Intraoperative navigation for accurate midline placement of anterior lumbar interbody fusion and total disc replacement prosthesis
Background
Anterior lumbar approach techniques for the management of discogenic back pain and placement of spinal instrumentation such as fusion and disc replacement prosthesis is becoming increasingly popular (1-7). However, these procedures may provide the surgeon with a limited view of the anatomy around the target region of the spine, with potential poor placement of spinal prosthesis (8). Fluoroscopic guidance has been utilized to make surgery safer by localizing and confirming the placement of the prosthesis. However this guidance method still presents a risk for improper cage positioning and also exposes the surgeon to increased radiation (8,9). An alternative is intraoperative spinal navigation using 3-dimensional (3D) computed tomography (CT). CT-based navigation has been shown to reduce radiation exposure for the surgeon, and improve spinal visualization, allowing more accurate placement of an instrumentation device (8,10,11). Accurate midline placement of a replacement disc is particularly important for its optimal biomechanical function and longevity (12,13). False positioning of a replacement disc can also cause of plethora of issues including spondylarthrosis and degeneration of adjacent discs (14).
It has been demonstrated that CT-based spinal navigation for pedicle screws insertion provides greater safety and accuracy when compared to fluoroscopic guidance and free-hand techniques (15). Similar results have been found in several reports using CT-based spinal navigation with lateral lumbar interbody fusion (LLIF) (8,16). The use of CT navigation with anterior lumber interbody fusion (ALIF) has also been shown to provide greater accuracy and less variation in device placement, though only in cadaveric models (14). To date, no studies have reported the clinical usage of spinal navigation with ALIF and total disk replacement (TDR). As a result, this case report will present the surgical technique of intraoperative CT-based navigation for a patient requiring ALIF and TDR.
Case presentation
A 35-year-old female physiotherapist presented with persisting multilevel (L3-S1) discogenic lower back pain over a 4-year time period. Her lower back pain had persisted despite prolonged conservative treatment including physiotherapy and multiple medical interventions including injection therapy and surgery. She had previously undergone two lumbar microdiscectomy procedures at L4/5 and L5/S1 at a different institution. There was no further relevant medical or social history.
Magnetic resonance imaging (MRI) of the lumbosacral spine revealed advanced degenerative disc and facet joint disease affecting L4/5 and L5/S1. Bone/SPECT Scan revealed disco-vertebral and facet joint uptake at the L4/5 and L5/S1 levels. Provocative discography revealed pain on injection of the lower 3 discs including the L3/4 level, with the L2/3 injection painless. A decision was made to manage the lower 3 lumbar disc levels.
Following consultation with a senior spine surgeon (RJM), the patient underwent a three level anterior reconstructive procedure, including L3/L4 disc arthroplasty, L4/L5 and L5/S1 ALIF procedure, with assistance of intraoperative CT navigation for positioning and confirmation of midline placement of the TDR. During the procedure, the patient was positioned supine under general anaesthesia on a Trumpf spinal table. The skin was prepared and draped in the usual fashion for anterior approach lumbar surgery. A linear incision and retroperitoneal exposure of the anterior vertebral bodies of L3/4, L4/5 and L5/S1 was performed by a vascular surgeon, with mobilization of the anterior vessels at L3/4 and L4/5.
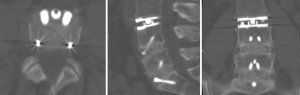
Image intensification was used to re-confirm the levels of pathology. The corresponding disc spaces were cleared out and endplates prepared. An ALIF was performed using allograft (AusBiotechnologies, Sydney, Australia) and BMP-2 (Infuse, Medtronic, USA) at L5/S1 and L4/L5 (Midline ALIF design, Centinel Spine, USA). Prior to placement of the disc prosthesis, an intraoperative CT scan was performed using the Airo/BrainLab (Germany) navigation system. Using navigation probes, the midline and angulation of insertion was determined using CT based navigation (Figure 1). At the L3/L4 level, an LP-ESP (LH Orthopaedics, France) disc prosthesis was implanted with a height of 10 mm at 9 degrees lordosis. Following implantation of the prosthesis, a further intraoperative CT was performed to confirm the accurate alignment and depth of all implants (Figure 2). The wound was then closed in standard fashion. There were no surgical complications and the blood loss was minimal at 80 cc.

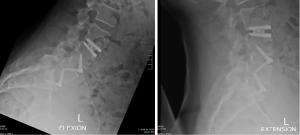
Postoperative X-rays at 6 weeks (Figure 3) demonstrated accurate placement of all prosthesis. Flexion/Extension X-rays at 3 months confirmed acceptable movement of the disc replacement prosthesis at L3/4 (Figure 4). The patient has experienced significant reduction of discogenic pain and returned to work as a physiotherapist at 4 months post-operative.
Discussion
While TDR has been shown to have high clinical success, studies have reported complication rates of up to 12% and unsatisfactory results in up to 37% of patients (14,17,18). The main cause of these poor outcomes include incorrect sizing of implants, incorrect indications for surgery and malpositioning of the implant (14,18). An implant must be placed accurately at the midline for optimum function, durability and clinical outcomes (8,10,11,14). If the positioning of the device is not correct, complications can arise such as coronal tilt and scoliosis, abnormal loading of the facet joints and adjacent disc degeneration (14).
Fluoroscopy is often used to aid the surgeon with implantation of the cage into the disc space at the correct position and orientation. This procedure often involves constant repositioning of the fluoroscope, which can be inconvenient and cause prolonged exposure to radiation to the surgical team (8,19). In addition, parallax error can occur leading to malpositioning of the implant(14,20). To avoid the issues associated with fluoroscopy guidance, intraoperative CT guidance systems may be used as an alternative. CT-guidance can aid the surgeon’s navigation into the disc space by providing real time 3D images. Park 2015 found that this method of navigation was safe, feasible and appeared to be accurate in LLIF procedures (8). This finding is similar to that of Joseph et al., who also used intraoperative CT and an image-guided navigation system for LLIF cage placement (16). A literature review of 26 prospective clinical trials also found that the percentage of inserted screws contained within the pedicle was 89% to 100% when using CT navigation (15). This displayed much higher accuracy and safety when compared to the free-hand technique and fluoroscopy guided method (15). Furthermore, various studies have shown that there is minimal radiation exposure to the surgeon and theatre staff when using an O-arm or cone beam CT imaging system for spinal navigation (19,21).
In a study by Kafchitsas et al. [2009], a spine surgeon without a prior learning curve used navigation to perform ALIF and TDR on 10 human cadavers (14). Their study reported that CT-navigation instruments improve accuracy and produce less variation than traditional fluoroscopy guidance. In their sample, three prostheses were placed suboptimally, with none placed poorly (defined as >5 mm from the preferred position). Also, the accuracy of device placement was greatest in the coronal plane. Anatomical limitations influencing prosthesis positioning in the midsagittal plane could be caused by lordosis (14). The stiffness of spinal ligaments and endplate of the vertebra may also influence prosthesis placement in the craniocaudal plane (14). Additionally, the accurate placement of the prosthetics were completed by an experienced spine surgeon with no experience in TDR, suggesting that navigation for TDR does not require the completion of the learning curve (14). This is supported by findings from other surgical procedures such as acetabular cup placement, where accurate implantation with navigation was not dependent on surgeon experience (22,23).
For multilevel fusion, surgeons may perform the operation using navigation based on just an initial image. This can present significant issues as the insertion of a prosthesis into one of the treated disc spaces can cause the anatomy of adjacent disc spaces to potentially be altered (8). As a result, subsequent navigation to the remaining disc spaces will not be as accurate. It has been suggested that while cage placement will cause significant disc height expansion superiorly, minimal changes will occur distally (8). As a result the relationship between the distal spinal segments and the fixed anterior superior iliac spine will be mostly unaffected. Accordingly, for multilevel spinal fusion procedures it has been recommended that a distal-to-proximal order of implant insertion be performed (8). Thus the finding by Park 2015 that device placement in multilevel fusion was less accurate, can be potentially explained by their use of a proximal-to-distal order of cage insertion (8).
Conclusions
ALIF and TDR remain a validated surgical intervention in the setting of treatment resistant discogenic back pain. The routine implementation of intra-operative CT-based navigation is not only radiologically safe but provides additional visualisation to the surgeon over conventional methods. We demonstrate accurate screw placement and favourable patient outcomes partially attributable to the information provided from the intra-operative guidance via CT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient.
References
- Wood M, Mannion R. A comparison of CT-based navigation techniques for minimally invasive lumbar pedicle screw placement. J Spinal Disord Tech 2011;24:E1-5. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Daly D, et al. Approach-Related Complications of Anterior Lumbar Interbody Fusion: Results of a Combined Spine and Vascular Surgical Team. Global Spine J 2016;6:147-54. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [PubMed]
- Mobbs RJ, Phan K, Thayaparan GK, et al. Anterior Lumbar Interbody Fusion as a Salvage Technique for Pseudarthrosis following Posterior Lumbar Fusion Surgery. Global Spine J 2016;6:14-20. [Crossref] [PubMed]
- Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg 2015;29:705-11. [Crossref] [PubMed]
- Phan K, Lee NJ, Kothari P, et al. Risk Factors for Readmissions Following Anterior Lumbar Interbody Fusion. Spine (Phila Pa 1976) 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Rao PJ, Ghent F, Phan K, et al. Stand-alone anterior lumbar interbody fusion for treatment of degenerative spondylolisthesis. J Clin Neurosci 2015;22:1619-24. [Crossref] [PubMed]
- Park P. Three-dimensional computed tomography-based spinal navigation in minimally invasive lateral lumbar interbody fusion: feasibility, technique, and initial results. Neurosurgery 2015;11 Suppl 2:259-67. [Crossref] [PubMed]
- Sharma AK, Kepler CK, Girardi FP, et al. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech 2011;24:242-50. [Crossref] [PubMed]
- Geerling J, Gösling T, Gösling A, et al. Navigated pedicle screw placement: experimental comparison between CT- and 3D fluoroscopy-based techniques. Comput Aided Surg 2008;13:157-66. [Crossref] [PubMed]
- Merloz P, Tonetti J, Pittet L, et al. Pedicle screw placement using image guided techniques. Clin Orthop Relat Res 1998.39-48. [Crossref] [PubMed]
- Goel VK, Faizan A, Palepu V, et al. Parameters that effect spine biomechanics following cervical disc replacement. Eur Spine J 2012;21 Suppl 5:S688-99. [Crossref] [PubMed]
- Smith HE, Vaccaro AR, Yuan PS, et al. The use of computerized image guidance in lumbar disk arthroplasty. J Spinal Disord Tech 2006;19:22-7. [Crossref] [PubMed]
- Kafchitsas K, Rauschmann M. Navigation of artificial disc replacement: evaluation in a cadaver study. Comput Aided Surg 2009;14:28-36. [Crossref] [PubMed]
- Gelalis ID, Paschos NK, Pakos EE, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 2012;21:247-55. [Crossref] [PubMed]
- Joseph JR, Smith BW, Patel RD, et al. Use of 3D CT-based navigation in minimally invasive lateral lumbar interbody fusion. J Neurosurg Spine 2016;25:339-44. [Crossref] [PubMed]
- McAfee PC, Cunningham B, Holsapple G, et al. A prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine (Phila Pa 1976) 2005;30:1576-83; discussion E388-90.
- Cinotti G, David T, Postacchini F. Results of disc prosthesis after a minimum follow-up period of 2 years. Spine (Phila Pa 1976) 1996;21:995-1000. [Crossref] [PubMed]
- Abdullah KG, Bishop FS, Lubelski D, et al. Radiation exposure to the spine surgeon in lumbar and thoracolumbar fusions with the use of an intraoperative computed tomographic 3-dimensional imaging system. Spine (Phila Pa 1976) 2012;37:E1074-8. [Crossref] [PubMed]
- Nowitzke A, Wood M, Cooney K. Improving accuracy and reducing errors in spinal surgery--a new technique for thoracolumbar-level localization using computer-assisted image guidance. Spine J 2008;8:597-604. [Crossref] [PubMed]
- Nottmeier EW, Bowman C, Nelson KL. Surgeon radiation exposure in cone beam computed tomography-based, image-guided spinal surgery. Int J Med Robot 2012;8:196-200. [Crossref] [PubMed]
- Honl M, Schwieger K, Gauck CH, et al. Comparison of total hip replacements cup orientation and position. Navigation vs. conventional manual implantation of hip prostheses. Orthopade 2005;34:1131-6. [Crossref] [PubMed]
- Honl M, Schwieger K, Salineros M, et al. Orientation of the acetabular component. A comparison of five navigation systems with conventional surgical technique. J Bone Joint Surg Br 2006;88:1401-5. [Crossref] [PubMed]



