
Patient-reported outcomes in spinal surgery—how can we keep getting better?
Atul Gawande, renowned author and compassionate surgeon himself, describes in his book “Better: a surgeon’s notes on performance” how doctors struggle to match their best intentions with best performance. He coined the phrase: “Better is possible. It does not take genius. It takes diligence. It takes moral clarity. It takes ingenuity. And above all, it takes a willingness to try” (1).
In line with Gawande’s thoughts, a strong tendency among most medical specialties to increase the focus on outcomes that matter to patients can be observed recently. Consequently, health related quality of life (HRQL) is measured with increased frequency to evaluate patients’ health status as well as medical performance. HRQL is a multidimensional construct covering physical, mental and social well-being of a person. Usually, information on HRQL comes directly from the patient without interpretation of a third person and is summarized under the umbrella term of patient-reported outcomes (PROs) (2). In the last decades, numerous patient-reported outcome measures (PROMs) have been developed and validated to measure HRQL for different populations, treatments and diagnoses.
In their annual Health at Glance report from 2017, the OECD defined robust outcome data as an essential prerequisite to achieve best possible care (3). Consequently, the OECD launched the Patient-Reported Indicators Surveys (PaRIS) Initiative aiming to promote people-centeredness of health care systems by defining, standardizing and supporting the measurement of quality and experience indicators that matter to people (4). Simple questions as ‘what good does the treatment do for the individual patient’, ‘will the patient be better off after adapting the medication plan’ or ‘will the patient be able to work again’ have become true challenges. Finding answers to those questions has become an urgent need for clinicians and health initiatives. These questions could be addressed efficiently and holistically by high-quality patient-centered data complementing classical medical outcome data. However, this requires the willingness to systematically collect PROs not only in clinical research but also in clinical practice. This data would facilitate comprehensive evaluation and comparison of relevant procedures to related outcomes and advance evidence-based medical decision making (5). Looking at spine treatments in the clinical routine, the ongoing discussion about conservative therapy vs. surgery is an area that could especially benefit from PROs to depict a holistic picture of the patient’s health after spine treatment.
Having the right measures in place can help minimizing the gap between “best intention” (1) and “best performance” (1), but what are the right measures? This staggering conflict can be solved by acknowledging the physician-patient mismatch of nearly one-fourth when it comes to defining success of an intervention (6). One answer to close this gap is: patient-centeredness. We have to ask patients to define what matters to them and then measure and subsequently set our achieved outcomes in context with the used resources, in order to know the value that we have created.
In the field of spine surgery, measurement of outcomes has undergone a fundamental evolution leading to an increased recognition and implementation of PROMs in observational studies as well as to a lesser extent in clinical trials (7). Already in 1980, the Oswestry Disability Index (ODI) version 1.0 has been introduced, a 10-item instrument specifically developed for patients with lower back pain aiming to quantify disability by focusing on pain and associated limitations, especially physical function (8). The trend towards recognizing the increasing importance of PROs is underlined by the rapid increase in the implication of the ODI which has more than tripled during a 10-year period from 2004–2014 (9). In the past decades, various instruments to measure PROs for patients with spinal problems have been developed for example the Cervical Spine Outcomes Questionnaire (CSOQ) or the Neck Disability Index (NDI) (10).
The variety of PROMs available in the field causes one major issue: comparability. Bhashyam et al. reported that 32 different PROMS were used to assess HRQL after a traumatic musculoskeletal injury (including spine and other musculoskeletal injuries) for the 20 studies included in their review (11). The use of different PROs assessing similar dimensions of health but applying different scorings and different metrics, made it impossible to compare the results and perform a comprehensive meta-analysis as envisioned.
The need for standardization of PROMs especially for patients with back pain was already stated in 1998 and is still shown to be relevant (12). To address the problem of missing comparability, different approaches have been undertaken to standardize outcome measurement. The International Consortium for Health Outcomes Measurement (ICHOM) is a non-profit organization striving for creating global standard sets by defining standardized sets of instruments to be used for various conditions such as low back pain in the field of musculoskeletal diseases (13). Thus, ICHOM defines not only what to measure in terms of PROs, but also provides guidance on how to measure these. Another promising approach to address this issue has been introduced by the Patient-Reported Outcomes Measurement Information System (PROMIS®) Initiative (14). A health domain framework with respect to HRQL was defined covering physical, mental and social health domains that are relevant for all individuals regardless of health condition. Corresponding to the developed framework, domain item banks were developed including items of established instruments and newly developed items that cover the continuum of respective domains. All items of one item bank were calibrated on one metric (T-metric) using item response theory (IRT) methods. Hence, it is possible to compare a score computed by use of three items of a domain to a score computed by 10, 15 or even one item of the same domain. Further, efforts linking legacy measures to PROMIS domains such as the Beck Depression Inventory (BDI) or the Patient Health Questionnaire-9 (PHQ-9) to the PROMIS Depression domain, enable to generate comparable scores by using the same metric while applying different PROMs (15).
Nevertheless, PROs now commonly used in research will be relevant in clinical routine but the challenge on how to integrate those in daily routine and measuring what matters to patients remains. An innovative concept that includes and links patient-centeredness and the measurement of PROs has been introduced by Porter and Teisberg in the book “Redefining Health Care: creating value-based competition on results” (16). In essence, their “strategy that will fix health care” restructures our way of care delivery in terms of “maximizing value for patients” (17) by “achieving the best outcomes at the lowest cost” (17). In order to quantify the value of a treatment for patients, Porter suggests the use of PROs. Besides measuring the value of a treatment, PROs can be applied for population surveillance, individual clinician interactions and research studies. The importance of contributing to patient-centered outcome research is especially evident when PROs are being linked to other clinical data thereby improving “care quality and patient outcomes by providing information” (18) that is of interest in regard to treatment and “emphasizing patient input to inform the research process” (18).
At the Charité University Hospital, Europeans largest university hospital, we are dedicated to promoting innovation in outcome measures in order to provide “proof-of-concept” for VBHC in terms of maximizing value for patients. A strategic reorientation has been launched defining the ambitious goal of measuring PROs for all of our patients by 2025, i.e., over 150,000 inpatients and nearly 700,000 outpatients, thereby encouraging other care providers to choose similar approaches (19). Following this line of thought, Charité University Hospital has started implementing PROMs in a variety of conditions, ranging from breast cancer, pregnancy and childbirth to musculoskeletal conditions. Already in 2016, a web-based system has been introduced to collect PROs at Charité Breast Center as part of a pilot project serving as a blueprint to further expand the PRO measurement to other disease entities and departments (20).
Charité’s spine center, renowned for their innovative and high-quality care delivery, proactively positioned themselves in the forefront of improving quality measures by pushing the implementation of PROs for their patients. Convinced that patient-centeredness is key to better outcomes, the spine center contributed enormously to the success of introducing PROMs at Charité by quickly adapting the corresponding ICHOM standard set complemented by additional PROMIS® Profile-29 to measure HRQL for their purpose.
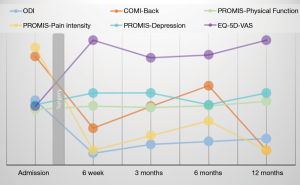
The procedure aims at covering all relevant outcomes thereby providing a holistic image of each individual: every patient who is seen in our outpatient clinic and either is admitted for surgery or followed-up through conservative care, gets a standardized set of PROMs at his/her first visit using an electronic data assessment tool. After being discharged, we follow-up on a predetermined schedule depending on the treatment and disease (in most cases at least after 3 and 6 months and yearly) via email, including a link to the questionnaire. In our Spine Center, we implemented the standard set recommended by ICHOM for Low Back Pain, the PROMIS® Profile-29 as well as the Core Outcome Measures Index (COMI)-Back and Neck recommended by the EuroSpine (13,14,21). These questions cover the most relevant domains of health for spine patients such as pain, physical functioning and mental well-being (13).
Immediately after completion, a report is generated and plotted longitudinal. Thus, it is possible to track the patients’ individual health trajectory. Figure 1 shows an exemplary patient journey after a surgery including the corresponding outcomes. In this way, clinicians can monitor the level of pain reported by patients, which might be high at admission, but will significantly decrease after surgery. The value of long-term monitoring becomes evident in regard to the changing scores in scope of time. Depicting measures that matter to patients on a regular basis offers the clinicians the chance to intervene when necessary and evaluate their own performance consequently leading to improved outcomes.
Health care systems are often described as being reluctant to change and innovation, which is partly assigned to the resistance of medical professionals and other important health care actors. In brief, forces affecting innovation efforts include players, funding, policy, technology, customers and accountability (22). However, the Spine Center and Charité’s overall efforts to promote PROMs demonstrate that innovation and imitation are speeding up. We witness that ambitious medical professionals enforce a rapid bottom-up development in terms of a “quality revolution” (23) as the work published by the Lancet Global Health Commission on High Quality Health Systems impressively shows. Innovation is happening as an increasing number of clinicians strive for acquiring information on their patients’ health outcomes and appreciate this data especially in terms of shared-decision-making. Therefore, framing the conditions and forces to foster innovation especially by providing the necessary tools for clinicians to evaluate and improve themselves as well as an overall openness to transparence on outcomes are crucial steps towards a system that focuses on value for patients.
To return to Atul Gawande’s thoughts. In our opinion, including the patient’s perspective in the evaluation of health care by use of PROs is crucial to get better. It does not take genius however needs diligence—enrolling and informing patients, motivating clinicians, nurses, and every other medical professional involved to come on board with this new and add-on activity. It does definitely require moral clarity, i.e., the willingness to become transparent on the results achieved and the possible harm inflicted, which might lead to change in practice standards consequently. It also requires ingenuity i.e., installing IT requirements for PRO collection in the remotest outpatient clinics, influencing policy makers and software vendors to demand and deliver standards on interfaces and interoperability such as FHIR/HL7b.
The willingness to just try and to cast aside doubts of feasibility is the biggest challenge. However, our medical obligation remains with changing treatment algorithms to assess outcomes that matter to patients with the most suitable and innovative tools.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Matthias Pumberger) for the series “Postoperative Spinal Implant Infection (PSII)” published in Journal of Spine Surgery. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jss-20-582). The series “Postoperative Spinal Implant Infection (PSII)” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gawande A. Better: a surgeon’s notes on performance. 1st ed. New York: Picador, 2008.
- U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), et al. Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims: Guidance for Industry. 2009. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/patient-reported-outcome-measures-use-medical-product-development-support-labeling-claims
- OECD. Health at a Glance 2017. Available online: https://www.oecd.org/social/health-at-a-glance-19991312.htm
- OECD. Patient-Reported Indicators Surveys (PaRIS). Available online: https://www.oecd.org/els/health-systems/paris.htm
- Black N.. Patient reported outcome measures could help transform healthcare. BMJ 2013;346:f167. [Crossref] [PubMed]
- Schwartz CE, Ayandeh A, Finkelstein JA. When patients and surgeons disagree about surgical outcome: investigating patient factors and chart note communication. Health Qual Life Outcomes 2015;13:161. [Crossref] [PubMed]
- Finkelstein JA, Schwartz CE. Patient-reported outcomes in spine surgery: past, current, and future directions. J Neurosurg Spine 2019;31:155-64. [Crossref] [PubMed]
- Fairbank JC, Couper J, Davies JB, et al. The Oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271-3. [PubMed]
- Guzman JZ, Cutler HS, Connolly J, et al. Patient-reported outcome instruments in spine surgery. Spine (Phila Pa 1976) 2016;41:429-37. [Crossref] [PubMed]
- McCormick JD, Werner BC, Shimer AL. Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg 2013;21:99-107. [Crossref] [PubMed]
- Bhashyam AR, van der Vliet QMJ, Ochen Y, et al. Injury-related variation in patient-reported outcome after musculoskeletal trauma: a systematic review. Eur J Trauma Emerg Surg 2020;46:777-87. [Crossref] [PubMed]
- Deyo RA, Battie M, Beurskens AJ, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 1998;23:2003-13. [Crossref] [PubMed]
- Clement RC, Welander A, Stowell C, et al. A proposed set of metrics for standardized outcome reporting in the management of low back pain. Acta Orthop 2015;86:523-33. [Crossref] [PubMed]
- Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol 2010;63:1179-94. [Crossref] [PubMed]
- Choi SW, Schalet B, Cook KF, et al. Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression. Psychol Assess 2014;26:513-27. [Crossref] [PubMed]
- Porter ME, Teisberg EO. Redefining health care: creating value-based competition on results. 1st ed. Boston: Harvard Business School Press, 2006.
- Porter ME, Lee TH. The strategy that will fix health care. Harvard Business Review 2013;91:24.
- Snyder CF, Jensen RE, Segal JB, et al. Patient-reported outcomes (PROs): putting the patient perspective in patient-centered outcomes research. Med Care 2013;51:S73-9. [Crossref] [PubMed]
- Insights: annual report 2018. Berlin: Charité-Universitätsmedizin Berlin, 2018.
- Karsten MM, Speiser D, Hartmann C, et al. Web-based patient-reported outcomes using the international consortium for health outcome measurement dataset in a major German university hospital: observational study. JMIR Cancer 2018;4:e11373. [Crossref] [PubMed]
- Fankhauser CD, Mutter U, Aghayev E, et al. Validity and responsiveness of the Core Outcome Measures Index (COMI) for the neck. Eur Spine J 2012;21:101-14. [Crossref] [PubMed]
- Herzlinger RE. Why innovation in health care is so hard. Harv Bus Rev 2006;84:58-66, 156. [PubMed]
- Kruk ME, Larson E, Twum-Danso NA. Time for a quality revolution in global health. Lancet Glob Health 2016;4:e594-6. [Crossref] [PubMed]


