
Online access to spine care: do institutions advertise themselves as multidisciplinary?
Introduction
Spine-related injuries are some of the most common problems leading patients to seek medical care (1). Low back pain for instance has been estimated to affect around 80% of the population at least one point in life, with 1–2% of the U.S. population disabled due to low back pain (2-4). Furthermore, 12–30% of adults have an active back problem (1,5). With over 10% of primary care visits stemming from back or neck pain, spine care has become the fifth most common reason for physician visits overall and leads to $86 billion in healthcare spending (6-8). The prevalence and expenditures pertaining to spinal conditions are continuing to increase as well, even though the health status of patients is not necessarily improving (6,9).
Given the wide range of medical specialties involved in the management of spine conditions, a new shift towards multidisciplinary spine care has emerged (10). Spine disorders involve a complex pathophysiology consisting of psychosocial, mechanical, and neurologic factors, thereby necessitating collaboration in diagnosing and treating such conditions (10,11). Yanamadala et al. specifically discusses how the majority of patients initially advised to undergo lumbar fusion surgery were instead recommended nonoperative management after assessment by a multidisciplinary panel (12). Such work highlights the importance of comprehensive multidisciplinary assessment in many similar patient scenarios so to limit the excessive costs and resource over-utilization associated with unnecessary surgery scheduling.
Previous literature has detailed the design and goals of comprehensive spine care centers, such as at the University of Missouri and at the University of Iowa (13,14). However, there has yet to be a comprehensive study regarding the extent to which institutions across the country have adopted multidisciplinary models. Clarifying such trends is of value to spine care providers, healthcare systems, and patients, as these lead to better understanding of how many institutions are aspiring towards such a model and how many are feasibly applying its principles in practice.
The primary aim of our study is to assess the extent to which healthcare systems advertise their spine care programs as multidisciplinary and furthermore clarify whether these institutions accurately reflect this description in their online access to spine care. The secondary aim of our study is to determine what proportion of institutions enable patients to self-schedule appointments online and select providers. We hypothesize that the majority of institutions describe their spine care approach as integrated, but that only a small fraction of these will have combined websites and phone numbers for multidisciplinary spine-focused divisions. We furthermore hypothesize that the majority of patients will not be able to schedule appointments online without having an online portal with their respective institution or choose their own providers.
Methods
Since this study utilized publicly available information, Institutional Review Board approval was not required prior to commencing this investigation. To obtain an extensive list of top-rated hospitals in the country for the purposes of this study, we utilized Newsweek’s 2021 list entitled “Best Hospitals 2021-United States”. A team of three research assistants analyzed each institution’s spine care websites to assess whether their approach to spine care was self-described as “multidisciplinary” and conferenced together with the principal investigator to ensure uniform approaches to website analysis. Institutions were considered to have advertised themselves as multidisciplinary if they used this term or similar wording (such as “care encompassing broad range of specialties”, “interdisciplinary”, “multidisciplinary”). Each institution’s website was additionally assessed for the existence of: (I) a standard overview website or multiple individual sites for respective spine-focused divisions (i.e., orthopaedic surgery, neurosurgery, physical medicine and rehabilitation, anesthesiology); (II) online self-scheduling; (III) triage questions prior to requesting appointments; and (IV) selection choice for specific providers. Online self-scheduling was considered having the ability to select a specific time and date from an online scheduler to meet with a physician, not simply submitting an online form to be considered for an appointment. An additional requirement to be considered self-scheduling for this study was the ability to register for an appointment online via a calendar-based scheduling interface without needing a specific medical record portal for the respective institution. Institutions which had online self-scheduling or personal phone numbers to schedule appointments with physicians were deemed to have selection choice for specific providers.
Statistical analysis
Descriptive statistics and percentages were utilized to summarize the assessed institutions according to utilization of multidisciplinary terminology, spine center website design, phone numbers for contact, option for online self-scheduling, presence of triage questions, and choice of provider. All requested variables were compared between groups using chi-square or Fisher’s exact tests (if expected cell counts are <5). All analyses were performed using SPSS.
Results
In total, 334 institutions were included in analysis. The majority (66%) utilized multidisciplinary terminology in describing their institution on their website.
Institutions described as multidisciplinary were more likely to have a link on a central page to each division (31% vs. 4%, P<0.001; Figure 1A,1B). No significant differences were found between institutions described as multidisciplinary and those not described as such when considering triage questions and online self-scheduling. Regardless of whether or not the institutions considered themselves multidisciplinary on their online descriptions, few allowed for online self-scheduling, with only 5.9% and 7.2% of “multidisciplinary” and “not-multidisciplinary” programs allowing this opportunity online. A similar pattern was noted with regards to institutions providing triage questions online. Very few triaged patients with these, with 4.5% of the “multidisciplinary” and 1.2% of the “non-multidisciplinary” institutions using these questions to triage patients appropriately the correct providers. Furthermore, there were no significant differences in choice of provider between institutions described as multidisciplinary and those described as such (Figure 2).
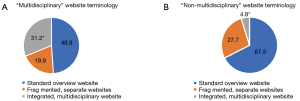
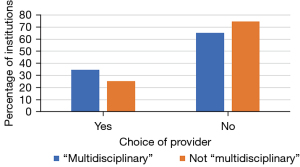
Additionally, most only had a standard overview website with no separate websites for respective divisions (54%). Though 32% of patients had a choice of selecting their provider, only 6% were able to do so via online self-scheduling. Full descriptive statistics regarding the institutions assessed are provided in Table 1.
Table 1
| Institution characteristics | N | % |
|---|---|---|
| “Multidisciplinary” website terminology | ||
| Yes | 221 | 66.2 |
| No | 83 | 24.9 |
| No website | 30 | 9.0 |
| Spine center website | ||
| Standard overview website | 164 | 53.9 |
| Fragmented, separate websites | 67 | 22.0 |
| Integrated, multidisciplinary website | 73 | 24.0 |
| Online self-scheduling | ||
| Yes | 19 | 6.3 |
| No | 285 | 93.8 |
| Triage questions | ||
| Yes | 11 | 3.6 |
| No | 293 | 96.4 |
| Choice of provider | ||
| Yes | 98 | 32.2 |
| No | 206 | 67.8 |
| Imaging requirements prior to appointment | ||
| Yes | 2 | 0.7 |
| No | 302 | 99.3 |
Discussion
Although a majority of institutions providing spine care described themselves as multidisciplinary, approximately half still only had standard overview websites with no way to explore their respective divisions. Institutions described as multidisciplinary were more likely to have an integrated website with links on a central page to each division. Despite this, these self-described multidisciplinary institutions still did not utilize triage questions, online self-scheduling, and choice of provider to a greater degree than websites not described as multidisciplinary. These results show how despite the commonplace use of multidisciplinary branding among spine care institutions, there remains a chasm between the online branding and an actual multidisciplinary online user experience.
Patients with spine issues are often burdened to not only understand which institution to choose, but also which specialty they should see, and which provider within that specialty is right for them. They choose and then often have to wait in a queue, and are often placed back in another queue if they are then directed to a provider of the appropriate specialty. This can lead to treatment delays, inefficiencies in terms of scheduling with the inappropriate provider, and overall frustration with the healthcare process. For example, a patient with lower back pain who is first scheduled to visit an orthopedic spine surgeon only to be referred to a physiatrist afterwards is likely to be frustrated by the increased time and costs of care. Optimally, the patient could instead initially have been scheduled for an appointment with a physiatrist at the online point of access. It is well understood that multidisciplinary spine care is optimal, and institutions with truly multidisciplinary systems internally would be expected at the least to provide initial multidisciplinary web browsing experiences with central institutional spine care sites linking patients to the spectrum of operative and nonoperative care resources and providers, with guidance to patients on how to obtain the proper care (15,16). Given how the service industry has evolved so that scheduling a restaurant reservation or even a haircut can be done with ease, the healthcare industry and from our results, need for spine care in particular, remains far behind in streamlining accessible, integrated experience for patients. Patients may benefit significantly from optimized scheduling of online care, as Luxenburg et al. shows how older and more ill patients are less likely to schedule appointments when the process is difficult (17). Further research supports the importance of online self-scheduling in empowering patient-centered care and satisfaction while providing advantages to traditional phone scheduling (18,19).
Despite the increased demand for spine and the rising expenditure to meet this demand, outcomes have not significantly improved (6,7,9,20-24). A contributing factor to the lack of improvement is that the current systems of delivering care to these patients are cumbersome and filled with inefficiencies. Yeung et al. [2021] highlighted many of the issues existing with the current state of spine care and proposed several solutions (11). The article highlighted the complexity of spine care involving physical, mental, social, and economic components, and variety of health care professionals and backgrounds involved in the care of these patients. Physicians and advanced practice providers from emergency medicine, primary care, neurosurgery, orthopedic surgery, physical medicine and rehabilitation, neurology, and other providers like physical therapists, chiropractors, acupuncturists could all be involved in the care of these patients (25,26). Among the problems existing in spine care are that non-surgical patients are commonly referred to surgeons. This both delays patients from receiving timely and appropriate care, as well as becomes a burden on surgeons’ schedules (27). Therefore systems need to be updated to allow for appropriate referrals and the providers within these systems should work in integrated multidisciplinary models of spine care. Patients seeking care should encounter a user-friendly system that directs them to timely and appropriate care.
Furthermore, Chen and Yang [2008] discussed what an interdisciplinary spine center at an academic medical center looks like (14). A team of orthopedic surgeons, physiatrists, physical therapists, vocational counselor, medical social worker, health psychologist, and administrative staff were all involved in the care of spine patients. Methods of care involved surgical, non-surgical, social, and psychological methods. They identified several keys to success including: common mission amongst providers, integrated scheduling and triage, patient preference, interdisciplinary team works in close proximity and meets frequently. Similarly, Drymalski and Agha [2017] provided another example of how a comprehensive spine center can benefit patients by also integrating a multidisciplinary group of health care professionals (13). They also described changes they made to the referral process where a single call center prioritized patients seeing non-operative physicians first unless urgent surgical need was warranted. In doing so they reduced wait times and increased the proportion of appropriate surgical candidates being referred to surgeons. Further research showing prioritization of non-operative providers and utilization of multidisciplinary teams for triage has shown reductions in overall spine costs and improvements in the proportion of surgical patients being referred to surgeons (28,29). Figure 3 illustrates an optimized model of multidisciplinary spine care triaging and scheduling.
One limitation to this study would be that only hospitals included on Newsweek’s 2021 list entitled “Best Hospitals 2021-United States” were taken into consideration. Given how this was the case, we likely excluded certain hospitals from analysis due to the finite nature of this list. Regardless, we feel that this Newsweek source provided an adequate sample size of 334 institutions and also a strong representation of diverse healthcare institutions with respect to geography, academic vs. private focus, and patient population size. A second limitation would be the subjective nature of some of the outcome measures in this study, such as categorization of institutions as describing themselves as multidisciplinary. Online access of institutional websites was the sole factor considered in making these designations, as other avenues such as in-person marketing weren’t considered. To limit any variation from this aspect of the study design, data recorded for each institution was cross-checked multiple times by separate authors on this project to ensure proper accuracy. Lastly, another limitation would be the limited existing literature regarding multidisciplinary spine care. No previous studies to our understanding have categorized spine care website according to whether they are described as multi-disciplinary and ensuingly assessed features representative of multidisciplinary care, making our investigation a pilot study in this aspect. Given how this is a novel area of research, the subjective nature of some of our outcome measures still provide valuable insights that have not yet been elucidated.
Conclusions
While a majority of institutions providing spine care advertise themselves as multidisciplinary, only a fraction of these actually allow patients the ability on their websites to explore the individual disciplines providing care. Only a small percentage of these highly ranked institutions allow patients to select their providers, self-schedule, or easily match to their appropriate spine care provider through a triage process. Spine care involves a complex, multidisciplinary array of providers, and this subspecialization can often confuse patients and lead to inefficiencies and fragmentation of care. It is incumbent on these institutions to provide the best, most user-friendly and truly integrated experience to their patients, and this often begins when patients search for the right care team online.
In non-healthcare industries, it is commonplace for consumers to be able to explore details of customer journey, and have the ability to self-schedule their experiences online. With continued effort and investment, institutions within healthcare can continue to evolve in their missions of providing high quality, transparent, patient-friendly spine and overall clinical experiences.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-38/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Casiano VE, Sarwan G, Dydyk AM, et al. Back Pain. In: StatPearls. Treasure Island: StatPearls Publishing, 2022. (cited 2022 Jul 14).
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med 2001;344:363-70. [Crossref] [PubMed]
- Yan W, Yu Y, Wang Y, et al. Research Relating to Low Back Pain and Physical Activity Reported Over the Period of 2000-2020. J Pain Res 2021;14:2513-28. [Crossref] [PubMed]
- Miki T, Higuchi D, Takebayashi T, et al. Factors associating with disability of non-specific low back pain in different subgroups: A hierarchical linear regression analysis. Sci Rep 2021;11:18278. [Crossref] [PubMed]
- Koes BW, van Tulder MW, Ostelo R, et al. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine (Phila Pa 1976) 2001;26:2504-13; discussion 2513-4. [Crossref] [PubMed]
- Martin BI, Turner JA, Mirza SK, et al. Trends in health care expenditures, utilization, and health status among US adults with spine problems, 1997-2006. Spine (Phila Pa 1976) 2009;34:2077-84. [Crossref] [PubMed]
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976) 2006;31:2724-7. [Crossref] [PubMed]
- Hines K, Mouchtouris N, Getz C, et al. Bundled Payment Models in Spine Surgery. Global Spine J 2021;11:7S-13S. [Crossref] [PubMed]
- Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Crossref] [PubMed]
- Sindaco G, Vigneri S, Zanella M, et al. The Development of a Multidisciplinary Spine Center: A New Shared Approach for Pain Care. Pain Pract 2017;17:281-3. [Crossref] [PubMed]
- Yeung CM, Lightsey HM 4th, Isaac S, et al. Improving Spine Models of Care. JBJS Rev 2021;9:e20.00183.
- Yanamadala V, Kim Y, Buchlak QD, et al. Multidisciplinary Evaluation Leads to the Decreased Utilization of Lumbar Spine Fusion: An Observational Cohort Pilot Study. Spine (Phila Pa 1976) 2017;42:E1016-23. [Crossref] [PubMed]
- Drymalski M, Agha M. The Changing Face of Spine Care: The MU Comprehensive Spine Center. Mo Med 2017;114:44-6. [PubMed]
- Chen JJ, Yang RK. A look inside an interdisciplinary spine center at an academic medical center. Iowa Orthop J 2008;28:98-101. [PubMed]
- Benton JA, Mowrey WB, De La Garza Ramos R, et al. A Multidisciplinary Spine Surgical Indications Conference Leads to Alterations in Surgical Plans in a Significant Number of Cases: A Case Series. Spine (Phila Pa 1976) 2021;46:E48-55. [Crossref] [PubMed]
- Huynh MA, Roldan C, Nunes P, et al. Characteristics of Patients and Treatment Recommendations from a Multidisciplinary Spinal Tumor Program. Palliat Med Rep 2020;1:143-8. [Crossref] [PubMed]
- Luxenburg O, Myers V, Ziv A, et al. Factors Affecting the Patient Journey in Scheduling a Specialist Appointment in a Public Healthcare System. J Patient Exp 2022;9:23743735221092547. [Crossref] [PubMed]
- Woodcock EW. Barriers to and Facilitators of Automated Patient Self-scheduling for Health Care Organizations: Scoping Review. J Med Internet Res 2022;24:e28323. [Crossref] [PubMed]
- Matulis JC, McCoy R. Patient-Centered Appointment Scheduling: a Call for Autonomy, Continuity, and Creativity. J Gen Intern Med 2021;36:511-4. [Crossref] [PubMed]
- Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine (Phila Pa 1976) 1995;20:11-9. [Crossref] [PubMed]
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain 2012;13:715-24. [Crossref] [PubMed]
- Kim LH, Vail D, Azad TD, et al. Expenditures and Health Care Utilization Among Adults With Newly Diagnosed Low Back and Lower Extremity Pain. JAMA Netw Open 2019;2:e193676. [Crossref] [PubMed]
- Davis MA, Onega T, Weeks WB, et al. Where the United States spends its spine dollars: expenditures on different ambulatory services for the management of back and neck conditions. Spine (Phila Pa 1976) 2012;37:1693-701. [Crossref] [PubMed]
- Mafi JN, McCarthy EP, Davis RB, et al. Worsening trends in the management and treatment of back pain. JAMA Intern Med 2013;173:1573-81. [Crossref] [PubMed]
- Murphy DR, Justice BD, Paskowski IC, et al. The establishment of a primary spine care practitioner and its benefits to health care reform in the United States. Chiropr Man Therap 2011;19:17. [Crossref] [PubMed]
- Murphy DR, Justice B, Bise CG, et al. The primary spine practitioner as a new role in healthcare systems in North America. Chiropr Man Therap 2022;30:6. [Crossref] [PubMed]
- Ahmad HS, Yang AI, Basil GW, et al. Towards personalized and value-based spine care: objective patient monitoring with smartphone activity data. J Spine Surg 2022;8:87-92. [Crossref] [PubMed]
- Fox J, Haig AJ, Todey B, et al. The effect of required physiatrist consultation on surgery rates for back pain. Spine (Phila Pa 1976) 2013;38:E178-84. [Crossref] [PubMed]
- Wilgenbusch CS, Wu AS, Fourney DR. Triage of spine surgery referrals through a multidisciplinary care pathway: a value-based comparison with conventional referral processes. Spine (Phila Pa 1976) 2014;39:S129-35. [Crossref] [PubMed]



