Lumbar fusion surgery for degenerative conditions is associated with significant resource and narcotic use 2 years postoperatively in the commercially insured: a medical and pharmacy claims study
Introduction
Chronic low back pain continues to be one of the costliest and most complex chronic medical conditions to manage, with lifetime prevalence in adults approaching 85% and an annual incidence of 15% to 20% in the United States. Back pain is reported to be the most common complaint requiring a physician evaluation (1-4), and accounts for 41% to 87% of worker’s compensation costs, second to only upper respiratory infections as a cause of work absenteeism (5). In 2005, the United States spent nearly $86 billion treating back pain, a 65% increase from $52.1 billion spent in 1997 (6). Use of lumbar spine fusion surgery, or lumbar fusion (LF) to treat chronic back pain increased 220% from 1990–2001 among Medicare beneficiaries (7,8), despite conflicting evidence for significant long term pain relief or improved outcomes. Deyo et al. identified increasing trends among Medicare beneficiaries in complex fusion procedures for spinal stenosis, and an increase in both complications and resource consumption with added surgical complexity (9). The rate of complex fusion procedures increased 15-fold from 2002–2007, and complications were found to increase concomitantly with increasing surgical invasiveness (9). Limited improvement in surgical and pain management outcomes combined with high costs suggest questionable value of LF (3). We used longitudinal data from 2009 Cigna beneficiaries to examine outcomes and utilization over two years following an index LF procedure to relieve back pain from degenerative conditions.
Methods
Design
We used a longitudinal cohort design with 2-year observation following index LF per beneficiary, measuring outcomes and utilization based on ongoing lumbar spine related medical and pharmacy claims over the early postoperative period. We chose a 2-year follow up period to examine outcomes and utilization extending beyond the immediate postoperative period. The data were from Cigna’s national claim database of over 8.5 million beneficiaries. There were 1,422 Cigna patients with continuous eligibility 2 years following the initial fusion procedure identified and included in this study group. Patients with LF performed from January 1, 2009 through September 30, 2009 with benefit eligibility through December 31, 2011 were included. Medicare primary and workers’ compensation patients were excluded, as were claims related to cervical or thoracic spine. Our analysis captured any additional planned or unplanned lumbar surgery procedures, complications including hardware issues and infections, pain management procedures, high tech radiology, physical therapy, acupuncture and chiropractic.
ICD-9-CM codes related to lower back (lumbar spine) and primary LF CPT codes 22612, 22630 and/or 22558 were identified. Diagnostic codes included lumbar intervertebral disc disorders, lumbago, backache, sciatica, spondylosis, degenerative disc, spinal stenosis, herniated disc and low back pain. All associated secondary CPT codes for the index fusion date of service were captured including instrumentation, decompression and bone graft codes. Claims with diagnostic codes related to fracture, tumor, infection, spondylolisthesis, inflammatory arthritis or deformity were excluded. Pharmacy claims were identified for specific therapeutic classes including narcotic and non-narcotic analgesics, antidepressants, antimanics, anticonvulsants, antipsychotics, anxiolytics, centrally acting and GABA-derived muscle relaxants, fibromyalgia medications and stimulants. Sustained release opioid medications were also identified in those patients on narcotics more than 1 year following LF. We conducted descriptive analyses of outcomes and utilization among these patients.
Results
Of the 1,422 patients in the study (Table 1), 87% or 1,241 patients continued to receive medical or pharmacy services related to back pain during the two years following the initial LF. A total of 70% or 992 continued to receive lumbar-related medical services incurring an additional $9.0 million in claims payment during the 2-year period following surgery at an average expense of $9,683 per patient. The study population with Cigna pharmacy benefits (829 patients) incurred an additional $2.2 million in claims payment during the 2-year period following surgery at an average expense of $2,600 per individual. Total average expenditure for combined medical and pharmacy services during the 2-year period was $12,283/individual. Many LF patients were younger with 43% being less than 50 years of age. There were 58% female and 42% male patients.
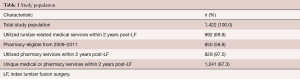
Full table
Surgical and non-operative interventions
One hundred and ninety four patients (13.6%) received additional single or multiple level lumbar surgical procedures within 24 months of the initial surgery, including 125 additional LF surgical procedures performed in 123 patients, with 8.6% procedures consisting of anterior or posterior interbody as well as posterolateral fusions (Table 2). There were 71 (5%) additional surgical procedures performed with or independent of additional LF surgical procedures. These procedures included instrumentation revision or removal, sacroiliac joint fusion, decompression procedures, fusion exploration and osteotomy procedures. It is not possible to determine if these procedures were for complications or other issues at the same level or additional levels from this claim database analysis. Some additional surgery may have included planned staged procedures on different dates of service.
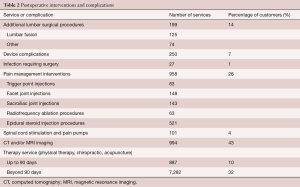
Full table
Device complications required additional surgical intervention in 106 patients (7%) during the study period. Fourteen patients (1%) had documentation of an infection, which included five with meningitis, who required 40 additional surgical procedures based on reported ICD-9 codes 996.4, 996.40–996.49, 996.67, 996.70, 996.78, 998.9, V5401.
Pain management interventions were identified for 349 patients (25%) who received a total of 958 lumbar spine procedures following LF which included 83 trigger point injections, 143 sacroiliac joint injections, 148 facet injections, 63 radiofrequency ablation, and 521 epidural steroid injection procedures.
Sixty-three (4.4%) patients also received additional pain management interventions with 41 patients receiving a spinal cord stimulator placement and 9 patients receiving intrathecal pain pump-related procedures within the 24-month period.
Six hundred and five (42.5%) of the LF patients received 994 additional lumbar computerized axial tomography (CT) and/or magnetic resonance imaging (MRI) procedures, which averaged 1.6 services per patient in this group. A subset of this group also received discography, epidurogram and/or myelography.
Post operatively, 592 patients (41.6%) received therapy services consisting of physical therapy, chiropractic and/or acupuncture with 457 members (32.1%) continuing to receive therapy services more than 90 days postoperatively.
Pharmacy
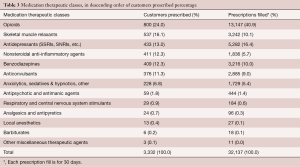
A subset of 850 patients out of 1,422 (60%) of the study population had Cigna pharmacy benefit from 2009–2011 and 829/850 patients (97%) continued to receive multiple categories of pain related medications over the 2-year period following LF. The average number of prescriptions filled post operatively for back-related symptoms per patient was 38.8 at an average cost of $2,600 per patient. Narcotic utilization for 30 days or longer was found in 775 out of 829 (93%) patients while 484/775 (62%) continued to receive narcotics more than 1 year after LF surgery. Those on narcotics beyond 1 year received on average 23.5 narcotic prescriptions refills during the study period. Medications were filled from 4 of the listed categories on average postoperatively. Of the 484 patients on narcotics more than 1 year following LF, sustained release opioid medications were prescribed to 633 patients indicating some patients received more than one sustained release product. It is not feasible from the study to determine the preoperative compared to postoperative total morphine milligram equivalent utilization per patient.
Further analysis was performed to determine those fusion patients in this study group with pharmacy benefit from 2009 to 2011 to determine those patients with Cigna pharmacy benefits in 2008, prior to the LF procedure. A total of 734 members from the study group had pharmacy eligibility in 2008 and post-surgically through 2011.
In 2008, 517/734 of patients with pharmacy eligibility received at least one narcotic prescription prior to LF surgery. A secondary analysis found that 492 of those 517 patients (95%) continued to receive narcotic medications more than 1 year postoperatively. Patients receiving postoperative narcotic medications averaged three different brand name narcotics including sustained release products which averaged 1.3 products per patient for those on narcotics beyond 1 year postoperatively. Opioids were the most commonly prescribed medication in the population, accounting for more than 40% of all prescriptions filled (Table 3).
Full table
Discussion
Our findings are noteworthy in providing evidence for substantial resource use and narcotic use postoperatively in the timeframe of 2 years following LF surgery among a commercially insured population at a time when the opioid epidemic is escalating and the Centers for Disease Control and Prevention have issued guidelines urging clinicians to seek other first-line analgesic therapies (10). Our results indicate that LF for degenerative lumbar related back pain is associated with additional surgical and/or pain management intervention procedures post operatively. Ongoing pain medication utilization was found in the majority of patients based on pharmacy claims data, with 62% of pharmacy benefit patients on narcotics over 1 year postoperatively and nearly 30% continuing to receive postoperative pain management procedures including epidural steroid and sacroiliac joint injections, facet injections, and radiofrequency ablation procedures as well as spinal cord stimulation. It is not possible to determine if other medical conditions existed for the medications provided, but based on ICD-9 codes available, the medications utilized in this observational group are primarily related to the lumbar diagnosis for which the LF was performed. 95% of patients with a Cigna pharmacy benefit both preoperatively and postoperatively and who received a narcotic medication preoperatively continued to receive long term narcotics postoperatively. Patients receiving preoperative and postoperative narcotic medications averaged three different narcotic brand names postoperatively. Of the 484 patients on narcotics beyond 1 year, sustained release products were often used by some patients based on 633 different prescriptions being prescribed to this subset.
LF for spinal instability including spondylolisthesis is supported in the peer reviewed literature. There are evidence-based peer reviewed outcome studies which support improved patient outcomes when a fusion is performed during spinal stenosis decompression surgery, when an associated spondylolisthesis exists at the level of decompression (11-15). However, fusion surgery for back pain in the absence of instability is not proven to provide any further improvement compared with an integrated nonoperative approach (16). There is also limited evidence for the effectiveness of one type of fusion technique over another (17).
Our data suggest that ongoing pain continues in the majority of patients who receive LF, as evidenced by continued medication utilization and other pain intervention services. Our findings are consistent with those of Castel and colleagues, who observed that narcotics and injections comprised the majority of pain interventions (18). Our findings were also consistent with those of Fritzell and colleagues, who observed that back pain over 2 years was reduced only 33% in LF patients (19). Deyo further reported that innovation has often outpaced clinical science regarding back pain management, which leaves uncertainty about the efficacy and safety of many common treatments. He further reported that complications and even deaths related to back pain management are increasing (8). Brox and colleagues performed a randomized study in 2003 that found equal improvement in patients with chronic low back pain and disc degeneration whether randomized to cognitive intervention and exercises or LF surgery (16). It is likely that continued pain management interventions and pain-related medication utilization will continue beyond 2 years. Also, adjacent segment degeneration may occur beyond this time period that could require additional nonoperative and surgical intervention years later incurring additional costs.
The American Academy of Orthopaedic Surgery (AAOS) endorsed the American Pain Society evidence based guidelines on “Interventional therapies, surgery and interdisciplinary rehabilitation for low back pain” and recommended physicians consider intensive interdisciplinary rehabilitation with a cognitive/behavioral emphasis for management of patients with nonradicular low back pain who do not respond to usual, non-interdisciplinary interventions (20). Evidence-based recommendations also include shared decision-making regarding surgery for nonspecific low back pain include a specific discussion about intensive interdisciplinary rehabilitation as a similarly effective option as the small to moderate average benefit from surgery versus non-interdisciplinary nonsurgical therapy, and the fact that the majority of such patients who undergo surgery do not experience an optimal outcome (defined as minimum or no pain, discontinuation of or occasional pain medical use, and return of high-level function) (20).
Our study was limited in that preoperative to postoperative comparison of patient-level opioid and other pain-related mediation use, including comparative morphine milligram equivalent utilization were not feasible. While it is possible that medication usage may have been associated with other medical conditions, the diagnostic codes submitted primarily indicated the lumbar spine as the principal source of pain in this observational study group. The long-term utilization of opioid medications for chronic back pain continues in the majority of this study group, and the utilization trend suggests continued narcotic and other classes of pain related medications are likely to last beyond this 2-year study. In addition, future studies should seek to report more detailed longitudinal information about shorter-term interim outcomes (e.g., 6 months).
LF was followed by continued narcotic and other psychotropic medication utilization in the majority of the patients, including on average more than one sustained release opioid in the subset on narcotics more than one year postoperatively. The ability of surgeons to effectively provide pain resolution with LF for back pain is not supported by this study. Lee et al. reported the use of increased narcotic consumption prior to spine surgery predicted worse patient reported outcomes and suggested a multidisciplinary approach with psychological and opioid screening including weaning of opioids in the preoperative period and close opioid monitoring in the postoperatively (21). Sullivan et al. found the proportion of individuals with non-cancer pain conditions receiving narcotics continued to increase from 2000–2005 (22) and concluded in another study that the use of opioids for chronic non-cancer pain is increasing, noting that more than half of patients with regular prescription opioid use for common psychiatric disorders have back pain (23).
Surgeons are often not able to accurately determine underlying psychological issues that may impact back pain. Daubs et al. found that a large percentage of patients (64%) presenting for spine evaluation have some level of psychological distress. It was further reported that compared with a standardized questionnaire designed to screen for psychological distress, spinal surgeons had low sensitivity rates to detect this distress (24).
Our study identified medical and pharmacy claims that occurred in the first 2 years following LF surgery; our findings were consistent with findings by D’Oro and colleagues that lumbar fusion surgery leads to subsequent costly complications and procedures (25).
A coordinated collaborative approach to chronic nonradicular back pain management has been shown to reduce pharmacy medications, disability and provide overall improved outcomes (5). There is evidence that supports exercise therapy in the management of chronic low back pain (26,27). The creation of programs centered on interdisciplinary spine or back pain management which integrates medical and surgical management as well as “behavioral medicine, physical reconditioning, and societal reintegration represent the model of high-value care for patients with chronic spine pain.” (5). The data and results of this study suggests there is value and opportunity for collaborative physician and health service company programs to improve individual health through a patient centric approach to support improved shared decision making with patient level real time data.
Smith notes that although 90% of spine pain resolves within 6 weeks, direct and indirect costs have been estimated as high as $100 billion per year in the United States, and the aging U.S. demographics are compounding this problem which necessitates optimizing value with high-quality care in the future (5,25). Ivanova et al. found that individuals with low back pain have high rates of baseline comorbidities and resource use associated with opioids commonly prescribed early (28). The results of the present study in a younger commercially insured population questions the value of LF for management of low back pain when considering the ongoing resource utilization and associated costs identified. As healthcare migrates from volume to value based care, collaborative relationships with real time individual level data sharing between physicians and health service companies should develop to support evidence based care.
Conclusions
Our findings indicate LF surgery for management of degenerative low back pain is associated with additional surgical procedures, with ongoing pain management intervention procedures post operatively in many of the individuals studied. Pain medication utilization and especially long term narcotic use persists in the majority of patients based on pharmacy claims data. Those patients on narcotics preoperatively continue on narcotics long term postoperatively. Surgery performed to significantly reduce pain medication utilization postoperatively is not supported in this study. Although this study only analyzed medical and pharmacy use over the 2 years following LF, the pattern of utilization did not suggest additional use of these resources would discontinue beyond this time period.
The functional outcomes for individual patients cannot be determined from this study but it is reasonable to conclude the majority of patients continued experiencing pain for which the LF surgery was performed based on the multiple medication utilization including opioid use on a long term basis. Our findings do not support the efficacy or postoperative cost savings of LF surgery for back pain, and moreover we observed significant continuing postoperative costs through utilization of pharmacy, medical, and surgical resources.
Acknowledgements
The authors thank Drs. Gregory Przybylski and Stuart Lustig for critical review of drafts.
Footnote
Conflicts of Interest: All authors were employed by Cigna at the time this work was performed and all work was performed at and funded by Cigna.
Ethical Statement: All work was performed in the course of treatment, payment, and operations as part of a quality improvement initiative incorporating the principles of the World Medical Association Declaration of Helsinki.
References
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-5. [Crossref] [PubMed]
- Carey TS, Freburger JK, Holmes GM, et al. A long way to go: practice patterns and evidence in chronic low back pain care. Spine (Phila Pa 1976) 2009;34:718-24. [Crossref] [PubMed]
- Hanley EN Jr, David SM. Lumbar arthrodesis for the treatment of back pain. J Bone Joint Surg Am 1999;81:716-30. [Crossref] [PubMed]
- Hanley EN Jr, Herkowitz HN, Kirkpatrick JS, et al. Debating the value of spine surgery. J Bone Joint Surg Am 2010;92:1293-304. [Crossref] [PubMed]
- Smith MJ. Accountable disease management of spine pain. Spine J 2011;11:807-15. [Crossref] [PubMed]
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Crossref] [PubMed]
- Deyo RA, Gray DT, Kreuter W, et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441-5; discussion 1446-7. [Crossref] [PubMed]
- Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med 2009;22:62-8. [Crossref] [PubMed]
- Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259-65. [Crossref] [PubMed]
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain. Available online: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
- Bridwell KH, Sedgewick TA, O'Brien MF, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 1993;6:461-72. [Crossref] [PubMed]
- Lumbar Fusion for Spinal Instability and Degenerative Disc Conditions, Including Sacroiliac Fusion. Cigna Healthcare Coverage Policy 0303. Available online: https://cignaforhcp.cigna.com/public/content/pdf/coveragePolicies/medical/mm_0303_coveragepositioncriteria_lumbar_fusion_degenerative_conditions.pdf
- Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 1991;73:802-8. [Crossref] [PubMed]
- North American Spine Society, 2007. Clinical guidelines for multidisciplinary spine care. Diagnosis and treatment of degenerative lumbar spinal stenosis. Available online: https://www.spine.org/ResearchClinicalCare/QualityImprovement/ClinicalGuidelines.aspx
- Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 2009;91:1295-304. [Crossref] [PubMed]
- Brox JI, Sørensen R, Friis A, et al. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine (Phila Pa 1976) 2003;28:1913-21. [Crossref] [PubMed]
- Lee CS, Hwang CJ, Lee DH, et al. Fusion rates of instrumented lumbar spinal arthrodesis according to surgical approach: a systematic review of randomized trials. Clin Orthop Surg 2011;3:39-47. [Crossref] [PubMed]
- Castel LD, Freburger JK, Holmes GM, et al. Spine and pain clinics serving North Carolina patients with back and neck pain: what do they do, and are they multidisciplinary? Spine (Phila Pa 1976) 2009;34:615-22. [Crossref] [PubMed]
- Fritzell P, Hägg O, Wessberg P, et al. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 2001;26:2521-32; discussion 32-4. [Crossref] [PubMed]
- Chou R, Loeser JD, Owens DK, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976) 2009;34:1066-77. [Crossref] [PubMed]
- Lee D, Armaghani S, Archer KR, et al. Preoperative Opioid Use as a Predictor of Adverse Postoperative Self-Reported Outcomes in Patients Undergoing Spine Surgery. J Bone Joint Surg Am 2014;96:e89. [Crossref] [PubMed]
- Sullivan MD, Edlund MJ, Fan MY, et al. Trends in use of opioids for non-cancer pain conditions 2000-2005 in commercial and Medicaid insurance plans: the TROUP study. Pain 2008;138:440-9. [Crossref] [PubMed]
- Sullivan MD, Edlund MJ, Steffick D, et al. Regular use of prescribed opioids: association with common psychiatric disorders. Pain 2005;119:95-103. [Crossref] [PubMed]
- Daubs MD, Patel AA, Willick SE, et al. Clinical impression versus standardized questionnaire: the spinal surgeon's ability to assess psychological distress. J Bone Joint Surg Am 2010;92:2878-83. [Crossref] [PubMed]
- D’Oro A, Spoonamore MJ, Cohen JR, et al. Effects of fusion and conservative treatment on disc degeneration and rates of subsequent surgery after thoracolumbar fracture. J Neurosurg Spine 2016;24:476-82. [Crossref] [PubMed]
- Bronfort G, Maiers MJ, Evans RL, et al. Supervised exercise, spinal manipulation, and home exercise for chronic low back pain: a randomized clinical trial. Spine J 2011;11:585-98. [Crossref] [PubMed]
- Shen FH, Samartzis D, Andersson GB. Nonsurgical management of acute and chronic low back pain. J Am Acad Orthop Surg 2006;14:477-87. [Crossref] [PubMed]
- Ivanova JI, Birnbaum HG, Schiller M, et al. Real-world practice patterns, health-care utilization, and costs in patients with low back pain: the long road to guideline-concordant care. Spine J 2011;11:622-32. [Crossref] [PubMed]


