
Validation of a novel range of motion assessment tool for the cervical spine: the HALO© digital goniometer
Introduction
Range of motion (ROM) assessment forms a critical component of the objective evaluation of patients in pre- and post-spinal surgeries (e.g., cervical and lumbar fusion and disc replacement surgeries), with a high degree of correlation with quality of life outcomes (1). Quantitative outcome assessments in neurosurgical and orthopaedic settings, with the notable exception of assessments such as the 6-minute walk test (6MWT), are lacking (2-4). Radiography is the accepted gold standard for cervical ROM measurement; however, it comes with the caveat of radiation exposure, increased time-to-assessment, and is most useful in flexion/extension, whilst not so much in the evaluation of cervical rotation. Additional tools commonly used to assess cervical ROM include visual estimation (5,6), tape measurement (7,8), inclinometers (9) and the universal goniometer (UG) (7).
The advent of novel ROM assessment technology, such as digital goniometer (DG), presents an avenue for research and potential application within clinical and surgical settings, given its ease of use, speed, and potential for increased accuracy of measurement. Indeed, if a digital tool proved more accurate, faster, and more user-friendly, it would represent a more viable tool than the oft-used UG in clinical settings, where high-volume batteries of assessment can lead to reduced precision and user fatigue. However, no previous study has been found to test the reliability of the DG in cervical ROM measurement. The aim of the present study was therefore to evaluate the DG in terms of validity, intra- and inter-rater reliability of the cervical spine. We present the following article in accordance with the MDAR reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-21-92/rc).
Methods
Ethics approval, inclusion and exclusion criteria
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). After approval by the Local Health District Ethics Committee and upon attaining verbal and/or written informed consent, 100 healthy subjects from the local university (The University of New South Wales) were recruited for the study. Sample size was chosen based on relevant validation studies (10). Sample calculations based on the results of a previous study evaluating passive hip ROM showed that a minimum sample size of n=50 is required to detect an effect size of 0.1 with a type 1 error rate (α) =0.05% and power (1-β) =0.8 (10). To be eligible for inclusion, subjects must have been over the age of 18 and have no current cervical spine injuries at the time of assessment. Subjects were excluded if they had any injury that had been managed surgically—irrespective of the time since management—if they had movement-restricting pain, or if they were unable to provide informed consent for the assessment.
Acquisition systems—the UG and the DG
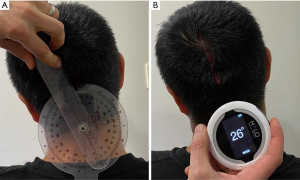
The UG is an instrument that measures joint ROM around a central axis of rotation in one-degree increments (see Figure 1A). A stationary arm provides a reference point for another motion arm that follows the joint or limb being assessed. The HALO© DG (model HG1, HALO Medical Devices, Sydney, Australia) is a digital ROM assessment tool that employs a laser-guided inclinometer system in place of the traditional arms of the UG (see Figure 1B).
Raters and subjects
All subjects were coded such that no identification of individual persons could be made.
A total of 100 subjects were assessed in two separate groups of 50, by two different groups of assessors. Fifty subjects (41 males, 9 females, mean age: 20.3±1.4 years) were assessed by physiotherapists (Rater 1/2) with 10 and 3 years of clinical experience, respectively. Rater 1 had 15 hours of experience using the DG, while Rater 2 had a single 1-hour training session prior to the commencement of this study. The remaining fifty (26 males, 24 females, mean age: 20±1.1 years) assessed by two 4TH year medical students (Rater 3/4). Both Rater 3 and 4 had 10 hours of experience with the UG and DG prior to the commencement of this study, The second group were assessed at a later follow-up session by Rater 3, at a mean follow-up time of 31.3 days. Each subject was randomly allocated into one of four groups, which determined the order of the device and rater they would get assessed by. Each rater was responsible for placement of the UG or DG, providing verbal instructions to commence each motion and obtaining a final reading from the device.
ROM assessment protocol—cervical spine
All ranges of motion were carried out in accordance with the American Association of Orthopaedic Surgeons (AAOS) guidelines (11). A brief protocol is presented here. The subject was required to sit in a neutral position—spine straight, eyes forward—prior to the commencement of each ROM. From this neutral position, the subject was asked to move their chin towards their sternum (cervical flexion), look up towards the ceiling (cervical extension), bring their right ear to their right shoulder (cervical lateral flexion) and turn 90° to their right, or as far as possible (rotation). For cervical flexion/extension, the goniometers were placed over the mastoid process of the subject, with the stationary arm perpendicular to the motion arm, which was aligned with the base of the nose. For lateral flexion, the base of the goniometer was placed over C7, and both arms were aligned with the occipital prominence. For rotation, the base of the goniometer was placed over the occipital prominence and the arms were aligned with the midline of the nose. From these positions, the active movements were performed, and the motion arm of the goniometers tracked the landmark of interest (i.e., the nose and occiput). Each movement was performed, and the range was measured three times using each tool, following one practice movement to ensure the subject understood the procedure. The mean of the three measures were calculated and compared between each set of two raters to determine the inter-rater reliability.
Statistical analysis
All data analysis and statistical evaluation of ROM was carried out using IBM SPSS Statistics 25 (IBM Corporation, Armonk, NY, USA). Intra-rater reliability was evaluated using a two-way mixed-effects absolute agreement intraclass correlation coefficient model for single measures (ICC3,1). Inter-rater reliability was determined using a two-way random effects absolute agreement ICC model for single measures (ICC2,1) (12). Standard error of the mean (SEM) and Bland-Altman plots were employed to provide visualization of the results (13).
For both intra-rater and inter-rater reliability, ICCs greater than 0.90 were considered as “excellent” reliability, ICCs between 0.75 and 0.90 were considered as “good” reliability, ICCs between 0.40 and 0.75 as “modest” reliability and those less than 0.40 as “poor” reliability (12). The standard error of measurement (SEm) was calculated for both intra-rater and inter-rater reliability using the following formula:
Using Eq. [1], the minimum detectable change at the 90% confidence interval (MDC90) was calculated using the following formula:
This value is of clinical significance as it describes the minimum amount of change that needs to occur to ensure that the change is not attributable to measurement error (14). The concurrent validity of the HALO© was established using a paired samples t-test to determine if the differences in the means obtained by the two different devices assessing a single motion were statistically significant. This was further analysed through Bland-Altman plots to visualise whether the two devices produced comparable results. The 95% limits of agreements (LOA) were calculated from these plots to determine the level of agreement between the two devices.
Results
Inter- and intra-rater reliability
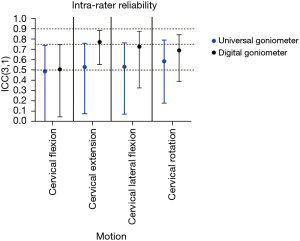
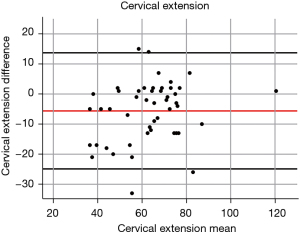
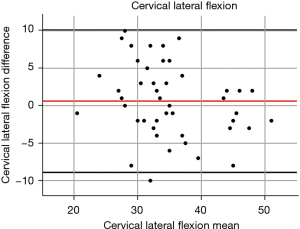
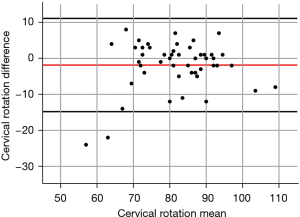
The mean and standard deviation (SD) value of the cervical ROM was summarized in the Table 1. For the reliability analyses, in the physiotherapist cohort, inter-rater reliability was highest for cervical extension for both the UG and DG, with good reliability at ICC values of 0.819 and 0.780, respectively (Table 2 and Figure 2). Reliability for cervical flexion and cervical rotation was poor with the UG, with ICCs of 0.380 and 0.255 respectively, but modest for the DG, with ICCs of 0.477 and 0.551. In the medical student cohort, the reliability of all planes of motion were modest for the UG (Table 3 and Figure 3). The reliability of all planes of motion were modest to good for the DG, with values between 0.477 and 0.831. Intra-rater reliability was modest for all ranges of motion when using UG and between modest to good with DG (Table 4 and Figure 4). In the physiotherapy cohort, cervical extension for the UG and cervical lateral flexion for the DG were the most accurate planes, with MDC90 values of 9.7 and 8.0 degrees (Table 2). For the medical student cohort, the most accurate planes were cervical lateral flexion for the UG and cervical flexion for the DG with MDC90 values of 10.48 and 10.10 degrees, respectively (Table 3).
Table 1
| Motion | Rater 1 | Rater 2 | Rater 3 | Rater 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| UG (mean ± SD) |
DG (mean ± SD) |
UG (mean ± SD) |
DG (mean ± SD) |
UG (mean ± SD) |
DG (mean ± SD) |
UG (mean ± SD) |
DG mean ± SD) |
||||
| Cervical flexion | 42.2±11.4 | 54.3±9.5 | 38.3±8.9 | 52.4±10.5 | 49.5±10.4 | 46.8±8.1 | 40.4±9.8 | 44.8±9.2 | |||
| Cervical extension | 60.4±17.3 | 66.1±15.0 | 59.6±15.0 | 65.6±14.3 | 55.8±12.7 | 56.5±11.3 | 54.6±11.6 | 57.5±11.6 | |||
| Cervical lateral flexion | 35.2±6.4 | 34.6±7.7 | 31.3±7.0 | 32.2±10.1 | 26.5±8.2 | 26.4±7.5 | 27.8±6.5 | 27.4±6.8 | |||
| Cervical rotation | 81.0±11.3 | 82.9±10.5 | 61.0±13.3 | 72.6±13.3 | 63.0±11.6 | 65.3±10.4 | 66.4±10.1 | 67.1±8.5 | |||
SD, standard deviation; ROM, range of motion; UG, universal goniometer; DG, digital goniometer.
Table 2
| Motion | UG | DG | UG | DG | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC2,1 | 95% CI | ICC2,1 | 95% CI | SEM (°) | MDC90 (°) | SEM (°) | MDC90 (°) | ||||
| Cervical flexion | 0.380 | 0.126 to 0.590 | 0.477 | 0.235 to 0.664 | 8.8 | 20.6 | 7.4 | 17.2 | |||
| Cervical extension | 0.819 | 0.702 to 0.893 | 0.780 | 0.642 to 0.869 | 4.2 | 9.7 | 4.6 | 10.7 | |||
| Cervical lateral flexion | 0.510 | 0.181 to 0.717 | 0.718 | 0.536 to 0.833 | 4.3 | 9.9 | 3.4 | 8.0 | |||
| Cervical rotation | 0.255 | −0.094 to 0.589 | 0.551 | −0.057 to 0.812 | 9.7 | 22.7 | 5.7 | 13.2 | |||
Results presented are average measures. UG, universal goniometer; DG, digital goniometer; ICC, intraclass correlation coefficients; CI, confidence interval; SEM, standard error of the mean; MDC, minimal detectable change.
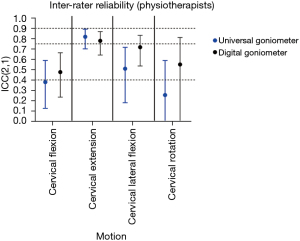
Table 3
| Motion | UG | DG | UG | DG | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ICC2,1 | 95% CI | ICC2,1 | 95% CI | SEM (°) | MDC90 (°) | SEM (°) | MDC90 (°) | ||||
| Cervical flexion | 0.579 | 0–0.822 | 0.707 | 0.487–0.833 | 6.35 | 14.81 | 4.33 | 10.10 | |||
| Cervical extension | 0.789 | 0.628–0.880 | 0.831 | 0.703–0.904 | 5.97 | 13.93 | 4.52 | 10.55 | |||
| Cervical lateral flexion | 0.685 | 0.448–0.820 | 0.655 | 0.393–0.804 | 4.49 | 10.48 | 4.70 | 10.96 | |||
| Cervical rotation | 0.561 | 0.239–0.748 | 0.720 | 0.510–0.841 | 7.95 | 18.55 | 5.29 | 12.35 | |||
Results presented are average measures. UG, universal goniometer; DG, digital goniometer; ICC, intraclass correlation coefficients; CI, confidence interval; SEM, standard error of the mean; MDC, minimal detectable change.
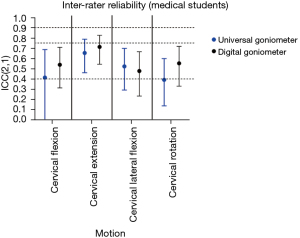
Table 4
| Motion | UG | DG | |||
|---|---|---|---|---|---|
| ICC3,1 | 95% CI | ICC3,1 | 95% CI | ||
| Cervical flexion | 0.487 | −0.011 to 0.740 | 0.507 | 0.045 to 0.748 | |
| Cervical extension | 0.529 | 0.075 to 0.761 | 0.773 | 0.554 to 0.885 | |
| Cervical lateral flexion | 0.532 | 0.071 to 0.764 | 0.728 | 0.326 to 0.877 | |
| Cervical rotation | 0.585 | 0.178 to 0.791 | 0.691 | 0.387 to 0.844 | |
Results presented are average measures. UG, universal goniometer; DG, digital goniometer; ICC, intraclass correlation coefficients; CI, confidence interval.
When assessing concurrent validity, the mean difference was the smallest for cervical lateral flexion throughout all the raters (Table 5 and Figure 5). This was further analysed using Bland-Altman plots and the 95% LOA (Figures 6-9), which again showed the most consistency between the two devices when assessing cervical lateral flexion. There was no statistically significant difference when comparing the values obtained by either device while assessing cervical lateral flexion for each rater. In contrast, however, there was a statistically significant difference for each rater when assessing cervical flexion.
Table 5
| Motion | Mean difference | |||
|---|---|---|---|---|
| Rater 1 | Rater 2 | Rater 3 | Rater 4 | |
| Cervical flexion | −12.2* | −14.1* | 2.7* | −4.3* |
| Cervical extension | −5.6* | −6.0* | −0.7 | −2.9 |
| Cervical lateral flexion | 0.6 | −0.9 | 0.1 | 0.4 |
| Cervical rotation | −1.9 | −11.6* | −2.3* | −0.7 |
*, indicates statistical significance (P<0.05).


Discussion
The current study results showed the HALO© DG as a valid and reliable substitute for the UG in the setting of ROM assessment of the certain planes of movement of the cervical spine. With the laser-guidance technology, pocket-size, single-handed operation design and 3-plane measurement capability, this device will benefit the ROM assessment for the patient undergoing cervical spine surgery and rehabilitation.
Inter-rater reliability and validity of the DG
The DG appears to be a reliable and valid substitute for the UG in the setting of ROM assessment, with a minimum of modest correlations attained when evaluating inter-rater reliability. Intra-rater reliability findings in this study are also in line with the work of previous ROM studies (15). According to the guideline (16) ICC ≥0.7 for a measure is generally accepted as ‘sufficient reliability’, DG performed well on the cervical extension and lateral flexion measurement, however, less sensitive (but still fair-good) on flexion and rotation. In essence, the DG had difficulties detecting changes when placed on a horizontal axis (i.e., on the occiput) versus the mastoid positioning to its own. It was not entirely clear why this was an issue across all raters but is most likely reflective of device-related sensitivity issues which could be rectified with additional improvements in future iterations.
Previous studies assessing the DG’s validity and reliability in the assessment of ROM have proven useful in illustrating the device’s capabilities but have suffered from significant methodological flaws. The most recent study evaluating the DG for knee ROM found unrealistically high ICCs for all methods, with values of >0.98; this was only carried out in a cohort of three subjects (17). As detailed previously, a statistical analysis completed showed that a sample size of 50 patients is required for statistical significance and to elicit valid data.
Other cervical ROM measurement tools reported previously also achieved good reliability. Alaranta et al. (18) used an inclinometer and tape measure to exam cervical sagittal movements, lateral flexion, and rotation. They reported high inter-rater reliability ICCs from 0.69 to 0.86, and fair good intra-rater reliability ICCs on sagittal and lateral flexion from 0.61 to 0.68, and poor intra-rater reliability ICC on rotation with 0.37. Their results showed better reliability compared to the UG from the current study, however, DG appears to be a more reliable tool, especially in rotation measurement with 0.69 intra-rater reliability ICC. The only setback of DG was flexion measurement, but Alaranta et al. (18) did not separate flexion and extension measurement in their study, thus it cannot directly compare the flexion and extension reliability between two studies. Antonaci et al. (19) used a 3D motion capture system to measure the human cervical motion and got ICCs from 0.68 to 0.86 in all motions except left lateral flexion with 0.47. Six markers and two infrared cameras were employed in this study. It is a statistically reliable method, also able to fully descript the head/neck mobility, however, the complex setup may not be suitable for daily clinical use compared to the DG. The CROM device tested by Audette et al. (20) also resulted good to excellent reliability. The follow-up time in their study was 2 days. The relatively extended follow-up time used in the present study was one month. A one-month follow-up time was chosen to avoid memory recall of the raters and minimise outside influences such as injury that may produce confounding results. Meanwhile, the CROM device was only designed for measure cervical ROM, whereas DG can also be used in other clinical applications such as ROM assessment of lower extremities (21).
Contemporary issues in the assessment of spine surgery outcomes: an overview
Generally, surgical candidates are evaluated per their response to conservative therapy, individual symptoms, functionality, and the cost-effectiveness of the operation. The efficacy of such operations is primarily assessed through a series of outcome measures; however, there is no consensus regarding the best tools to utilize in this population at present. Outcome measures often aid the clinical decision-making process, from determination of ongoing therapeutic modalities, to assessing the degree of impact of a patient’s disease (22). Several tools evaluating the nature and severity of back pain have been validated for use in the setting of spinal stenosis. However, there is limited data available on the efficacy of existing tools when compared in a head-to-head analysis, and they often require certain degrees of expert familiarity, particularly when several tools are niche and used only within select institutions. Indeed, a review by Vavken et al. (23) affirmed that further research is required in order to advance the field’s understanding of spinal outcome assessment and personalized spine care, as it is far from holistic at present.
The major limitation of existing functional outcome measures is that they are subjective in nature, relying heavily on data derived from patient-reported surveys, questionnaires, visual analogue scales and the like (22,24-27). These processes place great emphasis on the subjectivity of the reporter, which may prove to be a hindrance in long-term prediction of functional outcome and when informing patients of the impact of surgical interventions. Hence, standardization remains a significant challenge for clinicians and researchers (28). To the author’s knowledge, this is the largest study of its kind assessing a novel, quantitative tool to address this lack of standardization. It is hoped that with an increased focus on ROM assessment as a correlate measure for long-term functionality following surgical procedures, surgical outcomes can be better conveyed to patients and surgeon confidence in the efficacy of said procedures can be affirmed.
Existing objective outcome measures
At present, most objective assessment tools are physical task batteries, including the 6-minute walk test (6MWT), the self-paced walking test (SPWT) and the Timed Up and Go test (TUG)—gait analyses and activity monitors (4). Shorter and longer variants of these tests have also been utilized based on patient demographics and pre-operative individual ability. The SPWT has been shown to have high re-test reliability in the spinal stenosis population. Often, these tools attempt to distinguish between a patient’s capacity to perform a given task, versus their actual performance of the task itself relative to a normal individual. Unfortunately, the impact of spinal stenosis on each individual can be highly variable and hence can influence patient capacity and performance across a wide, multi-dimensional range (29). Mobbs et al. (2) affirmed this using accelerometery data derived from wearable activity tracking devices. In their pilot study of 30 patients examined over a three-month perioperative period, the team found no statistically significant correlation between the improvement in steps or distance travelled per day with improvements in Visual Analog Scale back or leg pain, Oswestry Disability Index, or Physical Component Summary scores at follow-up.
ROM assessment, similar to that utilized in the present study, has also emerged, with highly specific outcomes being assessed. For instance, Goto et al. (30), utilizing gait analysis software and electromyographic recordings, found that knee angle, knee torque and activity of the vastus lateralis increase significantly following decompressive surgery for lumbar spine stenosis, whereas activity of the paravertebral muscles decreases. This was also linked to an improvement in walking speed and posture, suggesting functional recovery. Evidently, this is of substantial use in terms of tailoring future treatment modalities. Again, however, lone physical assessment fails to quantify the effect of the disease process on a patient’s other psychometric facets, which can have clinically significant outcomes, which necessitates that ROM assessment should accompany well-validated, patient-conducted outcome measures (31).
Implications, limitations, and future directions
With the successful validation of the DG, application of the device in the assessment of a pathological cohort is the next logical step. The authors intend to recruit a patient population in a pre-operative setting (i.e., prior to spinal fusion), assess them and then conduct a follow-up at regular post-operative intervals. This study was constrained by several limitations. The physiotherapy cohort consisted of predominantly male subjects, where ideally, a more equal distribution between the sexes would be met to reflect clinical practice more accurately. The authors hypothesized that subject fatigue may begin to impair ROM measurements and hence after completing one battery of assessments, the subsequent tool would not be reading the subject’s full ROM capacity, but rather is reporting an “exhausted” value.
One limitation of the DG is its price. At approximately $400 AUD, the DG would have to bring significant benefits to clinical environment to be more favoured than its inexpensive analogue counterpart.
Conclusions
The present validation study identified the HALO© DG as a valid and reliable substitute for the UG in the setting of ROM assessment of the cervical spine in certain anatomic planes, with moderate to high inter-rater agreement, consistency, and validity, along with moderate intra-rater reliability.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Journal of Spine Surgery for the series “Objective Monitoring and Wearable Technologies including Sensor-Based Accelerometers and Mobile Health Applications for the Spine Patient”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-21-92/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-21-92/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-21-92/coif). The series “Objective Monitoring and Wearable Technologies including Sensor-Based Accelerometers and Mobile Health Applications for the Spine Patient” was commissioned by the editorial office without any funding or sponsorship. RJM served as the unpaid Guest Editor of the series and serves as the Editor-in-Chief of Journal of Spine Surgery. MHP and PR serve as the unpaid Associate Editors of Journal of Spine Surgery. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Local Health District Ethics Committee [Low/Negligible Risk (LNR). HREC 17/210] and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Misailidou V, Malliou P, Beneka A, et al. Assessment of patients with neck pain: a review of definitions, selection criteria, and measurement tools. J Chiropr Med 2010;9:49-59. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Maharaj M, et al. Physical Activity Measured with Accelerometer and Self-Rated Disability in Lumbar Spine Surgery: A Prospective Study. Global Spine J 2016;6:459-64. [Crossref] [PubMed]
- Ammendolia C, Schneider M, Williams K, et al. The physical and psychological impact of neurogenic claudication: the patients' perspectives. J Can Chiropr Assoc 2017;61:18-31. [PubMed]
- Ammendolia C, Stuber K, Tomkins-Lane C, et al. What interventions improve walking ability in neurogenic claudication with lumbar spinal stenosis? A systematic review. Eur Spine J 2014;23:1282-301. [Crossref] [PubMed]
- Youdas JW, Carey JR, Garrett TR. Reliability of measurements of cervical spine range of motion--comparison of three methods. Phys Ther 1991;71:98-106. [Crossref] [PubMed]
- Whitcroft KL, Massouh L, Amirfeyz R, et al. Comparison of methods of measuring active cervical range of motion. Spine (Phila Pa 1976) 2010;35:E976-80. [Crossref] [PubMed]
- Prushansky T, Dvir Z. Cervical motion testing: methodology and clinical implications. J Manipulative Physiol Ther 2008;31:503-8. [Crossref] [PubMed]
- Pool JJ, Hoving JL, de Vet HC, et al. The interexaminer reproducibility of physical examination of the cervical spine. J Manipulative Physiol Ther 2004;27:84-90. [Crossref] [PubMed]
- Hole DE, Cook JM, Bolton JE. Reliability and concurrent validity of two instruments for measuring cervical range of motion: effects of age and gender. Man Ther 1995;1:36-42. [Crossref] [PubMed]
- Nussbaumer S, Leunig M, Glatthorn JF, et al. Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord 2010;11:194. [Crossref] [PubMed]
- American Academy of Orthopaedic Surgeons. Joint motion: method of measuring and recording. Chicago, IL, USA: American Academy of Orthopaedic Surgeons, 1965.
- Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 2016;15:155-63. [Crossref] [PubMed]
- Kottner J, Audige L, Brorson S, et al. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. Int J Nurs Stud 2011;48:661-71. [Crossref] [PubMed]
- Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 2nd edition. Hoboken, NJ, USA: Prentice Hall, 2000.
- Correll S, Field J, Hutchinson H, et al. Reliability and validity of the Halo digital goniometer for shoulder range of motion in healthy subjects. Int J Sports Phys Ther 2018;13:707-14. [Crossref] [PubMed]
- Hripcsak G, Heitjan DF. Measuring agreement in medical informatics reliability studies. J Biomed Inform 2002;35:99-110. [Crossref] [PubMed]
- Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. J Exp Orthop 2018;5:46. [Crossref] [PubMed]
- Alaranta H, Hurri H, Heliövaara M, et al. Flexibility of the spine: normative values of goniometric and tape measurements. Scand J Rehabil Med 1994;26:147-54. [PubMed]
- Antonaci F, Bulgheroni M, Ghirmai S, et al. 3D kinematic analysis and clinical evaluation of neck movements in patients with whiplash injury. Cephalalgia 2002;22:533-42. [Crossref] [PubMed]
- Audette I, Dumas JP, Côté JN, et al. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther 2010;40:318-23. [Crossref] [PubMed]
- Muralidaran S, Wilson-Smith AR. Validation of a Novel Digital Goniometer as a Range of Motion Assessment Tool for The Lower Extremity. J Orthop Res Ther 2020;5:1158.
- Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med 2008;7:161-3. [Crossref] [PubMed]
- Vavken P, Ganal-Antonio AK, Quidde J, et al. Fundamentals of Clinical Outcomes Assessment for Spinal Disorders: Clinical Outcome Instruments and Applications. Global Spine J 2015;5:329-38. [Crossref] [PubMed]
- Velentgas P, Dreyer NA, Nourjah P, Smith SR, Torchia MM. editors. Developing a Protocol for Observational Comparative Effectiveness Research: A User's Guide. Rockville, MD, USA: Agency for Healthcare Research and Quality, 2013.
- Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976) 2000;25:3115-24. [Crossref] [PubMed]
- Turner JA, Comstock BA, Standaert CJ, et al. Can patient characteristics predict benefit from epidural corticosteroid injections for lumbar spinal stenosis symptoms? Spine J 2015;15:2319-31. [Crossref] [PubMed]
- Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther 2002;82:8-24. [Crossref] [PubMed]
- Azimi P, Mohammadi HR, Benzel EC, et al. Lumbar Spinal Canal Stenosis Classification Criteria: A New Tool. Asian Spine J 2015;9:399-406. [Crossref] [PubMed]
- Conway J, Tomkins CC, Haig AJ. Walking assessment in people with lumbar spinal stenosis: capacity, performance, and self-report measures. Spine J 2011;11:816-23. [Crossref] [PubMed]
- Goto T, Sakai T, Enishi T, et al. Changes of posture and muscle activities in the trunk and legs during walking in patients with lumbar spinal stenosis after decompression surgery. A preliminary report. Gait Posture 2017;51:149-52. [Crossref] [PubMed]
- Gautschi OP, Joswig H, Corniola MV, et al. Pre- and postoperative correlation of patient-reported outcome measures with standardized Timed Up and Go (TUG) test results in lumbar degenerative disc disease. Acta Neurochir (Wien) 2016;158:1875-81. [Crossref] [PubMed]


