
Varicocele complicating an anterior lumbar interbody fusion: a case report
Introduction
Anterior lumbar interbody fusion (ALIF) is a commonly performed procedure for lumbar degenerative disease with excellent results, particularly for discogenic low back pain (1-4). However, reported complications associated with ALIF include vessel injury, retrograde ejaculation, and ureteral and viscus organ injury (2,4,5). The development of a varicocele after ALIF has not been previously described in the literature. We report a case of varicocele as a complication of ALIF. We describe the occurrence of a varicocele following ALIF, its possible pathophysiology and treatment options. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-609).
Case presentation
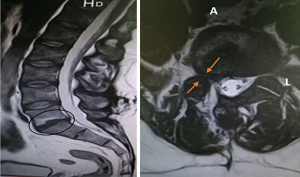
A 35-year-old patient who had been diagnosed with discogenic low back pain four years before and, operated twice on a L5S1 herniated disc, with excellent results, presented with lumbar pain six months later. Visual Analog Scale results showed a score of 8/10 for back pain, despite medical treatment. He also experienced right sciatica. Neurological examination was normal. MRI demonstrated a loss of disc height with Modic 2 endplate changes and a small recurrent L5S1 disc herniation (Figure 1). The patient underwent ALIF by a left retroperitoneal approach. No intraoperative complications were identified. The patient’s preoperative symptoms improved after surgery and the postoperative course was uneventful. He was discharged from the hospital on the 5th postoperative day. Three months after surgery, the patient complained of discomfort and scrotal pain. The patient’s medical history includes migraine headache as well as depression. Examination revealed a grade 3 varicocele according to the Dubin and Amelar classification (6) (Figure 2). Scrotal Doppler US demonstrated dilatation of the veins of the pampiniform plexus (Figure 3). A lumbar CT scan revealed a bulky left spermatic vein closed to the ureter (Figure 4). The patient was treated with platelet anti-aggregation especially acetylsalicylic acid 160 mg per day, he was seen at control intervals of 1, 3 and 5 months. Progress was seen as we had a regression of the varicocele. No adverse event was identified.
The patient adhered to the treatment and was satisfied with the result.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Varicocele is defined as an abnormal dilatation of the veins of the pampiniform plexus in the spermatic cord, with an incidence of 15% in the general population (7). Varicocele is the consequence of genetic defects, including undifferentiated connective tissue dysplasia (UCTD) with hereditary insufficiency of the venous valves and weakness of the testicular vein walls (8). This vein originates from the two terminal venous branches of the pampiniform plexus in the internal iliac fossa just after their exit from the inguinal canal. Gonadic vessels run along the psoas muscle, cross forwards over the ureter and are covered by the right and left mesocolic fascia of Toldt and the posterior parietal peritoneum. After a long course, the right internal spermatic vein ends in the inferior vena cava with an acute angle at the L2 level. On the left, the internal spermatic vein vertically ascends and curves at right angles into the left renal vein (9,10). This explains why varicocele occurs predominantly on the left side (78% to 93% of cases) (7,11). After known genetic and hereditary factors (7,8,12), compression factors in both the spermatic veins and left renal vein appear to play a key role in the pathogenesis of varicocele (12-14).
During ALIF by the left retroperitoneal route, both the ureter and gonadal vessels must be separated from the external iliac vessels. This mechanical stress could explain thrombosis of the left gonadic vein and thus the varicocele post ALIF. Indeed, the peritoneum and left gonadal vessels are pushed to the right, whereas the external iliac vessels remain to the left. The use of retractors creates a corridor in which to operate and the right retractor may lead to compression of the left gonadic vessels. A careful separation of the gonadal vessels could prevent this complication.
The diagnosis of varicocele is essentially based on clinical evidence, in particular the finding of a tortuous dilatation of the pampiniform plexus veins that, increases during the Valsalva maneuver. It needs to be distinguished from an inguinal hernia or scrotal hemangioma, which at the beginning stage may clinically constitute a differential diagnosis. Several classifications have been developed based on clinical examination of which that, of Dubin and Amelar is by far the most cited in the literature. Their classification is as follows: grade 1: varicoceles are palpable only during the Valsalva maneuver; grade 2: varicoceles are palpable without the Valsalva maneuver; grade 3: varicoceles are visible and palpable without the Valsalva maneuver. The use of diagnostic imaging techniques, ranging from phlebography to spermatic-vein Doppler US, can be helpful (6).
Varicoceles can be treated surgically or by radiological embolization. Embolization of the spermatic vein was first described by Iaccarino et al. in 1980 (15). This technique requires selective catheterization of the spermatic vein by the femoral or internal jugular approach, followed by its occlusion with either a sclerosant or a solid embolization agent (6,16). The immediate success rate is approximately 95% (17). The long-term success rate is 90–95% of cases. Surgical treatment includes seven distinct techniques, some of which are no longer used. High ligature of the spermatic vein by the extraperitoneal route, at the level of the anterosuperior iliac spine, is currently the most widely used treatment of varicocele. Ligation by the inguinal or subinguinal route is preferred by some in cases of voluminous varicocele with dilatation of the cremasteric veins. Laparoscopy has not been proven to be superior to open surgery (6).
Varicocele appears as a rare complication of ALIF, this complication is due to the mechanical stress exerted on the left spermatic veins during this surgery. The specific treatment of varicocele post ALIF is not described in the literature. In our case, platelet anti-aggregation resulted in a regression of clinical signs. This finding should be subject to evaluate platelet anti aggregation in the treatment of varicocele.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-609
Peer Review File: Available at http://dx.doi.org/10.21037/jss-20-609
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-609). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mobbs RJ, Lennox A, Ho YT, et al. L5S1 anterior lumbar interbody fusion technique. J Spine Surg 2017;3:429-32. [Crossref] [PubMed]
- Teng I, Han J, Phan K, et al. A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci 2017;44:11-7. [Crossref] [PubMed]
- Mobbs RJ, Loganathan A, Yeung V, et al. Indications for anterior lumbar interbody fusion. Orthop Surg 2013;5:153-63. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [PubMed]
- Patel AA, Spiker WR, Daubs MD, et al. Retroperitoneal lymphocele after anterior spinal surgery. Spine 2008;33:E648-52. [Crossref] [PubMed]
- Cornud F, Belin X, Amar E, et al. Varicocele: strategies in diagnosis and treatment. Eur Radiol 1999;9:536-545. [Crossref] [PubMed]
- Saypol DC. Varicocèle. J Androl 1981;2:61-71. [Crossref] [PubMed]
- Studennikova VV, Severgina LO, Tsarichenko DG, et al. Current view on the pathogenesis of varicocele and the problem of its recurrence. Urologiia 2018;1:150-4. [Crossref] [PubMed]
- Bensussan D, Huguet JF. Radio-anatomie de la veine spermatique. Anat Clin 1984;6:25-7. [Crossref]
- Wishahi MM. Anatomy of the venous drainage of the human testis: testicular vein cast, microdissection and radiographic demonstration. A new anatomical concept. Eur Urol 1991;20:154-60. [Crossref] [PubMed]
- Turner TT. Varicocele:still an enygma. J Urol 1983;129:695-9. [Crossref] [PubMed]
- Ludwig G. Pathogenesis of varicocele. In: Varicocele and male infertility. Berlin: Springer, 1982:6-12.
- Sayfan J, Halevy A, Oland J, et al. Varicocele and left renal vein compression. Fertil Steril 1984;41:411-7. [Crossref] [PubMed]
- Lewis DS, Grimm LJ, Kim CY. Left renal vein compression as cause for varicocele: prevalence and associated findings on contrast-enhanced CT. Abdom Imaging 2015;40:3147-51. [Crossref] [PubMed]
- Iaccarino V. A non-surgical treatment of varicocele: transcatheter sclerotherapy of gonadal veins. Ann Radiol 1980;23:369-71. [PubMed]
- Halpern J, Mittal S, Pereira K, et al. Percutaneous embolization of varicocele: technique, indications, relative contraindications, and complications. Asian J Androl 2016;18:234-8. [Crossref] [PubMed]
- Wells I. Embolization of varicoceles. Curr Opin Urol 1995;5:82-4. [Crossref]





