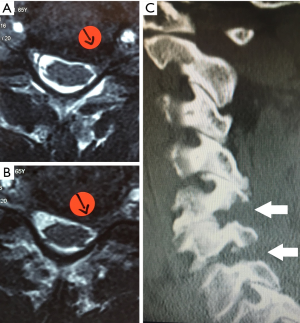
A 65-year-old male patient presented with 1 year of left arm pain and numbness in a C6 and C7 distribution. The patient had already undergone non-operative treatment that included physical therapy, traction, and two epidural steroid injections. On examination, the patient had 4+ motor strength in his left triceps and wrist extension, absent triceps and brachioradialis reflex on the left, and numbness in a C6 and C7 distribution. Magnetic resonance imaging (MRI) revealed stenotic neural foramen on the left at C5–6 and C6–7 (Figure 1).
Operative procedure
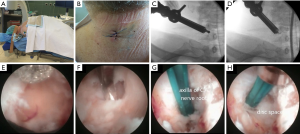
For the posterior cervical endoscopic procedure to decompress the left C5–6 and C6–7 foramina, the patient was positioned prone on hip and chest bolsters on the operating room table with the table flexed and his face in a foam pillow (Figure 2). Using intermittent fluoroscopic guidance, alternating between lateral and anterior-posterior (AP) view, a 25 cm 18 gauge needle was advanced and placed at the medial border of the left C5–6 facet junction. A Kirschner wire (K-wire) was placed through the needle, and incision made over the needle, and the needle was removed. Sequential dilation was performed, and a cannulated tubular retractor was “screwed” through the skin, fascia, and muscle until it was docked on the facet junction. The Joimax Ilessys® Delta rigid endoscope is a 10 mm outer diameter endoscope with a 6 mm working channel through which the endoscopic instruments can be used under continuous endoscopic high definition visualization. The endoscopic foraminotomy procedure was performed in the following steps and is displayed in Figure 2: (I) the radiofrequency probe and graspers were used to clean off the facet tissue and help identify the lamina, facet, and ligamentum flavum; (II) the endoscopic drill was used to perform the foraminotomy at the laminar facet junction at C6–7; (III) the endo-kerrison punches with a 1.5 and 3 mm foot print were used to remove the thin remaining layer of foraminal bone to complete the neural decompression; and (IV) the radiofrequency probe was used was used for hemostasis and is shown in Figure 2 as a dissector elevating the C6 nerve at the axilla and exposing the disc. The disc was not removed because it was felt to be a firm degenerative disc and the bony decompression was sufficient to relieve the patient’s radicular symptoms. The same sequence of steps was used to decompress the C5–6 foramen through the same incision. At the end of the surgery, the cannulated tubular retractor was removed, and the wound was closed with a two interrupted sutures (Figure 1).
Postoperative course
The postoperative course was uneventful, and the patient’s pain improved immediately after surgery. Figure 1B shows the excellent bony decompression demonstrated in the postoperative CT sagittal reconstruction. One year after his endoscopic procedure, the patient has no clinical symptoms related to his previous cervical radiculopathy
DiscussionOther Section
Ruetten in 2008 published a case series of one hundred and seventy-five patients who either underwent a single level anterior cervical discectomy and fusion or a posterior cervical endoscopic foraminotomy utilizing a 5.9 mm working channel endoscope (11). There were no differences in the two patient groups as far as complications or revision rates. Here we present a technique for 2-level posterior cervical foraminotomy through a 10 mm working channel high definition endoscope and a case that highlights three important issues.
First, not all minimally invasive approaches are the same. One could ask what great advantage does reducing the size of the tubular retractor down from 16 to 20 mm used in microendoscopic surgery down to 10 mm retractor used here. The advantages gained by performing a minimally invasive posterior cervical foraminotomy through working channel endoscope are 3 folds: reduced tissue retraction, instrument manipulation is not down the same path as the light for visualizing the surgical pathology, and the light source and camera for visualizing the surgical pathology is directly over the pathology rather than 30–50 cm’s away as it is in the case of an operating microscope.
Second, posterior cervical approaches are now approaching the realm of what could almost be considered percutaneous surgery. Surgeons offering an anterior versus posterior cervical approach to treat cervical radiculopathy will often choose an anterior fusion approach because that procedure is so well tolerated—there is so little muscle retraction and subsequent postoperative pain with that approach. If the posterior cervical foraminotomy procedure could advance to a truly percutaneous procedure that carried with it very little postoperative pain, then surgeons and patients in choosing two well tolerated procedures may consider the procedure that does not entail a fusion.
Third, the endoscopic procedure presented here may look like a standard minimally invasive cervical foraminotomy with the surgical application of drills, graspers, kerrison punch, and bipolar, but it is very different. The procedure is performed under continuous irrigation, so visualization is extremely clear because bleeding is diluted and irrigated away. The surgeon does not need to clean the kerrison or graspers with each use but can open the instrument and the irrigation will wash the tissue out the endoscope side port. One major difference and disadvantage that has to be appreciated by surgeons considering this type of approach is that the surgical instruments are used “one-at-a-time”. Meticulous microscopic technique when working to decompress cervical nerve roots might entail using a dissector at the same time as a drill or kerrison punch when decompressing a nerve root. In the endoscopic surgery presented here, only one instrumented is used at a time down the working channel—no “helper” instruments are in the field. Continuous irrigation is helpful for both obviating the need for using suction instruments and for acting as a retractor in pulsing away the dural and neural elements, but the endoscopic procedure is technically different from the microendoscopic procedure in more than just the method of visualization during the procedure.
ConclusionsOther Section
Degenerative spine disease in the aging population is a growing problem as this portion of our population grows. The evolution of minimally invasive solutions to degenerative spine pathologies makes sense to patients who want to get back to life more quickly and may make sense to health care delivery systems as we have to consider how to pay for caring for this aging population. Other studies have shown that microendoscopic minimally invasive cervical foraminotomy is as successful as an open surgical approach for the same disease pathology (12,13). Patients with symptomatic cervical radiculopathy from foraminal stenosis can be effectively managed with either a traditional open or a minimally invasive foraminotomy, and here we describe an endoscopic technique for performing a multilevel posterior cervical foraminotomy that highlights nuances of a procedure that offers both advantages and challenges to the spine surgeon who is trying to take advantage of the newest advances in the growing technology available in minimally invasive spine surgery.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
ReferencesOther Section
- Alvin MD, Lubelski D, Abdullah KG, et al. Cost-Utility Analysis of Anterior Cervical Discectomy and Fusion With Plating (ACDFP) Versus Posterior Cervical Foraminotomy (PCF) for Patients With Single-level Cervical Radiculopathy at 1-Year Follow-up. Clin Spine Surg 2016;29:E67-72. [PubMed]
- Henderson CM, Hennessy RG, Shuey HM Jr, et al. Posterior-lateral foraminotomy as an exclusive operative technique for cervical radiculopathy: a review of 846 consecutively operated cases. Neurosurgery 1983;13:504-12. [Crossref] [PubMed]
- Herkowitz HN, Kurz LT, Overholt DP. Surgical management of cervical soft disc herniation. A comparison between the anterior and posterior approach. Spine (Phila Pa 1976) 1990;15:1026-30. [Crossref] [PubMed]
- Quintana LM. Complications in anterior cervical discectomy and fusion for cervical degenerative disc disease. World Neurosurg 2014;82:1058-9. [Crossref] [PubMed]
- Tomaras CR, Blacklock JB, Parker WD, et al. Outpatient surgical treatment of cervical radiculopathy. J Neurosurg 1997;87:41-3. [Crossref] [PubMed]
- Nanda A, Sharma M, Sonig A, et al. Surgical complications of anterior cervical diskectomy and fusion for cervical degenerative disk disease: a single surgeon's experience of 1,576 patients. World Neurosurg 2014;82:1380-7. [Crossref] [PubMed]
- Clarke MJ, Ecker RD, Krauss WE, et al. Same-segment and adjacent-segment disease following posterior cervical foraminotomy. J Neurosurg Spine 2007;6:5-9. [Crossref] [PubMed]
- Lubelski D, Healy AT, Silverstein MP, et al. Reoperation rates after anterior cervical discectomy and fusion versus posterior cervical foraminotomy: a propensity-matched analysis. Spine J 2015;15:1277-83. [Crossref] [PubMed]
- Mansfield HE, Canar WJ, Gerard CS, et al. Single-level anterior cervical discectomy and fusion versus minimally invasive posterior cervical foraminotomy for patients with cervical radiculopathy: a cost analysis. Neurosurg Focus 2014;37:E9. [Crossref] [PubMed]
- Selvanathan SK, Beagrie C, Thomson S, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien) 2015;157:1595-600. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:940-8. [Crossref] [PubMed]
- McAnany SJ, Kim JS, Overley SC, et al. A meta-analysis of cervical foraminotomy: open versus minimally-invasive techniques. Spine J 2015;15:849-56. [Crossref] [PubMed]
- Song Z, Zhang Z, Hao J, et al. Microsurgery or open cervical foraminotomy for cervical radiculopathy? A systematic review. Int Orthop 2016;40:1335-43. [Crossref] [PubMed]


