
Etiologies, incidence, and demographics of lumbar vertebral fractures in U.S. emergency departments
Introduction
Vertebral fractures are common injuries that affect diverse patient populations with the majority of these fractures involving the thoracolumbar junction and lumbar spine (1-3). Lumbar vertebral fractures have been shown to be debilitating injuries that can be associated with spinal deformity, disability, pain, and neurological deficit (4-7). While fractures of the lumbar spine are less likely to result in severe neurological deficit compared to those involving the cervical or thoracic spine, lumbar injuries can sometimes compromise the cauda equina nerve roots or the conus medullaris. In fact, neurologic deficits were reported in 25–60% of patients with lumbar fractures depending on fracture classification (4,5). Whereas many lumbar vertebral fractures have the potential to heal with non-operative management, surgical interventions including spinal fusion, kyphoplasty, and vertebroplasty are commonly performed to address neurologic deficits, provide stability to the spinal column, and improve functional outcomes (8,9).
Beyond the immediate and long-term impact on patients, vertebral fractures lead to significant healthcare costs and further stress the healthcare system. A cross-sectional study found that approximately 1.4 million patients sustain vertebral compression fractures every year with an annual inpatient cost just under $5 billion (10). Given the large clinical and economic impacts of lumbar vertebral fractures on patients and society, a deeper understanding of their incidence and etiologies is warranted. Improvement in understanding, may help clinicians optimize strategies for both prevention as well as treatment (11).
While the common etiologies of cervical fractures have been explored in the literature (12), investigations that detail the etiologies of lumbar vertebral fractures remain lacking. However, there is yet to be a national investigation encompassing the multitude of lumbar vertebral fractures by injury to date. Therefore, in this study, we examine the incidence, demographics and etiologies of lumbar vertebral fracture injuries in the United States (U.S.) from 2010 to 2018. We present the following article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-21-110/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This cross-sectional epidemiological study utilized cases of lumbar fractures in the U.S. Consumer Product Safety Commission’s (CPSC) National Electronic Injury Surveillance System (NEISS) database. The NEISS repository uses collected product-related injury data to create a complex probability survey that estimates nationwide injuries in all U.S. emergency departments. The NEISS sample includes 102 hospitals that were originally designated by stratified, randomized sampling of all 5,200 U.S. hospitals with an emergency department. Stratification was based on both geographic location and annual emergency department volume data. Data was gathered on all patients present in the 102 sample emergency departments between 2010–2018 with each datapoint assigned a national estimate weight (13).
A search to isolate injuries categorized as fractures (NEISS code: 57) located at the lower trunk (NEISS code: 79) was performed. The narrative associated with each injury was individually evaluated for inclusion and exclusion criteria. In the search, specific inclusion criteria included entries with the terms: “Lumba”, “Lumb”, “Ls spine”, “L-spine”, “L1”, “L2”, “L3”, “L4”, “L5”, “Lumbar”, “Low Back”, “Lower Back”, and “Lwr back”. With use of the free text narrative section of the database, each injury was analyzed individually to exclude fractures of the pelvic and hip regions. As past literature has shown that lumbar fractures primarily affect elder populations and that pediatric fracture etiologies differ significantly from adult fracture etiologies, this study examined non-pediatric patients and excluded patients 18 years of age and younger from the sample (14). There were insignificant pediatric cases and excluding these samples effectively removed statistical noise for the calculations. Given these parameters, available sample NEISS data was generated for years 2010 through 2018.
Statistical analysis
Sample data provided information regarding cause of injury (product code), sex, age, and a free text narrative history. From the sample, the national frequency of lumbar vertebral fractures was estimated per year and in aggregate. National estimates were then calculated as the sum of the provided NEISS weights by year, since this weight was directly representative of the population. In order to calculate the 95% confidence interval (CI) about the national estimate, verified algorithms provided by NEISS were used (13): first, variances of estimates were calculated from excel; next, the coefficients of variation (CV) were calculated as the root of the variances divided by their respective national estimate; finally, the 95% CIs around the estimate was calculated as the product of the national estimate, the CV, and a z-score of 1.96. Hence, all estimates calculated took into account relative variability of weighing the NEISS sample to the national U.S. population by using the respective CV. These national estimates of fracture were stratified by sex and age distribution. Population estimates by age (18+) were obtained from annual U.S. Census estimates and used to calculate annual incidence rates of lumbar fractures per 100,000 people.
As a trend analysis, mean age of injury was calculated for each individual year as well as for the overall time frame studied. This calculation was taken as a weighted average of sample patients’ national weights and ages and stratified by year. The annual national estimates of the three leading causes of fracture were calculated by indexing the most frequent product codes in the sample data. Finally, linear regression and ANOVA were utilized to further understand and visualize the relationship between the etiologies of fracture and demographic distribution.
Results
Between 2010 to 2018, 8,377 sample lumbar vertebral fractures were isolated from the search criteria in the NEISS repository. Utilizing the verified algorithm from NEISS to determine the national estimates across the U.S., it was approximated that there have been 382,914 (95% CI: 382,855–382,973) lumbar vertebral fractures in the U.S. population (Table 1). Females constituted the majority of fractures at 59.8% (223,865 fractures, 95% CI: 223,323–224,407) and males constituted 40.2% (154,049 fractures, 95% CI: 153,679–154,419) (Table 2).
Table 1
| Year | National estimate of cases (95% CI) | Standard error |
|---|---|---|
| 2010 | 34,327.5±50.7 | 50.7 |
| 2011 | 33,178.0±49.4 | 49.4 |
| 2012 | 34,880.6±55.6 | 55.6 |
| 2013 | 35,781.3±59.0 | 59.0 |
| 2014 | 37,889.9±63.6 | 63.6 |
| 2015 | 46,963.9±66.0 | 66.0 |
| 2016 | 46,125.2±66.4 | 66.4 |
| 2017 | 56,668.7±57.2 | 57.2 |
| 2018 | 57,098.2±54.2 | 54.2 |
| 2010–2018 | 382,913.3±58.9 | 58.9 |
The table illustrates the increasing lumbar vertebral fracture admissions to the emergency department by year. CI, confidence interval.
Table 2
| Items | Value |
|---|---|
| National estimate of cases | |
| Male | 154,049±370.2 |
| Female | 223,865±542.4 |
| Fraction of patients | |
| Male | 40.20% |
| Female | 59.80% |
The table illustrates greater female lumbar fractures than male in U.S. emergency departments.
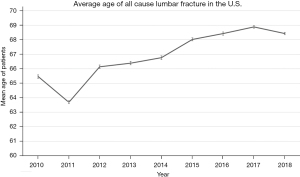
For all lumbar fracture etiologies, the mean age was 67.2 years between 2010 and 2018, supporting past literature that lumbar fractures primarily target adult and elder populations (14). From 2010 to 2018, the mean age of patients sustaining lumbar fracture increased by 2.96 years from 65.5 (95% CI: 65.38–65.62) years in 2010 to 68.4 (95% CI: 68.32–68.48) years in 2018, a 4.5% increase (Figure 1). In addition, the average age for floor related injuries was 77.1 years, for stair/step injuries was 59.8 years, and for ladder injuries was 56.7 years.
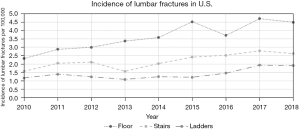
The annual incidence rate (per 100,000) of total lumbar fractures in the U.S. increased by 54%, from 14.6 to 22.5 per 100,000 people from 2010 to 2018. Similarly, lumbar fracture incidence rates due to falls onto the floor from standing increased from 2.3 to 4.5 (92% increase), fractures due to falls down stairs increased from 1.6 to 2.6 (63% increase), and fractures due to falls off ladders increased from 1.2 to 1.9 (58% increase) (Figure 2).
The number of all-cause annual lumbar vertebral fractures increased by 66.3% from 34,328 (95% CI: 34,277–34,379) in 2010 to 57,098 (95% CI: 57,044–57,152) in 2018. Most notably, the largest relative annual increase in fractures was observed between 2014 and 2015 where a 23.9% increase was seen from 37,890 (95% CI: 37,826–37,954) in 2014 to 46,964 (95% CI: 46,898–47,030) in 2015. From 2010 to 2018 the total amount of lumbar fractures increased each year with the exception of 2010 to 2011 and 2015 to 2016 where slight declines were noted (Table 3).
Table 3
| Year | Total | Floor | Stairs/steps | Ladders |
|---|---|---|---|---|
| 2010 | 34,328 | 5,482 | 3,690 | 2,752 |
| 2011 | 33,178 | 6,840 | 4,860 | 3,308 |
| 2012 | 34,881 | 7,199 | 5,066 | 2,971 |
| 2013 | 35,781 | 8,164 | 3,795 | 2,632 |
| 2014 | 37,890 | 8,761 | 4,964 | 3,048 |
| 2015 | 46,964 | 11,146 | 5,962 | 2,995 |
| 2016 | 46,125 | 9,241 | 6,274 | 3,635 |
| 2017 | 56,669 | 11,839 | 7,013 | 4,875 |
| 2018 | 57,098 | 11,381 | 6,650 | 4,836 |
| Sum | 382,913 | 80,054 | 48,274 | 31,053 |
This table illustrates fractures are increasingly driven by injuries of floors, steps, and ladders.
Throughout the study period floors, stairs/steps, and ladders remained the three main mechanisms of injury for lumbar vertebral fracture. Based on review of the free text narrative depicting the mechanism of injury, it was seen that these top three etiologies of fracture were all fall related. Across the nine-year time frame, the estimated sum of floor-related fractures was 80,054 (95% CI: 79,986–80,122), stair/step-related fractures was 48,274 (95% CI: 48,209–48,339), and ladder-related fractures was 31,053 (95% CI: 30,987–31,119) (Table 3). Floor-related injuries accounted for 20.9%, stair-related injuries for 12.6%, and ladder-related injuries for 8.1% of total lumbar fractures. At the national level, these three etiologies constituted 41.6% of all lumbar fractures. The figure below illustrates the growing prevalence of lumbar fractures from these three injuries and clearly depicts floors as the main mechanism of injury each year while consistently being followed by stairs/steps and ladders (Table 3). The categories of products that comprised the remaining 58.4% lumbar fractures were attributed to bedroom, sports, building/venting, bathroom, personal items, outdoors/agriculture/construction, powered vehicles, kitchen, and toys (Table 4). The exclusive categories of injuries in Table 4 were developed in accordance with the NEISS Coding Manual, which excludes motor vehicles and physical human interactions as sources of injury.
Table 4
| Category | Cases | Relative, % |
|---|---|---|
| Stairs/steps, floors, ladders | 159,381 | 41.62 |
| Bedroom | 83,048 | 21.69 |
| Sports | 33,714 | 8.80 |
| Building/venting | 30,776 | 8.04 |
| Bathroom | 24,483 | 6.39 |
| Personal items | 16,237 | 4.24 |
| Outdoors/agriculture/construction | 16,187 | 4.23 |
| Powered vehicles | 14,186 | 3.70 |
| Kitchen | 3,214 | 0.84 |
| Toys/children products | 1,687 | 0.44 |
This table illustrates fracture cases and relative percentage by exclusive categories of injuries with the top 3 injuries grouped into one category.
Linear regression performed to understand the relationship between etiology and demographic distribution found that there was a strong [(>0.95) R2=0.97] correlation coefficient between these variables, indicating a relationship among etiology, age, and increasing national estimates of lumbar fracture. Analysis of variance demonstrated that the average age and the incidence of ladder-related cases have had the most statistically significant correlation to the increase in total lumbar fractures between 2010 to 2018 (P value =0.0002). The other recurrent etiologies, floors (P value =0.17) and stairs (with P value =0.74), had a statistically insignificant impact on the increase lumbar fractures between 2010 and 2018.
Discussion
There is a paucity of literature on the epidemiology of lumbar fractures, with more efforts within the U.S. addressing the epidemiology of spinal cord injury (15). The objective of this study was to investigate the frequency, population distribution, and leading causes of lumbar vertebral fracture injuries in the U.S. from 2010 to 2018. The study successfully identified the national volume of lumbar vertebral fractures from NEISS and analyzed demographic trends observed in these data. The data showed a 66.3% increase in total lumbar vertebral fractures that presented to U.S. emergency departments between 2010 and 2018.
We found that increasing mean age was highly associated with an increase in annual number of lumbar vertebral fractures. Similar to studies conducted in other countries, this is likely due to the fact that the U.S. population is aging (11,16). It is therefore reasonable to suggest that the aging population is a likely cause of the increase in number of annual vertebral fractures. Age is a strong risk factor for both osteoporosis and decreased bone density, both of which can predispose patients to fracture (17). Previous studies cite osteoporosis as the second highest comorbidity associated with lumbar vertebral fractures, with more than 700,000 of all vertebral fractures annually within elderly populations attributed to osteoporosis (11,18). Patient of older age treated for lumbar vertebral fractures are at higher risk for nonroutine discharge, medical complications, and adverse reactions following surgical treatment, highlighting the significant of recognizing this at-risk population and instituting preventative measures (11).
Furthermore, we found that adult women sustained a greater proportion of lumbar fractures (59.8%) than adult men in the U.S. women are at higher risk of developing osteoporosis and have lower bone density compared to men (19). This may help explain the observed data that more women sustained vertebral lumbar fractures than men within the study population. Although the data did not support a statistically significant correlation between sex and fracture frequency, this distribution suggests women sustain more fractures than men.
The three most common etiologies of lumbar vertebral fracture between 2010 and 2018 were falls from standing onto floors (20.9%), falls involving stairs/steps (12.6%), and falls involving ladders (8.1%). While it remains unclear the extent to which these fractures are caused by increasing patient proclivity for falls (e.g., increasing frequency of falls) versus patient susceptibility to falls (e.g., increasing frailty) versus inherently faulty floors, stairs, and ladders our study would suggest that future preventative measure should address all these possibilities. Clinicians should identify patients at high risk of falls (such as those with balance problems) and patients at high risk of injury following falls (such as those with osteoporosis) and educate them and their families about safety measures to prevent falls. Furthermore, environmental factors that could increase risks of fall such as unsafe stairs or ladders should be addressed. By understanding the etiology and demographic distribution of lumbar vertebral fractures, preventative health measures can be allocated accordingly and become more targeted to result in the greatest impact of decreased morbidity and healthcare costs. The data also serves as a key reference for common mechanisms of injury for physicians in their recommendations to patients to prevent lumbar vertebral fractures. Specifically, since the data has identified that falls involving floors, stairs/steps and ladders are responsible for 41.6% of all lumbar vertebral fractures between 2010 and 2018, physicians and other advanced providers can be more precise in where they stress caution to their patients. Such interventions could prevent injuries and thereby decrease healthcare costs. Future cost-effectiveness and health economics studies should reveal the effect these preventative interventions could have on clinical outcomes and economic costs related to vertebral fracture care.
The results of this investigation should be viewed within the context of its limitations, specifically its retrospective design. The quality of the data, and by extension the study, depends entirely on the CPSC NEISS medical database as well as the accuracy of the initial text narrative search. While this database captures lumbar vertebral fractures that present to the emergency departments, it may underestimate the true incidence of fractures. A portion of lumbar vertebral fractures may present to the clinic or urgent care centers and not the emergency department. Additionally, some lumbar vertebral fractures that present to emergency rooms may not be captured if it doesn’t meet all inclusion/exclusion criteria of the NEISS database. For example, fractures presenting to the emergency department but not associated with an NEISS consumer product would not be captured, such as trauma from motor vehicle collision or human interaction. Another limitation of the study is that we assumed the data to be normally distributed in order to calculate relative variance and CV by the central limit theorem. This may discount inherent skew/bias in the data.
Future research can use our NEISS estimation process for related fractures and injuries in order to highlight other U.S. population health trends. This investigation provided a preliminary national estimate of adult lumbar fractures through a straightforward and reproducible methodology. Future studies should delve further into national trends regarding outcomes of lumbar fractures and the associated patient morbidity and economic burden. Categorizing these injuries as being operable, inoperable, or treatable with conservative measures will better inform physicians of the economic impacts of increased lumbar fractures. Such categorization could provide improved prevention, diagnosis and treatment of older patients, who are most affected in lumbar fracture cases (11). The rising incidence of lumbar fractures may then underlay the noted rise of operative procedures in spinal care (20). Future studies should additionally map the risk factors associated with specific etiologies of fracture for more accurate and reliable prognostic information.
Conclusions
The volume of lumbar vertebral fracture has increased over the last near decade (66.3%), and approximately half (48%) of these fractures result from falls to the floor from standing, falls on the stairs/steps, and ladder-related falls. The increasing mean patient age, as well as accidents involving ladders, were found to be statistically correlated with the rise in total lumbar fracture volume over the time period studied. Clinicians should target preventative educational measures to population groups at high risk of falls and at high risk of injury following falls, such as the elderly. Environmental and technical factors that further increase risk of injury such as hazardous steps or unsafe ladder use should be addressed as well. These interventions could help reduce, or at least slow down, the increasing rate of lumbar vertebral fractures in the U.S.
Acknowledgments
The abstract of this publication was published as an e-poster in The Spine Journal.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-21-110/rc
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-21-110/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-21-110/coif). CS received consulting fees from Nuvasive, received payment for expert testimony from RxPro Services, received support for attending meetings from Medtronic and Nuvasive, and has stock shares in Vertera LLC, AlphaTec, Huxley. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Camacho JE, Usmani MF, Strickland AR, et al. The use of minimally invasive surgery in spine trauma: a review of concepts. J Spine Surg 2019;5:S91-100. [Crossref] [PubMed]
- Holmes JF, Miller PQ, Panacek EA, et al. Epidemiology of thoracolumbar spine injury in blunt trauma. Acad Emerg Med 2001;8:866-72. [Crossref] [PubMed]
- Francis RM, Baillie SP, Chuck AJ, et al. Acute and long-term management of patients with vertebral fractures. QJM 2004;97:63-74. [Crossref] [PubMed]
- Mohanty SP, Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise? Spinal Cord 2002;40:295-9. [Crossref] [PubMed]
- Laghmouche N, Prost S, Farah K, et al. Minimally invasive treatment of thoracolumbar flexion-distraction fracture. Orthop Traumatol Surg Res 2019;105:347-50. [Crossref] [PubMed]
- Hansson E, Hansson T. The cost-utility of lumbar disc herniation surgery. Eur Spine J 2007;16:329-37. [Crossref] [PubMed]
- Suzuki N, Ogikubo O, Hansson T. The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months. Eur Spine J 2008;17:1380-90. [Crossref] [PubMed]
- Baaj AA, Downes K, Vaccaro AR, et al. Trends in the treatment of lumbar spine fractures in the United States: a socioeconomics perspective: clinical article. J Neurosurg Spine 2011;15:367-70. [Crossref] [PubMed]
- Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: An overview. Indian J Orthop 2015;49:72-82. [Crossref] [PubMed]
- Joish VN, Brixner DI. Back pain and productivity: measuring worker productivity from an employer's perspective. J Pain Palliat Care Pharmacother 2004;18:79-85. [Crossref] [PubMed]
- Drazin D, Nuno M, Shweikeh F, et al. Outcomes and National Trends for the Surgical Treatment of Lumbar Spine Trauma. Biomed Res Int 2016;2016:3623875. [Crossref] [PubMed]
- Lomoschitz FM, Blackmore CC, Mirza SK, et al. Cervical spine injuries in patients 65 years old and older: epidemiologic analysis regarding the effects of age and injury mechanism on distribution, type, and stability of injuries. AJR Am J Roentgenol 2002;178:573-7. [Crossref] [PubMed]
- U.S. Consumer Product Safety Commission. National electronic injury surveillance system (NEISS). Available online: https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data
- Waterloo S, Ahmed LA, Center JR, et al. Prevalence of vertebral fractures in women and men in the population-based Tromsø Study. BMC Musculoskelet Disord 2012;13:3. [Crossref] [PubMed]
- Schoenfeld AJ, McCriskin B, Hsiao M, et al. Incidence and epidemiology of spinal cord injury within a closed American population: the United States military (2000-2009). Spinal Cord 2011;49:874-9. [Crossref] [PubMed]
- Chmielnicki M, Prokop A, Kandziora F, et al. Surgical and Non-surgical Treatment of Vertebral Fractures in Elderly. Z Orthop Unfall 2019;157:654-67. [Crossref] [PubMed]
- Pietschmann P, Rauner M, Sipos W, et al. Osteoporosis: an age-related and gender-specific disease--a mini-review. Gerontology 2009;55:3-12. [Crossref] [PubMed]
- Cooper C, Atkinson EJ, O'Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 1992;7:221-7. [Crossref] [PubMed]
- Alswat KA. Gender Disparities in Osteoporosis. J Clin Med Res 2017;9:382-7. [Crossref] [PubMed]
- Ponkilainen VT, Toivonen L, Niemi S, et al. Incidence of Spine Fracture Hospitalization and Surgery in Finland in 1998-2017. Spine (Phila Pa 1976) 2020;45:459-64. [Crossref] [PubMed]


