
Cardiac asystole following high spinal cord injury: a case report
Introduction
Cervical spine injuries or high spinal cord injuries (HSCI) can present with cardiac manifestations and are frequently overlooked when considering possible etiologies (1). These cardiac abnormalities secondary to cervical trauma are believed to be the result of autonomic pathway dysregulation and most often present with bradycardia, which can progress to cardiac arrest/asystole (1). The risk of progression to cardiac asystole from a HSCI increases with prolonged bradycardia (2). Risk factors for prolonged bradycardia in these patients include hypotension at the time of presentation, pneumonia, and tracheostomy (2). Some procedures including endotracheal suctioning and changing of body positioning are associated with increased incidence of bradycardia in cervical trauma patients (2). Although cardiac asystole is thought to be more common with severe cervical trauma, low-impact trauma has also been reported to cause cardiac asystole (3). Populations at high risk for low-impact fractures and cervical trauma include the elderly and in patients with ankylosing spondylitis (3-5). The literature recommends that in patients with cardiac asystole of unknown etiology, a further traumatic cervical spinal cord injury should be considered as a potential cause (3).
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-669).
Case presentation
A 67-year-old left hand dominant female retired nurse with no past medical history presented following a motor vehicle accident which occurred at 20:15 on 4/24/2018. She was an unrestrained front seat passenger that was T-boned near the passenger side. Air bags did not deploy. When emergency medical services (EMS) arrived, the patient was reportedly cyanotic and unresponsive and pulseless. She did have a short period of CPR performed. Return of spontaneous circulation (ROSC) was obtained after 1–2 minutes. The patient slowly became responsive after 10 minutes of assisted ventilations. Prehospital 12-lead electrocardiogram (EKG) showed atrial fibrillation along with inferior and lateral ST segment depressions. The patient had a Glasgow Coma Scale (GCS) of 13 upon arrival to the emergency department (ED) with resolution of ST segment depressions. The patient had breath sounds bilaterally. The patient had no gross deformities of her extremities upon arrival to the ED.
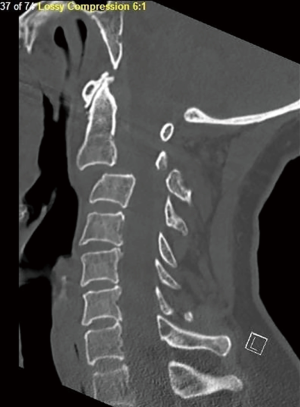
Initial cervical spine CT showed anterior subluxation of C2 on C3. There were comminuted displaced C2 fractures involving the right vascular foramen, right transverse process, right pedicle, base of the spinous process and left lamina. There was a displaced fracture of the left C3 facet and left transverse process with involvement of the vascular foramen (Figure 1). No fractures of the thoracic or lumbar spine. She also had a sternal body fracture and fractures of the right 1st-4th ribs and left 2nd-5th ribs. Computed tomography angiography (CTA) neck showed irregularity of the right vertebral artery at the level of the displaced C2 fracture and irregularity of the left vertebral artery at the level of the C3 fracture. There were no acute intracranial processes on head computed tomography (CT).
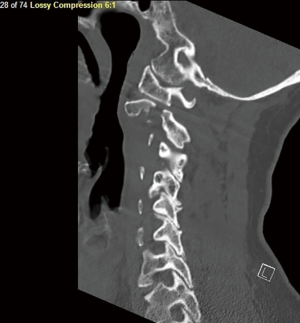
Upon initial evaluation at the ED, the patient reported anterior chest wall pain and right-side neck pain. Her breathing was unlabored. She had equal and reactive pupils. There was no facial asymmetry. She was able to follow commands and was grossly motor and sensory intact (American Spinal Injury Association Impairment Scale Score E). There was no spasticity or clonus in her lower extremities. Her extremities were sensate to light touch, pin prick, and proprioception. The patient denied any paresthesias as well as bowel or bladder symptoms. She was kept in a cervical collar and was admitted to the trauma ICU at 23:45 on 4/24/2018. At 01:00 2/25/2018, the patient reported numbness in her bilateral upper extremities and left lower extremity with rapid progression to motor deficits. She had voluntary plantarflexion of her right foot and ankle and flaccid paralysis of her left upper and lower extremities and spasticity in the right upper extremity. She was started on Decadron 10 mg every six hours. Magnetic resonance imaging (MRI) showed significant cord compression by an epidural hematoma and spinal cord changes from C1-C2 to C3-C4 (Figure 2). The anterior longitudinal ligament, posterior longitudinal ligament, and ligamentum flavum appeared to be torn at the level of C2-C3. The patient was taken emergently to the operating room on 04/25/2018 at 07:15 for open reduction of C2-C3 fracture, C2-C3 laminectomies, and C1-C5 posterolateral fusion with instrumentation.
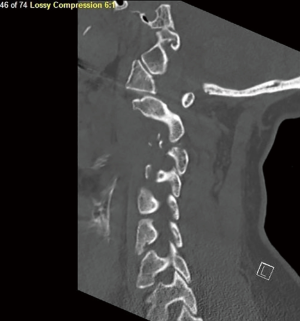
A longitudinal midline incision was made from occiput to C5 spinous process. The fracture dislocation of C2-C3 was readily identifiable. A subperiosteal dissection to the tips of the lateral masses was performed. Screws were placed in bilateral lateral masses of C1. Screws were placed on the right C3 lateral mass due to left facet fracture and bilateral lateral masses of C4 and C5. A laminectomy was performed at C2 and C3 to completely decompress the spinal cord. There was no residual stenosis or evidence of spinal fluid leak. Rods were contoured and placed to stabilize C1 to C5 (Figure 3).
The patient was extubated on postoperative day (POD) 1 without complication. Her neurologic function continued to improve and the patient was transferred to the floor with sensation and motor function intact in all four extremities. She was discharged to rehab on 05/03/2018. Her right upper extremity and bilateral lower extremities had mostly 4/5 muscle strength, while left upper extremity had 3/5 muscle strength both proximally and distally. On the day of discharge to rehab, she was ambulating with physical therapy (PT). The patient was discharged home on 5/15/2018. She had 4/5 strength in bilateral upper and lower extremities throughout (American Spinal Injury Association Impairment Scale Score D). At this time the patient had good grip strength. She did complain of bilateral hand numbness and tingling along with persistent neck and back pain.
On follow-up 02/05/2020 the patient continued to complain of posterior neck, left shoulder, and arm pain as well as spasms and paresthesia of her left hand. She was prescribed cortisone and BOTOX injections as well as methocarbamol for pain. Her motor strength was grossly intact and relatively symmetric. She reported numbness of her left hand and forearm. X-rays demonstrated well-healed fractures and aligned hardware. MRI demonstrated signal change in the spinal cord at C3 with myelomalacia. There was no evidence of stenosis or post-traumatic syrinx (Figures 4,5).
Informed Consent Statement: all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
High spinal cord injury is often a devastating injury that most commonly occurs in young males (80%) and is often associated with prolonged neurologic deficit following the initial injury (93%) (2). These injuries carry a high mortality rate (9.4–19%) and can occasionally be the cause of cardiac abnormalities including bradycardia and cardiac asystole at the time of presentation (2,6-8).
Cardiac asystole following cervical spine trauma is a relatively rare complication found to occur in 15–16% of patients with HSCI and is thought to be due to autonomic dysregulation following the initial insult (1,9-11). It is more often associated with a high-energy mechanism of injury and more severe spinal cord injuries, however it has also been reported to occur following low-energy mechanisms such as a fall from standing (3,9). Current literature lacks a general consensus on timing and duration of cardiac asystole following the initial injury (2). Previous studies have reported incidence of bradycardia following HSCI to peak between 4–7 days, although cardiac abnormalities have been noted to persist for as long as 2–6 weeks following initial injury (2,9,11,12).
In this case, the patient was found unresponsive, cyanotic, and pulseless in the field by EMS after a high-energy motor vehicle collision. The patient had ROSC after a short period of CPR and was brought to the hospital where she was diagnosed with anterior subluxation of C2 on C3, comminuted displaced C2 fractures involving the right vascular foramen, right transverse process, right pedicle, base of the spinous process and left lamina, and a displaced fracture of the left C3 facet and left transverse process with involvement of the vascular foramen on CT scan. The patient subsequently developed progressive motor and sensory deficits of her extremities. She remained hemodynamically stable and did not experience any further cardiac events prior to or after her surgery, suggesting a more acute onset and recovery of cardiac symptoms than previously reported.
Studies have demonstrated efficacy for both medical management with inotropic agents and vasopressors as well as placement of cardiac pacemaker for the treatment of bradycardia and cardiac asystole secondary to HSCI (2,7,10,11). In our case our patient experienced acute cardiac asystole with rapid recovery of cardiac function, and did not need further intervention for the cardiac manifestations of her injury. We suggest that in patients with HSCI who experience cardiac asystole with rapid recovery, a work-up prior to surgery should be performed to rule out any cardiac cause of asystole. Surgery to address motor and sensory deficits in these patients should not be delayed, and careful monitoring of the patient’s cardiovascular status via telemetry prior to and after surgery should be considered. Medical management or cardiac pacing may not be required in patients who experience rapid recovery of cardiac function following cardiac asystole secondary to HSCI. This is demonstrated by the patient in this case who tolerated surgery well and was able to be quickly extubated postoperatively, discharged from the hospital, and has had no other cardiac manifestations of her injury to date.
HSCI can often be overlooked as the initial cause of cardiac asystole at presentation which may lead to a delay in diagnosis as well as the performance of more invasive diagnostic testing such as cardiac catheterization (1,3,9). We recommend providers have a high index of suspicion for these injuries in patients presenting with cardiac manifestations following trauma. This can aid in diagnosis of spinal cord pathology as a cause of cardiac dysfunction and can help guide surgical and medical management.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-669
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-669). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim SW, Park CJ, Kim K, et al. Cardiac arrest attributable to dysfunction of the autonomic nervous system after traumatic cervical spinal cord injury. Chin J Traumatol 2017;20:118-21. [Crossref] [PubMed]
- Shaikh N, Rhaman MA, Raza A, et al. Prolonged bradycardia, asystole and outcome of high spinal cord injury patients: Risk factors and management. Asian J Neurosurg 2016;11:427-32. [Crossref] [PubMed]
- Mayà-Casalprim G, Ortiz J, Tercero A, et al. Cervical spinal cord injury by a low-impact trauma as an unnoticed cause of cardiorespiratory arrest. Eur Heart J Case Rep 2020;4:1-6. [Crossref] [PubMed]
- Tanaka H, Kawanishi M, Yokoyama K, et al. Delayed Diagnosis of Upper Cervical Spine Injury Presenting with Cardiopulmonary Arrest in Elderly Patients—A Case Report and Review of Literature. Spinal Surg 2018;32:192-6. [Crossref]
- Han SW, Kim SH. Ankylosing spondylitis with cervical fracture, cardiac arrest, locked-in syndrome and death. BMJ Case Rep 2012;2012:bcr0120125522 [Crossref] [PubMed]
- Bilello JF, Davis JW, Cunningham MA, et al. Cervical spinal cord injury and the need for cardiovascular intervention. Arch Surg 2003;138:1127-9. [Crossref] [PubMed]
- Shao J, Zhu W, Chen X, et al. Factors associated with early mortality after cervical spinal cord injury. J Spinal Cord Med 2011;34:555-62. [Crossref] [PubMed]
- Rangappa P, Jeyadoss J, Flabouris A, et al. Cardiac pacing in patients with a cervical spinal cord injury. Spinal Cord 2010;48:867-71. [Crossref] [PubMed]
- Lehmann KG, Lane JG, Piepmeier JM, et al. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: incidence, time course and severity. J Am Coll Cardiol 1987;10:46-52. [Crossref] [PubMed]
- Moerman JR, Christie BD 3rd, Sykes LN, et al. Early cardiac pacemaker placement for life-threatening bradycardia in traumatic spinal cord injury. J Trauma 2011;70:1485-8. [Crossref] [PubMed]
- Franga DL, Hawkins ML, Medeiros RS, et al. Recurrent asystole resulting from high cervical spinal cord injuries. Am Surg 2006;72:525-9. [Crossref] [PubMed]
- Piepmeier JM, Lehmann KB, Lane JG. Cardiovascular instability following acute cervical spinal cord trauma. Cent Nerv Syst Trauma 1985;2:153-60. [Crossref] [PubMed]




