Tailored minimally invasive tubular laminectomies for the urgent treatment of rare holocord spinal epidural abscess: case report and review of technique
Introduction
Holocord spinal epidural abscess (SEA) is a very rare conditions with only a few case that have been so far reported in literature (1-10). Although non-surgical treatment has been utilized in selected patients (11), most of the reported cases have required urgent surgical decompression and drainage. In light of the widespread infection with involvement of the whole length of the spinal axis and the frequent presence of associated medical comorbidities, such diabetes, obesity or osteomyelitis/diskitis, the choice of the safest and more effective surgical approach can be challenging.
In this article we describe the use of tandem alternating laminectomies for the minimally invasive urgent treatment of a symptomatic cervico-sacral (holocord) SEA. To facilitate drainage and decompression, limit the amount of soft tissue trauma and exposure, and minimize the time in the operative room, alternating tandem incisions based on the preoperative radiological studies were utilized, with levels and laterality of the unilateral approaches that were planned according to the sagittal and axial extension of the abscess, respectively.
Although the use of tubular decompression in multilevel SEA has been reported in the past, the suggestion to tailor such technique not only for level but also for laterality when treating rare holocord epidural infections, has not been previously made.
We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jss-20-603).
Case presentation
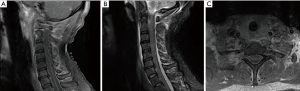
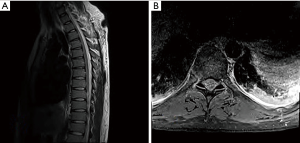
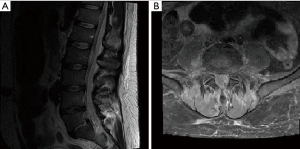
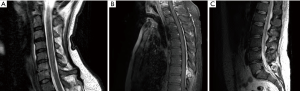
This adult gentleman with history of chronic low back pain and of IV drug use, presented to the ER complaining of worsening low back pain over a few weeks, intermittent low grade fever and onset of acute severe upper and lower extremities weakness that led to a fall without loss of consciousness and onset of urinary incontinence. At clinical examination he had a severe tetraparesis with sensory level at T10 and minimal motion of the trapezius (C3-4) but no muscle activity below that level. On MRI and CT evaluations there was evidence of lumbar diskitis/osteomyelitis at L5–S1, possible diskitis at C6–7, with a dorsal holocord compressive SEA spanning from C3–4 to S1 (Figures 1-3). A small central acute HNP was also seen at C6-7 with faint increased signal on T2 images within the cord at that level, but no fracture/subluxation or posterior ligamentous injury. The cervical spine was promptly immobilized on a rigid orthosis and medical management and work up, comprehensive of empiric antibiotic therapy were started. No hemodynamic signs of spinal cord shock were present. Urgent SEA surgical decompression was recommended and, in light of the medical scenario and timing of the events, decision was made to defer the treatment of the cervical disk herniation to a later time, if needed.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).
Surgical technique
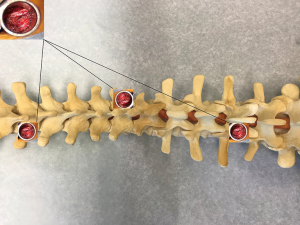
On the thoracic spine the SEA was more prominent on the left, while it was compressing mostly the right side of the dural sac in the lumbar region (Figures 2B,3B). There was also suspicion for a post-traumatic cord contusion at C6–7. Based on clinical and radiological evaluations, we planned to perform urgent tandem laminectomies at C6–7 and at T8 from the left side and at L4 from the right side. On the cervical spine the SEA had bilateral extension, therefore a left side approach was chosen at this level to facilitate the right handed surgeon. A METRx system was utilized for the tandem tubular decompression at each level.
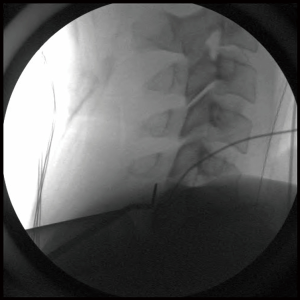
After positioning the patient prone and insuring that vital signs were stable with no hypotension, the skip laminectomies were performed starting from the cervical incision. Once the laminectomies at C6-7 were made and the ligament opened, the epidural purulent collection of fluid, consistent with the diagnosis of SEA, was drained and send to Microbiology/Pathology for analysis. After tilting the tubular retractor cranially, a red rubber catheter was gently passed into the epidural space to reach the C4 level (Figure 4). Irrigation with saline and antibiotic solution via the catheter was able to displace the mid cervical abscess as the returning mixed fluid was collected and aspirated from the laminectomy site under direct visualization. In light of the possible cord contusion and utilizing the same fascial incision, the cervical laminectomy was then extended to encompass three levels (C5 to C7, tilting and gently mobilizing the tubular retractor cranially and caudally). After hemostasis was achieved, the cervical tubular retractor was left in place and a left T8 skip laminectomy was performed. After draining the local SEA, a second rubber catheter was carefully fed into the epidural space, toward the high thoracic region, and gentle irrigation was restarted from this end. Intermittently, the irrigation was resumed from the cervical incision, as the injection of saline from below was able to displace more of the purulent collection. A second METRx tube was left inside the thoracic incision and while the surgical assistant kept gently irrigating the surgical sides, a third tandem laminectomy at L4 on the right (according to the preoperative planning) was performed. A copious amount of pus was drained and another catheter was passed into the epidural space toward the higher lumbar levels, as gentle irrigation was again applied. This time the epidural washout was alternated with irrigation of the lower thoracic levels by advancing the thoracic rubber catheter caudally (from the thoracic incision), toward the lumbar region (by tilting the tubular retractor). Catheter irrigation toward the sacral region was also completed from the lumbar incision. Such sequential and alternating catheter irrigations of the cervico-thoracic and lumbo-sacral epidural spaces continued, from the tandem laminectomies sites, until no more purulent material could be retrieved. The tubular retractors were then removed and muscles, fascia and skin were closed in the usual fashion. The surgery lasted approximately 120 minutes and blood loss was less that 50 cc. Blood cultures and microbiology analysis were consistent with a methicillin-sensitive staphylococcus aureus infection and antibiotic treatment was tailored to culture sensitivity. Serial postoperative MRIs confirmed the good evacuation/decompression of the holocord SEA and medical and rehabilitation treatments were maximized as the cervical spine remained immobilized with a cervical orthosis (Figure 5). The wounds healed well and no procedural complications were recorded. Although at a 3- month follow up the sensory level was improved to T4, the patient regained only minimal and not against gravity muscle strength. Follow up radiological studies ruled out new areas of spinal compression or recurrent SEA.
Discussion
Spinal epidural abscess, an infection characterized by the collection of purulent material into the epidural space, is a severe condition often associated to medical comorbidities such as diabetes mellitus, obesity, percutaneous procedures or history of IV drugs use (12). Abscesses that involve the full length of the spine, from the cervical to the sacral regions (holocord SEA) are rare, and account for 1% of cases according to a large meta-analysis conducted on 915 patients with SEA (13). Although commonly located in the posterior epidural space, holocord SEA have also been reported to involve the ventral epidural space (14).
Patients commonly present with pain not responsive to NSAID medications, occasionally fever and, depending on location and extension of the infection, rapidly progressive neurological deficits may develop. Holocord SEA are usually treated with urgent surgical drainage to decompress the spinal cord/dural sac, decrease the burden of the infection and lower the risks of venous thrombosis or ischemia infection mediated. Severe acute neurological deficits may in fact be the result of spinal cord compression, spinal cord ischemia, venous thrombophlebitis or its combination (15).
Although the use of open multilevel laminectomies can certainly be effective to decompress the epidural space, due to the extent of the disease and the morbidity associated with a lengthy and extensive open surgery in an urgent setting and in an infected field, this surgery may not be inconsequential (16). Amount of blood loss, degree of paraspinal muscles trauma, length of incisions in bedridden patients and risks of postoperative progressive spinal deformity, should all be factored in when planning and selecting the best surgical operation for these patients and the use of limited laminectomies have been advocated in the past (17). In light of all of these considerations, the use of minimally invasive and catheter based procedures has been suggested as an effective and less traumatic option to treat multilevel and holocord SEA, especially in an urgent setting (18-21) and the use of tubular laminectomies to treat multilevel SEA has been previously described (22). With the introduction of tubular minimally invasive techniques, several variations of such less invasive procedures have been reported and terms such as “skip”, “apical”, “double-triple barrel”, “alternating side” laminectomies have been introduced (23-27). Aside from facilitating daily postoperative wound care, the use of level-skipping muscle sparing procedures can minimize surgical related trauma and intraoperative blood loss, also reducing postoperative pain and length of the surgery (28). In our case, due to the possible trauma to the cord, the use of tandem laminectomies allowed for an effective and quick drainage of the SEA, avoiding the risks related to a lengthy surgery with significant blood loss and possible intraoperative hypotension.
The use of “skip” laminectomies with alternating side incisions for unilateral approaches with bilateral decompression, was designed to minimize soft tissue trauma, muscles imbalance as well as iatrogenic postoperative instability (25).
Tandem or alternating tubular laminectomies are now often utilized for the treatment of many degenerative conditions such as tandem stenosis, multilevel disk herniation, and multilevel spinal stenosis (28,29), with the goals to minimize paraspinal muscles trauma, decrease the use of postoperative opioids and limit the degree of postoperative muscle spasms. In level-skipping procedures described for the treatment of SEA, laminectomies can also be performed at the rostral and caudal ends of the purulent collection, with rubber or Fogarty catheters utilized to drain the epidural space for the length of a few vertebral levels, by means of gentle continuous irrigation with saline and antibiotic solution and gentle suction (23).
In the technique we illustrated, the level of the laminectomies was tailored and planned according to the sagittal extension of the SEA, while the laterality of the incision/tubular approach was guided by the radiological extension of the fluid collection on the axial plane, which in our case led to tandem, alternating sides, laminectomies (Figure 6). The choice to tailor the laminectomies depending on the extension of the abscess not only on the sagittal but also on the axial plane, not only led to an effective and relatively fast decompression, but also minimized the need for an “over-the-top” tubular decompressive laminectomy, thus shortening the overall duration of the urgent surgical procedure. This recommendation to tailor the tubular tandem approach not only for level but also for laterality, while treating rare holocord epidural infections, has not been previously suggested. In case of loculated or less fluid abscesses (at times seen when dealing with slowly evolving or more chronic infections), approaching the purulent collection from the side most heavily involved, may in fact facilitate the removal of thick granulation tissue from the dura, thus obviating the need for an extensive “over-the-top” decompression (30). Although the tubular retractors can be easily tilted contralaterally to visualize central dural and contralateral foramens, in cases where granulation tissue adherent to the dura is present, an ipsilateral approach offers the quickest route for its removal and minimizes the need of dural retraction, which is also not possible when the pathology involves the cervical and thoracic levels.
Conclusions
Holocord SEA is a rare but severe condition that can have life changing consequences if left untreated. Minimally invasive, muscle sparing approaches have proven safe and efficient in allowing adequate spinal decompression and drainage of multilevel and holocord SEA.
A tailored tandem approach with tubular laminectomies, planned according to the sagittal length (for level) and axial extension (for laterality) of the SEA, can be an effective and lesser traumatic method to treat such condition in an urgent setting. To better evaluate the possible benefits of minimally invasive treatments of holocord SEA on the incidence of infection related late events (such mechanical instability or loss of spinal alignment) over open procedures, long term follow-up data are needed.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The author has completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jss-20-603
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-603). FR has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Due to the timing of this publication we were unable to obtain written informed consent. Nevertheless no personal information were disclosed in the manuscript/images and the patient’s privacy was protected. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tahir MZ, Hassan RU, Enam SA. Management of an extensive spinal epidural abscess from C-1 to the sacrum. Case report. J Neurosurg Spine 2010;13:780-3. [Crossref] [PubMed]
- Ghosh PS, Loddenkemper T, Blanco MB, et al. Holocord spinal epidural abscess. J Child Neurol 2009;24:768-71. [Crossref] [PubMed]
- Leonard J, Kaufman B. Treatment of a holocord epidural abscess. Case illustration. J Neurosurg 2001;94:179. [PubMed]
- Moghaddam AM, Kilincoglu BF, Atalay B, et al. Holocord epidural abscess: case report. Adv Ther 2003;20:324-8. [Crossref] [PubMed]
- Burton KR, Wang X, Dhanoa D, et al. Holocord spinal epidural abscess in a pregnant patient presenting as premature labour: a rare presentation of an unusual diagnosis. CJEM 2014;16:334-8. [Crossref] [PubMed]
- Sahu KK, Chastain I., Sahu KK, et al. A rare case of holocord spinal epidural abscess. QJM 2020;113:302-3. [Crossref] [PubMed]
- Gelabert-González M, Cutrín-Prieto J, Allut AG, et al. Holocord spinal epidural empyema. Rev Neurol 2006;43:637-8. [Crossref]
- Bridges KJ, Than KD., Bridges KJ, et al. Holospinal epidural abscesses - Institutional experience. J Clin Neurosci 2018;48:18-27. [Crossref] [PubMed]
- Khattar NK, Zussman BM, Agarwal N, et al. Use of Omnipaque Intraoperative Dye in the Surgical Treatment of Pan-Spinal Epidural Abscesses: Technical Case Report. Neurosurgery 2015;11 Suppl 3:E479-82. [PubMed]
- Gorchynski J, Hwang J. McLaughlin A methicillin-resistant Staphylococcus aureus-positive holospinal epidural abscess Am J Emerg Med 2009;27:514.e7-9. [Crossref]
- O’Brien C, Lenehan B, Street J. Non-operative management of an extensive anteriorly located epidural abscess. J Clin Neurosci 2011;18:1401-2. [Crossref] [PubMed]
- Rigamonti D, Liem L, Sampath P, et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol 1999;52:189-96. [Crossref] [PubMed]
- Reihsaus E, Waldbaur H, Seeling W, et al. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 2000;23:175-204; discussion 205. [Crossref] [PubMed]
- Supreeth S, Al Ghafri K. Ventral holocord spinal epidural abscess managed surgically in a critical setting. Surg Neurol Int 2019;10:248. [Crossref] [PubMed]
- Shah NH, Roos KL. Spinal Epidural Abscess and Paralytic Mechanisms. Curr Opin Neurol 2013;26:314-7. [Crossref] [PubMed]
- Payer M, Walser H.. Evacuation of a 14-vertebral-level Cervico-Thoracic Epidural Abscess and Review of Surgical Options for Extensive Spinal Epidural Abscesses. J Clin Neurosci 2008;15:483-6. [Crossref] [PubMed]
- Urrutia J, Rojas C. Extensive epidural abscess with surgical treatment and long term follow up. Spine J 2007;7:708-11. [Crossref] [PubMed]
- Proietti L, Ricciardi L, Noia G, et al. Extensive Spinal Epidural Abscesses Resolved with Minimally Invasive Surgery: Two Case Reports and Review of the Recent Literature. Acta Neurochir Suppl 2019;125:345-53. [Crossref] [PubMed]
- Panagiotopoulos V, Konstantinou D, Solomou E, et al. Extended cervicolumbar spinal epidural abscess associated with paraparesis successfully decompressed using a minimally invasive technique. Spine (Phila Pa 1976) 2004;29:E300-3. [Crossref] [PubMed]
- Schultz KD Jr, Comey CH, Haid RW Jr. Technical note. Pyogenic spinal epidural abscess: a minimally invasive technique for multisegmental decompression. J Spinal Disord 2001;14:546-9. [Crossref] [PubMed]
- Ahuja K, Das L, Jain A, et al. Spinal holocord epidural abscess evacuated with double thoracic interval laminectomy: a rare case report with literature review. Spinal Cord Ser Cases 2019;5:62. [Crossref]
- Safavi-Abbasi S, Maurer AJ, Rabb CH. Minimally invasive treatment of multilevel spinal epidural abscess. J Neurosurg Spine 2013;18:32-5. [Crossref] [PubMed]
- Abd-El-Barr MM, Bi WL, Bahluyen B, et al. Extensive spinal epidural abscess treated with “apical laminectomies” and irrigation of the epidural space: report of 2 cases. J Neurosurg Spine 2015;22:318-23. [Crossref] [PubMed]
- Kurudza E, Stadler JA 3rd, Kurudza E, et al. Pediatric Holocord Epidural Abscess Treated with Apical Laminotomies with Catheter-directed Irrigation and Drainage. Cureus 2019;11:e5733. [Crossref] [PubMed]
- Hwang R, Yung BH, Sedney C, et al. Treatment of holocord spinal epidural abscess via alternating side unilateral approach for bilateral laminectomy. W V Med J 2015;111:14-16-8. [PubMed]
- Roberti F, Arsenault KL. The Use of a "Double-Triple Barrel" Technique during Minimally Invasive Multilevel Tubular Laminectomy. A Technical Note. J Neurol Surg A Cent Eur Neurosurg 2017;78:202-5. [PubMed]
- Di Rienzo A, Brunozzi D, Dobran M, et al. Skip Hemilaminectomy for Large, Multilevel Spinal Epidural Hematomas: Report of a Series of 11 Patients. World Neurosurg 2018;111:e933-e940. [Crossref] [PubMed]
- Yukawa Y, Kato F, Ito K, et al. Laminoplasty and Skip Laminectomy for Cervical Compressive Myelopathy: Range of Motion, Postoperative Neck Pain, and Surgical Outcomes in a Randomized Prospective Study. Spine (Phila Pa 1976) 2007;32:1980-5. [Crossref] [PubMed]
- Wipplinger C, Melcher C, Hernandez RN, et al. "One and a half" minimally invasive transforaminal lumbar interbody fusion: single level transforaminal lumbar interbody fusion with adjacent segment unilateral laminotomy for bilateral decompression for spondylolisthesis with bisegmental stenosis. J Spine Surg 2018;4:780-6. [Crossref] [PubMed]
- Kirnaz S, Wipplinger C, Schmidt FA, et al. Minimally Invasive Laminotomy for Contralateral "Over-the-Top" Foraminal Decompression Using 3-Dimensional Total Navigation: 2-Dimensional Operative Video. Oper Neurosurg (Hagerstown) 2020;19:E296. [Crossref] [PubMed]