
Frequency and determinants of surgical treatment in patients with uncomplicated disc-related sciatica hospitalized in the Rheumatology Department of Lille University Hospital
Introduction
Lumbosciatica is a condition affecting the L5 and/or S1 nerve roots, resulting in lower back pain radiating to a lower limb along a specific root path (1).
It is a frequent condition, with about 100,000 cases/year and a prevalence of 3–5% (2). Most cases of sciatica evolve favorably further to rest, treatment with analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs), and possibly epidural corticosteroid injection (1,3).
Although several randomized controlled trials have reported that surgery is more effective than conservative management in the short term (6 weeks to 6 months), no significant differences in pain or functional disability have been reported in the longer term (1, 2 and 5 years) (4-12). As such, discounting complications requiring urgent intervention (motor deficit ≤3/5 and cauda equina syndrome), surgery is generally only performed in patients in whom medical treatment has failed (13).
The evolution of lumbosciatica is usually favorable without surgery, which highlights the interest of medical management for the vast majority of patients.
However, a post-hoc analysis of the Spine Patient Outcomes Research Trial (SPORT) highlighted better outcomes when surgery is early (14).
In addition, patients with severe sciatica who are resistant to first-line medical treatment often visit hospitals’ emergency departments, and once a surgical emergency is ruled out, they are usually admitted to the rheumatology department in France. These patients represent only a small proportion of patients with sciatica—but they are the ones with the most severe forms of the condition.
The main objective of our study was to assess the proportion of patients treated by surgery one year after hospitalization in a rheumatology department for uncomplicated disc-related sciatica.
Our secondary objective was to identify possible determinants of surgical outcome. We present the following article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-43/rc).
Methods
This was a retrospective, observational, single-center study conducted at the Rheumatology Department of Lille University Hospital Center (LUHC) between January 2014 and December 2018. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The National Commission for Data Processing and Liberties approved the study and individual consent for this retrospective analysis was waived.
Patients
Patients were selected from the LUHC Medical Information Department’s records and were included if they were over 18 years of age and were hospitalized for uncomplicated disc-related sciatica. They were excluded if they had an indication for emergency surgery during hospitalization (i.e., motor deficit less than or equal to 3/5, cauda equina syndrome).
Data collection
The data were collected retrospectively from the patients’ computerized medical records. Follow-up was performed in out-patients visits with rheumatologists and/or surgeons.
Statistical analysis
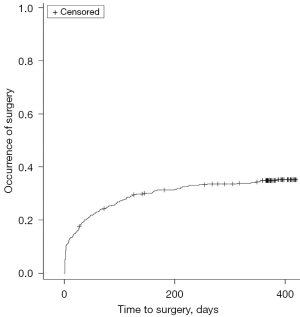
The surgery rate was estimated using the Kaplan-Meier method.
Factors associated with the probability of surgery were analyzed using univariate Cox proportional hazards models. Hazard ratios were calculated with their 95% confidence interval (CI). Significant factors (P<0.05) considered to be the most clinically relevant were included in a multivariate Cox model with stepwise backward selection, with a selection criterion of P<0.10.
Missing data were treated by multiple imputations under the assumption “missing at random” using the chained equation method with 10 imputations. Quantitative variables were imputed using predictive mean matching, and qualitative variables using logistic regression models (binomial, ordinal or multinomial according to the number and order of the modalities) (15). Rubin’s rules were used to combine the estimates obtained in each imputed dataset (16).
All statistical tests were two-tailed with a 5% significance level. Statistical analyses were performed using SAS software (SAS Institute Inc., Cary, NC 25513, version 9.4).
Results
Of the 450 patients hospitalized for disc-related sciatica between 2014 and 2018, 405 were included (Figure 1). The description of our population is presented in Table 1.
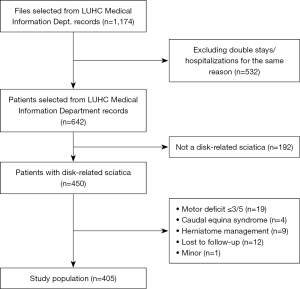
Table 1
| Patients’ characteristics | N (%) or mean (SD) |
|---|---|
| Gender (female) | 214 (52.8) |
| Age (years) | 47.5 (13.8) |
| BMI (kg/m²) | 27.4 (6.1) |
| Charlson Comorbidity Index | 1.47 (2.02) |
| Working | 260 (69.5) |
| Precipitating factor | 161 (50.6) |
| Carrying heavy load | 77 (24.2) |
| Wrong move | 31 (9.8) |
| Duration of symptoms | |
| Acute: <1 month | 208 (51.4) |
| Sub-acute: 1–3 months | 70 (17.3) |
| Chronic: >3 months | 127 (31.3) |
| Positive straight leg-raising test | 283 (76.0) |
| Impulsive pain | 220 (68.8) |
| Motor loss ⅘ | 129 (31.9) |
| Hypoesthesia | 97 (24.3) |
| Concordant herniated disc on cross-sectional images (CT or MRI) | 347 (89.9) |
P<0.05 considered significant. SD, standard deviation; BMI, body mass index; CT, computed tomography; MRI, magnetic resonance imaging.
The analysis of the occurrence of herniated disc surgery after hospitalization for uncomplicated disc-related sciatica revealed a rate of 34.8% at 1 year and 37.5% at 2 years (Figure 2). The median time to surgery was 31 days, with interquartiles of 3 and 112 days.
Univariate and multivariate associations of baseline factors with the risk of surgery are presented in Tables 2,3.
Table 2
| Univariate analysis | Hazard ratio (95% CI) | P |
|---|---|---|
| Biometric data | ||
| Gender (female) | 1.123 (0.816; 1.548) | 0.476 |
| Age (years) | 0.992 (0.980; 1.003) | 0.153 |
| BMI (kg/m²) | 0.953 (0.917; 0.990) | 0.013 |
| Medical background | ||
| Charlson Comorbidity Index | 0.756 (0.616; 0.928) | 0.0075 |
| Active smoking | 1.935 (1.326; 2.824) | 0.0006 |
| Working | 2.213 (1.433; 3.419) | 0.0003 |
| Carries heavy loads at work | 1.047 (0.707; 1.552) | 0.818 |
| Anamnesis | ||
| Carrying heavy load | 0.942 (0.598; 1.486) | 0.798 |
| Wrong move | 0.766 (0.380; 1.545) | 0.457 |
| Duration of symptoms | ||
| Acute: <1 month | 1 | |
| Sub-acute: 1–3 months | 1.170 (0.737; 1.856) | 0.505 |
| Chronic: > 3 months | 1.669 (1.173; 2.375) | 0.0044 |
| Treatment prior to hospitalization | ||
| Non-steroidal anti-inflammatory drugs | 1.323 (0.949; 1.847) | 0.099 |
| Corticosteroids | 1.266 (0.811; 1.975) | 0.299 |
| Morphine | 1.591 (1.115; 2.271) | 0.011 |
| Epidural glucocorticoid injections | 1.346 (1.139; 1.591) | 0.0005 |
| Clinical findings at admission | ||
| Low back pain | 1.109 (0.721; 1.706) | 0.637 |
| Spinal stiffness | 1.041 (0.719; 1.506) | 0.831 |
| Nerve root pain distribution | ||
| S1 | 1 | |
| L5 | 0.714 (0.508; 1.005) | 0.0533 |
| L5 and S1 | 0.488 (0.178; 1.333) | 0.162 |
| Not systematized | 1.034 (0.607; 1.763) | 0.902 |
| Complete radiculalgia | 1.245 (0.855; 1.813) | 0.252 |
| Positive straight leg-raising test | 2.022 (1.270; 3.220) | 0.003 |
| Impulsive pain | 2.238 (1.407; 3.560) | 0.0007 |
| Motor loss ⅘ | 1.463 (1.055; 2.035) | 0.024 |
| Hypoesthesia | 1.228 (0.855; 1.766) | 0.2666 |
| Concordant herniated disc on cross-sectional images (CT or MRI) | 3.996 (1.636; 9.761) | 0.0024 |
| Hospital care | ||
| Length of hospital stay (days) | 1.045 (1.012; 1.080) | 0.008 |
| IV NSAIDs | 1.539 (1.067; 2.220) | 0.021 |
| Corticosteroids | 0.901 (0.519; 1.562) | 0.710 |
| Anti-neuropathic treatment | 0.949 (0.642; 1.403) | 0.795 |
| Initial numeric pain-scale rating | 0.975 (0.900; 1.057) | 0.544 |
| Decrease in numeric pain-scale rating between beginning and end of hospitalization | 0.898 (0.846; 0.953) | 0.0004 |
| Infiltrative management | ||
| Epidural glucocorticoid injections | 3.219 (1.784; 5.81) | 0.0001 |
| Number of injections received per patient before and during hospitalization | 1.55 (1.326; 1.813) | <0.0001 |
P<0.05 considered significant. CI, confidence interval; BMI, body mass index; CT, computed tomography; MRI, magnetic resonance imaging; IV, intravenous; NSAIDs, non-steroidal anti-inflammatory drugs.
Table 3
| Multivariate analysis | Hazard ratio (95% CI) | P |
|---|---|---|
| BMI (kg/m²) | – | 0.17 |
| Charlson Comorbidity Index | – | 0.87 |
| Working | 2.314 (1.481; 3.617) | <0.001 |
| Active smoking | – | 0.10 |
| Duration of symptoms | – | – |
| Acute: <1 month | 1 | – |
| Sub-acute: 1–3 months | 1.277 (0.772; 2.112) | 0.34 |
| Chronic: >3 months | 1.667 (1.115; 2.492) | 0.013 |
| Use of opioids before hospitalization | – | 0.30 |
| Nerve root pain distribution | – | 0.13 |
| Positive straight leg-raising test | – | 0.99 |
| Impulsive pain | 1.985 (1.258; 3.133) | 0.003 |
| Motor loss ⅘ | 1.728 (1.229; 2.431) | 0.002 |
| Decrease in numeric pain-scale rating between beginning and end of hospitalization | 0.921 (0.861; 0.985) | 0.017 |
| Number of epidural injections received per patient before and during hospitalization | 1.393 (1.165; 1.665) | <0.001 |
| Length of hospital stay (days) | – | 0.11 |
| IV NSAIDs | – | 0.67 |
P<0.05 considered significant. CI, confidence interval; BMI, body mass index; IV, intravenous; NSAIDs, non-steroidal anti-inflammatory drugs.
In univariate analysis, predictive factors for surgery were, in backward order, presence of a concordant herniated disc, number of epidural infiltrations, working, duration of leg-pain greater than 3 months before hospitalization, clinical signs of disco-radicular conflict (such as positive straight leg-raising test and impulsive pain), use of morphine before hospitalization, motor loss at initial clinical examination, use of intravenous (IV) NSAIDs during hospitalization, and longer hospital stay (Table 2). Conversely, certain factors—such as higher body mass index (BMI) and a decrease in pain following hospitalization—were associated with a lower occurrence of surgery.
In multivariate analysis, we found that working, impulsive pain (coughing, defecation), motor loss, duration of pain greater than 3 months, and higher number of epidural injections were significantly associated with the occurrence of surgery (Table 3). Surgery was less frequent in patients in whom a decrease in numeric pain-scale rating was observed between the beginning and the end of the hospitalization.
Discussion
One of the key findings of this study is that a relatively low proportion (one-third) of patients hospitalized for sciatica due to discal herniation required surgery at one year, which underscores the interest of our medical management protocol. This finding also seems to be consistent with the findings reported in the few previous studies carried out with the same objective.
Indeed, 34.8% of our patients underwent surgery within a year of hospitalization. This finding is comparable to that reported by Valls et al. (17)., where 35.1% of their patients underwent surgery one year after hospitalization, as well as to findings reported in older studies (18-20), where the proportion was 28% to 32%. In a study conducted by Berthelot et al., the authors reported that 13% of their patients underwent surgery following hospitalization in a rheumatology department. However, in that study, the authors focused only on surgery immediately following hospitalization (20). In fact, that finding is quite consistent with our data, which showed a median time to surgery of 31 days.
At a time when institutions are questioning the relevance of maintaining hospital beds in rheumatology departments, our study underscores the benefit of doing so, since two thirds of our patients—in many of whom out-hospital management had failed—recovered and did not need to undergo surgery as a result of their being hospitalized in our rheumatology department.
Our surgery rate may seem high, but it should be interpreted in light of the fact that it was determined in patients who had been hospitalized and does not reflect all disc-herniated sciatica cases, especially those seen in an out-patient setting.
Indeed, as our pre-hospitalization care data shows, medical care had already failed for many patients hospitalized in our department: 52.5% of the patients had already received NSAIDs, 13% corticosteroid therapy, 22.5% opioids and 27% infiltration.
Regarding the median time to surgery of 31 days, this should be interpreted in light of the proportion of patients who had been exhibiting symptoms for more than 3 months before hospitalization. In addition, as previously mentioned, our study was carried out in a University Hospital Center, which is a tertiary center.
We did not find an association between gender or age and surgery, which is consistent with the findings of previous studies (6,10,17,21-28).
However, we did find a statistically significant association between BMI and lower occurrence of surgery in univariate analysis. This finding differs from previous studies evaluating the impact of obesity on radical treatment (23,28). On the other hand, in those studies, there were fewer patients and the proportion of obese patients was lower. As the prevalence of obesity is increasing in France, changes may have occurred in the knowledge and management of obese patients with sciatica.
Another explanation could be that the functional prognosis for herniated disc surgery among obese patients is less favorable. This was demonstrated by Weinstein et al. in the SPORT trial (6), but also in several other studies, which report less satisfaction and less improvement in perceived quality of life (29-31). In addition, the frequency of reoperation tends to be higher in obese patients (32), who are also at higher risk of postoperative complications (33).
Likewise, we observed that patients with a higher Charlson Comorbidity Index underwent less surgery, which also seems to be related to a different risk-benefit ratio, which is probably due to the increase in anesthetic risk and complications among older patients and/or patients with more co-morbidities (33-37). In the observational cohort in the SPORT trial (6), the findings were not consistent with ours, but in that study, the “comorbidities” parameter was not the Charlson index and included conditions such as anxiety or migraine, which could explain the differences between our findings and those reported by the authors of that study.
We found that active smoking increased the risk of surgery. As this finding has not been reported by other authors (10,23,26), it should be interpreted with caution. It is nevertheless surprising because a few studies have reported less favorable outcomes for pain symptoms and functional impairment following lumbar spine surgery in patients who smoke (38-40). To understand this finding, we wondered whether it might be associated with the difficulty in observing the relative rest that is recommended in the medical management of lumbosciatica, and with the involvement of inflammatory discoradicular phenomena, promoted by active smoking. We also hypothesized that the sensation of pain would be greater among smokers, especially since it has been shown that there is a higher proportion of smokers in patients with chronic pain (41). However, these explanations should be treated with caution, since smoking was not associated with surgery in the multivariate analysis.
Like Deshayes et al. (42), we found that working influenced the surgical management decision, since professionally active patients, regardless of their activity, were more likely to receive radical treatment. We found that this factor had the highest weight in multivariate analysis [odds ratio (OR) 2.314, 95% CI: 1.481; 3.617]—in which we took into account the Charlson score, which included age and comorbidities, which could be confounding factors—and this could be explained by the fact that professionally active patients are younger and have fewer comorbidities. We can assume that because recovery is faster with surgery, these patients would choose this option more often so that they could resume work more quickly.
We also found that the presence of clinical signs of discoradicular conflict—such as impulsive pain and a positive straight leg-raising test—were more often observed in patients who subsequently underwent surgery. Other authors have also reported a statistically significant association between a positive straight leg-raising test and surgery (6,17,43). However, the presence of clinical signs of discoradicular conflict is an argument in favor of the discal origin of lumbosciatica and of the indication for surgery, and therefore might be confounding factors.
A motor deficit rated at 4/5 was predictive of surgery. This finding was not reported by Valls et al. (17), but their results were equivocal since paresis was found in 18.6% of operated patients as opposed to only 8.7% of non-operated patients, with P=0.13. As our study included more patients—and perhaps was more powerful—we were able to conclude that this parameter was significant.
Regarding infiltrative management, our objective was not to determine the effectiveness of epidural infiltrations. The statistically significant association we found between the number of infiltrations and surgery, or between IV NSAIDs and surgery, is more likely a reflection of the severity of the patients’ symptoms, which ultimately justified surgical management.
We also found a statistically significant association between a decrease in numeric pain-scale rating at the end versus the beginning of hospitalization and less surgery, which seems to suggest that patients who experience the most relief further to medical management undergo less surgery. This finding was also highlighted in the SPORT trial (6), where patients with lower numeric pain-scale ratings after medical treatment had less cross-over to surgery. It has also been shown in the literature that when infiltrative management allows for a favorable evolution of pain symptoms, patients resort less to surgery (17,23).
The main limitation of our study lies in its retrospective nature, which led to missing data.
Moreover, since it was a single-center study, carried out in a university (i.e., tertiary) center, a recruitment bias, which could limit the extrapolation of our results, cannot be ruled out.
The main strengths of our study are the large number of patients that were included, and the fact that a thorough assessment was obtained for all patients, which enabled us to analyze relevant factors associated with the use of surgery.
In our study, a third of the patients underwent surgery within one year of hospitalization. This rate is rather a low and underscores the interest of hospitalizing these patients in a rheumatology department. However, this rate was determined in a population that was hospitalized in a university (i.e., tertiary) center and does not reflect all cases of lumbosciatica, and in particular ambulatory cases.
Predictive factors of subsequent surgery were highlighted, in particular working, having pain for more than 3 months before the hospitalization, and having a motor deficit of 4/5. We also demonstrated that patients who failed to experience pain relief through medical care during hospitalization, and who did not experience less pain at the end than at the beginning of hospitalization, were more likely to undergo surgery.
These identified factors could orient patients with severe lumbosciatica more towards surgical management, since, as Fjeld’s team has shown, surgery is associated with better outcomes in severe sciatica (44).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-43/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-43/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-43/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-43/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The National Commission for Data Processing and Liberties approved the study and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jensen RK, Kongsted A, Kjaer P, et al. Diagnosis and treatment of sciatica. BMJ 2019;367:l6273. [Crossref] [PubMed]
- Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976) 2008;33:2464-72. [Crossref] [PubMed]
- Konstantinou K, Dunn KM, Ogollah R, et al. Prognosis of sciatica and back-related leg pain in primary care: the ATLAS cohort. Spine J 2018;18:1030-40. [Crossref] [PubMed]
- Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 2007;356:2245-56. [Crossref] [PubMed]
- Lequin MB, Verbaan D, Jacobs WC, et al. Surgery versus prolonged conservative treatment for sciatica: 5-year results of a randomised controlled trial. BMJ Open 2013;3:002534. [Crossref] [PubMed]
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 2006;296:2441-50. [Crossref] [PubMed]
- Osterman H, Seitsalo S, Karppinen J, et al. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine (Phila Pa 1976) 2006;31:2409-14. [Crossref] [PubMed]
- Gugliotta M, da Costa BR, Dabis E, et al. Surgical versus conservative treatment for lumbar disc herniation: a prospective cohort study. BMJ Open 2016;6:e012938. [Crossref] [PubMed]
- Bailey CS, Rasoulinejad P, Taylor D, et al. Surgery versus Conservative Care for Persistent Sciatica Lasting 4 to 12 Months. N Engl J Med 2020;382:1093-102. [Crossref] [PubMed]
- Peul WC, van den Hout WB, Brand R, et al. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ 2008;336:1355-8. [Crossref] [PubMed]
- Jacobs WC, van Tulder M, Arts M, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 2011;20:513-22. [Crossref] [PubMed]
- Fernandez M, Ferreira ML, Refshauge KM, et al. Surgery or physical activity in the management of sciatica: a systematic review and meta-analysis. Eur Spine J 2016;25:3495-512. [Crossref] [PubMed]
- Rothoerl RD, Woertgen C, Brawanski A. When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev 2002;25:162-5. [Crossref] [PubMed]
- Rihn JA, Hilibrand AS, Radcliff K, et al. Duration of symptoms resulting from lumbar disc herniation: effect on treatment outcomes: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 2011;93:1906-14. [Crossref] [PubMed]
- Van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software 2011;45:1-67. [Crossref]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley and Sons, 1987.
- Valls I, Saraux A, Goupille P, et al. Factors predicting radical treatment after in-hospital conservative management of disk-related sciatica. Joint Bone Spine 2001;68:50-8. [Crossref] [PubMed]
- Delauche-Cavallier MC, Budet C, Laredo JD, et al. Lumbar disc herniation. Computed tomography scan changes after conservative treatment of nerve root compression. Spine (Phila Pa 1976) 1992;17:927-33. [Crossref] [PubMed]
- Abanco J, Ros E, Llorens J, et al. Infiltrations épidurales dans le traitement de la radiculopathie lombaire. À propos de 200 cas. Rev Chir Orthop 1994;80:689-93. [PubMed]
- Berthelot JM, Rodet D, Guillot P, et al. Is it possible to predict the efficacy at discharge of inhospital rheumatology department management of disk-related sciatica? A study in 150 patients. Rev Rhum Engl Ed 1999;66:207-13. [PubMed]
- Haugen AJ, Brox JI, Grøvle L, et al. Prognostic factors for non-success in patients with sciatica and disc herniation. BMC Musculoskelet Disord 2012;13:183. [Crossref] [PubMed]
- El Barzouhi A, Verwoerd AJ, Peul WC, et al. Prognostic value of magnetic resonance imaging findings in patients with sciatica. J Neurosurg Spine 2016;24:978-85. [Crossref] [PubMed]
- Sutheerayongprasert C, Paiboonsirijit S, Kuansongtham V, et al. Factors predicting failure of conservative treatment in lumbar-disc herniation. J Med Assoc Thai 2012;95:674-80. [PubMed]
- Vignon G, Site J, Meunier P, et al. Enquête statistique par ordinateur sur le traitement chirurgical de la névralgie sciatique discale. Rev Rhum Mal Ostéoartic 1970;37:465-75. [PubMed]
- Cheng F, You J, Rampersaud YR. Relationship between spinal magnetic resonance imaging findings and candidacy for spinal surgery. Can Fam Physician 2010;56:e323-30. [PubMed]
- Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am 2004;86:670-9. [Crossref] [PubMed]
- el Barzouhi A, Vleggeert-Lankamp CL. Predictive value of MRI in decision making for disc surgery for sciatica. J Neurosurg Spine 2013;19:678-87. [Crossref] [PubMed]
- Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 1983;8:131-40. [Crossref] [PubMed]
- Macki M, Alvi MA, Kerezoudis P, et al. Predictors of patient dissatisfaction at 1 and 2 years after lumbar surgery. J Neurosurg Spine 2019; Epub ahead of print. [Crossref] [PubMed]
- Park C, Garcia AN, Cook C, et al. Long-term impact of obesity on patient-reported outcomes and patient satisfaction after lumbar spine surgery: an observational study. J Neurosurg Spine 2020; Epub ahead of print. [Crossref] [PubMed]
- Sielatycki JA, Chotai S, Stonko D, et al. Is obesity associated with worse patient-reported outcomes following lumbar surgery for degenerative conditions? Eur Spine J 2016;25:1627-33. [Crossref] [PubMed]
- Walid MS, Zaytseva N. History of spine surgery in older obese patients. Ger Med Sci 2011;9:Doc05. [PubMed]
- Sivaganesan A, Zuckerman S, Khan I, et al. Predictive Model for Medical and Surgical Readmissions Following Elective Lumbar Spine Surgery: A National Study of 33,674 Patients. Spine (Phila Pa 1976) 2019;44:588-600. [Crossref] [PubMed]
- Saleh A, Thirukumaran C, Mesfin A, et al. Complications and readmission after lumbar spine surgery in elderly patients: an analysis of 2,320 patients. Spine J 2017;17:1106-12. [Crossref] [PubMed]
- Lakomkin N, Kothari P, Dodd AC, et al. Higher Charlson Comorbidity Index Scores Are Associated With Increased Hospital Length of Stay After Lower Extremity Orthopaedic Trauma. J Orthop Trauma 2017;31:21-6. [Crossref] [PubMed]
- Sukhonthamarn K, Grosso MJ, Sherman MB, et al. Risk Factors for Unplanned Admission to the Intensive Care Unit After Elective Total Joint Arthroplasty. J Arthroplasty 2020;35:1937-40. [Crossref] [PubMed]
- Ogura K, Yasunaga H, Horiguchi H, et al. What is the effect of advanced age and comorbidity on postoperative morbidity and mortality after musculoskeletal tumor surgery? Clin Orthop Relat Res 2014;472:3971-8. [Crossref] [PubMed]
- Pearson A, Lurie J, Tosteson T, et al. Who should have surgery for spinal stenosis? Treatment effect predictors in SPORT. Spine (Phila Pa 1976) 2012;37:1791-802. [Crossref] [PubMed]
- Sandén B, Försth P, Michaëlsson K. Smokers show less improvement than nonsmokers two years after surgery for lumbar spinal stenosis: a study of 4555 patients from the Swedish spine register. Spine (Phila Pa 1976) 2011;36:1059-64. [Crossref] [PubMed]
- Seicean A, Seicean S, Alan N, et al. Effect of smoking on the perioperative outcomes of patients who undergo elective spine surgery. Spine (Phila Pa 1976) 2013;38:1294-302. [Crossref] [PubMed]
- Orhurhu VJ, Pittelkow TP, Hooten WM. Prevalence of smoking in adults with chronic pain. Tob Induc Dis 2015;13:17. [Crossref] [PubMed]
- Deshayes P, Baron JJ, Le Loët X. Résultat du traitement médical en milieu hospitalier des sciatiques d’origine discale. Rev Rhum Mal Ostéoartic 1981;48:563-8. [PubMed]
- White AP, Harrop J, Dettori JR. Can clinical and radiological findings predict surgery for lumbar disc herniation? A systematic literature review. Evid Based Spine Care J 2012;3:45-52. [Crossref] [PubMed]
- Fjeld O, Grotle M, Siewers V, et al. Prognostic Factors for Persistent Leg-Pain in Patients Hospitalized With Acute Sciatica. Spine (Phila Pa 1976) 2017;42:E272-9. [Crossref] [PubMed]


