Management of progressive late onset scoliosis with magnetic growth rod insertion leading to improvement of neural anomalies—a case report
Introduction
Early onset scoliosis refers to the spinal deformity which are presented before the age of ten years. Bracing has been used to prevent further progression of scoliosis during the active growth period. But we often find very weak compliance as a result of physical and psychological stress (1). Conventional growing rods have traditionally been the most commonly used distraction-based devices in the treatment of progressive early onset scoliosis. The literature describes advantages of magnetic growth rods (MGR) compared with conventional growing rods, especially the avoidance of repeated surgical lengthening procedures, in the safe and effective treatment of early and late onset scoliosis (2,3). The Magnetic rods are also deemed to be cost effective (4).
The association of intraspinal anomalies with scoliosis is well documented and early surgical management have shown to improve the outcome of scoliosis (5,6). Chiari malformation and syringomyelia are the commonest neural anomalies, both of which create diagnostic and treatment challenges in patients with progressive scoliosis requiring surgical correction (7-9).
In our center, all such cases are discussed in a formal Spinal Neurosurgical Multi-disciplinary Team meeting, with patients considered for foramen magnum decompression prior to scoliosis surgery if deemed appropriate. All such scoliosis patients are monitored with serial magnetic resonance imaging (MRI) scans to exclude any deterioration in their Chiari malformation or syringomyelia.
There is little data reported in the literature to date about the improvement of conservatively managed Chiari malformation or syringomyelia following corrective posterior spinal fusion surgery for scoliosis, and no such data at all, for patients with MGR insertion. We present the first known reported case of juvenile idiopathic scoliosis with Chiari malformation and syringomyelia found to have significant improvement in both intraspinal anomalies after MGR insertion and subsequent serial distractions.
Methods
A 10-year-old Caucasian female presented with a progressive spinal deformity, diagnosed as early adolescent idiopathic scoliosis on plain radiography. She was born by an uncomplicated normal vaginal delivery, achieved all her developmental milestones normally, had no significant medical background and no family history of scoliosis. On examination, the shoulders were level and there was no clinical evidence of pelvic obliquity. Adam’s forward bending test revealed a moderate right sided rib hump. There were no stigmata of spinal dysraphism, and no neurological deficit. Initial plain radiography revealed a right thoracic scoliosis with a Cobb angle measurement of 51 degrees from T4 to T12 at aged 10.
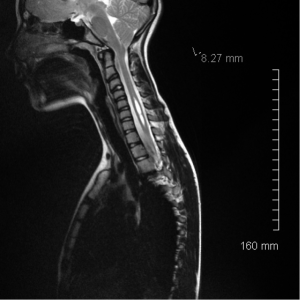
Upon routine follow-up review, the Cobb angle continued to progress to 66 degrees over 11 months, therefore surgical correction with MGR insertion was proposed as best management. Pre-operative MRI of the whole spine demonstrated a small cervicothoracic syrinx, and a Chiari type I malformation with a cerebellar tonsillar descent measured as 8.27 mm upon T2 weighted sagittal MRI sequences. The associated syrinx measured 3.5 mm × 5.6 mm on the axial image and longitudinally it measured 41 mm on the sagittal images (Figure 1).
After discussion at our Neurosurgical Spinal Multi-Disciplinary team meeting, a consensus was reached that no further intervention was required for the syringomyelia or Chiari malformation, and deemed safe to proceed with corrective surgery for the scoliosis.
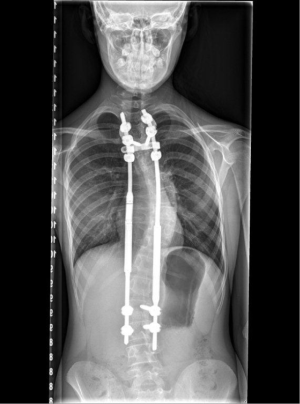
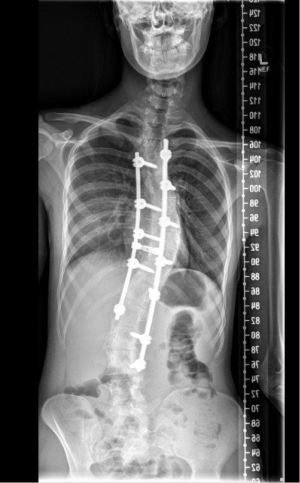
MGR insertion was therefore performed at the age of twelve with two limited posterior incisions placed in the midline in the upper thoracic and lumbar spine. Bilateral pedicle screws were inserted at T2 and T3 as well as L2 and L3, and dual MGRs were implanted via a submuscular approach. The rod was anchored proximally and distally at the points above. The operation was uncomplicated, with normal spinal cord monitoring traces (both motor evoked potentials and sensory evoked potentials) throughout. Post-operative radiography was satisfactory, demonstrating the pedicle screws and MGR appropriately in place, and a reduction in the Cobb angle to 45 degrees (Figure 2).
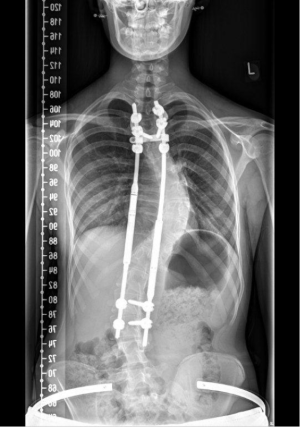
The patient was subsequently followed up periodically on a six-monthly basis for 48 months, with her successfully having lengthening of her MGR in the outpatient clinic and confirmatory plain radiography at each visit (Figure 3). She remained asymptomatic with a well-healed surgical scar and no neurological dysfunction throughout this follow-up period.
At this stage 48 months after her index operation, the patient developed thoracolumbar back pain and serous discharge from the cranial end of her upper thoracic incision with granuloma formation. Culture and microscopy of a discharge fluid sample demonstrated no bacterial growth, and the patient underwent surgical washout and debridement with primary closure of the wound. There was again no bacterial growth seen within deep tissue samples obtained at the time of surgery. The patient subsequently had worsening of her thoracolumbar back pain and further granuloma formation warranting complete surgical removal of the posterior spinal metalwork 48 months after the index procedure. There was no subsequent clinical or biochemical evidence of infection.
The Cobb angle of the residual thoracic curve measured 60 degrees immediately after removal of the spinal metalwork. The scoliosis continued to deteriorate over the next 18 months with a Cobb angle measuring 80 degrees. With the patient now 18 years old and skeletally mature on radiography, the decision was made to treat the scoliosis with a definitive single stage posterior instrumented spinal fusion.
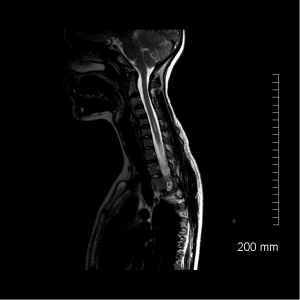
Concurrently, the patient developed subjective transient altered sensation of the hands, therefore a contemporary MRI scan of the whole spine was arranged to exclude an increase in the size of the syringomyelia or extent of the Chiari malformation. This imaging in fact demonstrated a reduction in the size of the Chiari malformation to 2.15 mm from 8.27 mm. The size of the cervicothoracic syrinx has also reduced to 1.5 mm × 3.1 mm × 25 mm (Figure 4) from 3.5 mm × 5.6 mm × 41 mm.
The patient therefore underwent her definitive posterior spinal fusion for correction of her scoliosis with pedicle screw and dual rod instrumentation from T3 to L3 without complication. She has made a full recovery from this operation after 4 months of follow up (Figure 5).
Results
After 48 months of serial distractions of the implanted MGR in this patient, the previously diagnosed Chiari type I malformation was incidentally found to have significantly improved without any direct decompressive neurosurgical intervention on MRI scanning. The cervicothoracic syrinx also decreased in size.
Conclusions
This is a unique case of apparently spontaneous radiological resolution of a Chiari malformation and improvement in syringomyelia in a patient with progressive late onset scoliosis treated with MGR insertion as the primary corrective procedure. No such case has been reported in the literature to date to the best of our knowledge. There is a paucity of published data with respect to the management and outcome of both Chiari malformation and syringomyelia, and also little knowledge about the behavior of these intraspinal anomalies in patients undergoing surgical spinal deformity correction.
This case suggests that uncomplicated syringomyelia and Chiari malformations may improve with gradual and protracted lengthening distraction of the vertebral column in cases of scoliosis. We advocate further clinical research specifically investigating the behavior of such intraspinal anomalies in the context of sequential spinal deformity correction, particularly in the context of MGR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Selle A, Seifert J, Carus CG, et al. Early night-time-bracing – an alternative in AIS management. Scoliosis 2010;5:O57. [Crossref]
- Cheung KM, Cheung JP, Samartzis D, et al. Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 2012;379:1967-74. [Crossref] [PubMed]
- Figueiredo N, Kananeh SF, Siqueira HH, et al. The use of magnetically controlled growing rod device for pediatric scoliosis. Neurosciences (Riyadh) 2016;21:17-25. [Crossref] [PubMed]
- Jenks M, Craig J, Higgins J, et al. The MAGEC system for spinal lengthening in children with scoliosis: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 2014;12:587-99. [Crossref] [PubMed]
- Eule JM, Erickson MA, O'Brien MF, et al. Chiari I malformation associated with syringomyelia and scoliosis: a twenty-year review of surgical and nonsurgical treatment in a pediatric population. Spine (Phila Pa 1976) 2002;27:1451-5. [Crossref] [PubMed]
- Hwang SW, Samdani AF, Jea A, et al. Outcomes of Chiari I-associated scoliosis after intervention: a meta-analysis of the pediatric literature. Childs Nerv Syst 2012;28:1213-9. [Crossref] [PubMed]
- Godzik J, Holekamp TF, Limbrick DD, et al. Risks and outcomes of spinal deformity surgery in Chiari malformation, Type 1, with syringomyelia versus adolescent idiopathic scoliosis. Spine J 2015;15:2002-8. [Crossref] [PubMed]
- Bradley LJ, Ratahi ED, Crawford HA, et al. The outcomes of scoliosis surgery in patients with syringomyelia. Spine (Phila Pa 1976) 2007;32:2327-33. [Crossref] [PubMed]
- Charry O, Koop S, Winter R, et al. Syringomyelia and scoliosis: a review of twenty-five pediatric patients. J Pediatr Orthop 1994;14:309-17. [Crossref] [PubMed]