
Occipital condyle screws: indications and technique
Introduction
Occipitocervical instability is a rare potentially life threatening and disabling disorder caused by a myriad of pathologies such as congenital malformations, trauma, infections, tumors, rheumatoid arthritis and degenerative conditions, wherein immediate reconstruction of the occipitocervical junction (OCJ) to regain its stability is of paramount importance (1). Occipitocervical fusion is used to restore the biomechanical stability of the OCJ. Stabilization of the OCJ remains a challenge. For many years, surgical stabilization of craniocervical junction, has primarily depended on occipital squama-based fixations (2). The options available for anchorage in the cephalad part of the construct in occipitocervical fixation systems are limited by the complex topographical anatomy of the craniocervical junction and the critical neurovascular structures in the vicinity. With the availability of modern spinal implant systems, intra-operative image guidance and the advent of intraoperative image-guided navigation, it is possible to access areas that were previously considered difficult to be accessed or unsuitable for implant anchorage. The occipital condyle (OC) through its articulation with the superior facet of the C1 lateral mass, plays a pivotal role in maintaining the stability at the OCJ. Recently, La Marca et al. and Uribe et al. described a novel method of segmental occipitocervical stabilization by utilizing the OCs for screw anchorage (3-5). Although this is not a common technique for occipital stabilization, it may be required in specific situations. We describe the indications, biomechanical and technical considerations, preoperative planning, surgical technique, complications, advantages and limitations of occipital condyle screw (OCS) based occipitocervical fixation.
Prerequisites of an ideal fixation system for stabilizing the OCJ
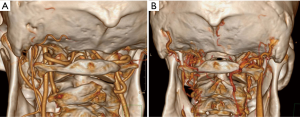
The OCJ forms the most cranial part of the neuraxis, extending from the occiput to the second cervical vertebra. The C0-C1 articulation allows significant movement in the sagittal plane, while simultaneously maintaining the anatomical integrity and stability (4). A sound knowledge of the intricate osseoligamentous and neurovascular anatomy ( Figure 1) and the biomechanics of the OCJ is imperative to develop an ideal implant system to address the instability at the OCJ. The ideal system for stabilizing the craniocervical junction should fulfill these criteria (6): (I) it should provide rigid segmental stabilization; (II) no spinal canal compromise by hardware; (III) it should facilitate immediate correction of the deformity and maintain stability till the occurrence of bony fusion, without the need for external immobilization after surgery; (IV) must be useful in stabilizing the OCJ even in scenarios where the posterior elements and occipital plate are deficient or compromised.
Anatomical considerations for OCS placement
The paired OCs are the key anatomical structures which render stability while maintaining significant mobility at the craniocervical junction by forming the occipitoatlantal (O-C1) joints with the superior facet of lateral masses of atlas. Successful exposure and preparation of the OCs for screw placement requires an in-depth knowledge of the osseous anatomy of the OCJ and its relationship with the neurovascular structures in its vicinity namely, the vertebral arteries, spinal canal, hypoglossal canal (HC) and the jugular foramen (7).
The OCs project from the undersurface of the lateral part of the occipital bone. The OCs lie anterolateral to the foramen magnum. They are on an average, 23.6 mm (range, 16.7 to 30.6 mm) long, 10.5 mm (range, 6.5 to 15.8 mm) broad, 9.2 mm (range, 5.8 to 18.2 mm) tall. The OCs are oval (in more than half of the population) and converge ventrally with a mean angulation of thirty degrees (10 to 54 degrees) to the sagittal plane (8,9). Laterally, the lateral atlantooccipital ligament and the rectus capitis lateralis muscle separate the OC from the jugular foramen and its contents (the internal jugular vein and cranial nerves IX, X, XI) (8,10). The HC and the jugular tubercle lie cranial to the OC while the inferior surface of the OC articulates with the superior facet of C1 forming the atlantooccipital joint.
The condylar fossa is a concave depression lying posterosuperior to the OC ( Figure 2A) . The condylar fossa contains the posterior condylar foramen through which the posterior condylar emissary vein (PCEV) communicates posteriorly with the deep cervical vein and horizontal portion of the vertebral artery venous plexus and drains anteriorly into the superior bulb of the internal jugular vein and sigmoid sinus ( Figure 2B,C) (11,12). An important step in surgical exposure is to identify the PCEV, which defines the lateral extent of dissection, and is imperative to avoid profuse bleeding during surgery. The PCEV is located 8-10 mm cranial to the inferior surface of the OC (3).
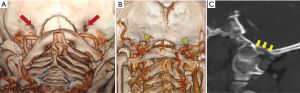
The V3 segment of vertebral artery along with the dense network of veins surrounding it, rests on the superior surface of posterior arch of the atlas within the sulcus arteriae vertebralis. It must be identified early through meticulous exposure along the posterior arch of C1 vertebra, where the artery turns medially around the posterior surface of the lateral mass of C1 vertebra ( Figure 3A,B) . The artery and its venous plexus are protected with cottonoids and by gentle inferior retraction during condylar screw insertion. Meticulous care must be taken to protect the V3 segment of vertebral artery throughout its extradural course till it pierces the spinal dura and arachnoid to continue as V4.
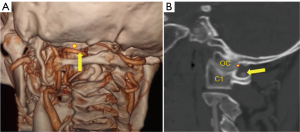
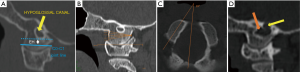
The HC contains the hypoglossal nerve, which passes in an anterolateral direction just above the base of the OC. It is embryologically homologous to the intervertebral foramen (13). The HC lies cranial to a horizontal plane passing through condylar emissary vein foramen. The vertical height from the undersurface of the HC to the undersurface of the OC was variable (9.1 to 11.5 mm), but adequate for safe insertion of an OCS (7,8). A more relevant parameter is the presence of an effective height (EH) for passage of a 3.5 mm diameter occipital condyle screw along the safe corridor situated between the inferior surface of the HC above and C0-C1 joint line below ( Figure 4A) . Allowing a safety margin of 1 mm, an EH of at least 4.5 mm must be available for safe placement of an OC screw (7).
Biomechanical considerations and their implications
- Occipitocervical stabilization with OC screws as the cranial anchors has been shown to be biomechanically equivalent to the standard occipitocervical plate/rod system (14-16).
- The OCS (20 to 24 mm intraosseous) being longer than occipital screws (10 to 14 mm) have better pull out strength and greater tolerance to higher screw loads (16). This would decrease complications like screw loosening, implant breakage, construct failure and obviate the need for multiple occipital fixation points.
- Occipitocervical fusion using the technique of occipital condylar fixation with OCs as the cephalad anchors has several technical advantages. It obviates the need for rod bending to negotiate the sharp angulation of the craniocervical junction.
- Since OCS are in alignment with C1 lateral mass screws and C2 pars/pedicle screws, it allows easy accommodation of the rod into screw heads in a C0-C1-C2 construct.
- The lateral placement of OCSs allows creation of two parallel occipital condylar cervical constructs which are in alignment with the lateral masses. This results in an increase in the effective moment arm of the construct with resultant decrease in the rate of implant failure (17).
- Occipital condylar cervical fixation is a lower profile construct leaving generous occipital surface area for bone grafting and osseous fusion, while preventing complications related to wound healing (16).
- OCS can be incorporated into the traditional occipital plate-rod construct and can be used to augment the standard occipital plate-C1-C2 construct.
Indications for OCS placement
There is limited evidence in the literature, to suggest the use of OCs screws as the primary option or the sole cranial fixation points for craniocervical stabilization (18). In certain distinct scenarios like posterior fossa craniectomy (for foramen magnum decompression, removal of posterior fossa tumors or hematoma) with deficiency of occipital squama for screw placement, malignancy and infection of occipital squama (poor screw purchase in the diseased occipital bone) and in revision surgery for failed occipital squama-based craniocervical stabilization, occipital plate-based instrumentation is not feasible. In these scenarios, OCS can be used as salvage cephalad anchors. They can also be used as additional augmentative anchors in a standard occipital plate-screw-rod construct.
Preoperative planning
A sound knowledge of the anatomical and radiological landmarks is imperative before contemplating an OCS placement. A thin slice computed tomography (CT) scan of the OCJ in the axial, coronal and sagittal planes along with multiplanar three-dimensional reconstructions is essential to study the bony anatomy of the OCJ and anatomical variations if any ( Figure 4B,C,D) (7). The size, orientation, and integrity of the OCs are assessed. The safe screw length for placement of a screw along the planned trajectory with bicortical purchase was measured. The space available between the base of the occipital bone and upper surface of the posterior arch of C1 is an important parameter which dictates feasibility of OCS placement (18). The position of the HC and the EH available for OCS placement are analyzed. A CT angiography of the OCJ is mandatory to assess the relationship of the condyles to its neurovascular neighborhood (vertebral artery, PCEV, hypoglossal nerve, jugular bulb) and to identify any variations in the normal anatomy (Figure 4D).
Patient positioning
Owing to the highly unstable nature of diseases at the OCJ, patient’s cervical spine is protected with a Philadelphia collar or halo fixation while shifting to the operating room. Surgery is performed under general endotracheal anaesthesia and intraoperative neuromonitoring, along with EMG monitoring of both hypoglossal nerves. Patients are intubated using a flexometallic endotracheal tube. In cases of severe cervical canal compromise, a fiber-optic laryngoscope is used for intubation without hyperextending the cervical spine. Afterward patients are positioned prone on a radiolucent spinal table, with the head supported in a Mayfield head holder. It is ensured that the cervical spine is neutrally aligned using an image intensifier. The head is then placed in slight flexion for better exposure of the CVJ. In patients with atlantooccipital dislocation, reduction is achieved and maintained using skull tong traction. Screw placement is performed under fluoroscopic guidance or neuronavigation.
Surgical technique
Exposure
A standard posterior-midline skin incision is made from the inion to the spinous process of the caudad cervical vertebra to be instrumented. Deep dissection is carried down up to the spinous process by dividing the ligamentum nuchae in the midline. The occipital squama, laminae of C1,C2 and the exposed subaxial cervical vertebrae were exposed by stripping the paraspinal muscles in a subperiosteal fashion. The horizontal segment of the vertebral artery is identified by continuing the subperiosteal dissection laterally from the midline along the superior surface of posterior arch of C1. Caution must be exercised to protect the artery and its surrounding plexus of veins. The atlantooccipital membranes, ligamentum flavum and the laminae of C2 and C3 are exposed by blunt dissection. This is followed by exposure of the lateral masses of the first and second cervical vertebra for placing C1 lateral mass screws and C2 pars/pedicle screws. Exposure of the subaxial cervical lateral masses is performed as needed for placing lateral mass screws (18).
The atlantooccipital membrane is carefully dissected from the foramen magnum in a medial to lateral direction, using curette till the medial border of the OC is reached. Dissection is carried out laterally along the condylar fossa while staying on the occipital bone, taking care to avoid injury to the V3 segment of vertebral artery, until the PCEV is identified, which defines the lateral most extent of dissection (18). Meticulous dissection is carried out to avoid injuring the PCEV which can cause profuse bleeding (12). C1 lateral mass screws and C2 pedicle/pars interarticularis screws were placed as described in literature (19,20). Initial placement of the C1 lateral mass screws gives an idea of the approximate location and orientation of the OCs as they form the superior articulating surface of the C0-C1 joint.
The condylar entry point (CEP) is identified using anatomic and radiographic/fluoroscopic landmarks. The condylar emissary vein foramen, the foramen magnum and the superior articular facet of atlas are identified as important cranial, medial and caudal anatomical landmarks for identifying the entry point of OCS.
La Marca technique
The CEP is about 3 mm inferior to the condylar emissary vein foramen, along the middle of the posterior surface of the OC. The lateral margin of the OC is established by an imaginary line extending cranially along the lateral border of the occipitoatlantal joint capsule, while the medial margin to be the posterolateral edge of the foramen magnum. A pilot hole is made at the entry point defined by a combination of anatomic landmarks and fluoroscopic guidance, after protecting the horizontal segment of the vertebral artery using cottonoids and by inferior retraction. The planned trajectory for screw placement was, 30 degrees caudad and 10 degrees medial to avoid injury to the HC and the jugular foramen, respectively (3). Using fluoroscopic guidance, the holes were drilled to the depth determined preoperatively using CT scan. Tapping of the holes was done using a 3.5 mm tap and probed to rule out cortical breach. A screw of 22 mm length and 3.5 mm diameter was inserted into the OC.
Uribe technique
The entry-point for OCS is made, 5 mm lateral to the posteromedial corner of the OC at the midpoint of its posterior surface using an awl and is confirmed with fluoroscopy or free hand navigation (4). The planned trajectory for screw placement is: 15 degrees of medial angulation in the axial plane and 5 degrees of cranial angulation in the sagittal plane. Drilling is performed under fluoroscopic or navigational guidance with continuous hypoglossal nerve EMG monitoring with slow advancements till the anterior cortex of the OC was penetrated, typically at a length of 20 mm (5). Screw length is calculated preoperatively using CT scan and confirmed intraoperatively using a probe and fluoroscopic imaging. After tapping the hole, a 3.5 mm diameter polyaxial shank screw of predetermined length is inserted bicortically. Approximately, 9–12 mm of unthreaded portion should remain superficial to the posterior cortex of the OC, to allow the screw tulip to remain above the posterior arch of C1 in alignment with the rest of the construct to avoid compromise of vertebral artery by rods. Implant position is confirmed with fluoroscopy/intraoperative navigation and hypoglossal nerve integrity is checked with EMG stimulation.
Rod construct (C0-C1-C2 construct with or without subaxial lateral mass screws) is completed bilaterally. Autografts/allografts are laid on the prepared fusion bed. Closure is performed in layers over a subfascial drain. Post procedure CT scan and radiographs of the cervical spine are performed to confirm implant position.
Table 1 shows the safe trajectories and screw lengths described in literature for placement of OCS.

Full table
Complications and tips to avoid them
Many authors have described the possible complications that might be encountered during each stage of occipitocervical stabilization using the OCS fixation technique. Table 2 highlights the complications that must be foreseen while performing this technique and provides tips to avoid them.
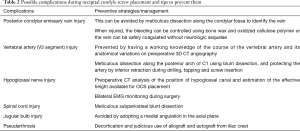
Full table
Conclusions
OCSs are feasible alternative or salvage cranial anchors for occipitocervical stabilization, where occipital squama-based fixations are not feasible. The indications for their use are limited and rather specific. The technique of OCS placement has a steep learning curve. Due to the complex bony and vascular anatomy of the OCJ, a detailed preoperative assessment using multislice computed tomography scan including 3D-CT angiography before screw placement. Navigational guidance, will be a valuable aid for safe placement of these screws. The preoperative planning strategies and the surgical techniques presented here will be a valuable aid in guiding the spine surgeon during placement of OCSs.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. ISA served as the unpaid Guest Editor of the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wertheim SB, Bohlman HH. Occipitocervical fusion. Indications, technique, and long-term results in thirteen patients. J Bone Joint Surg Am 1987;69:833-6. [Crossref] [PubMed]
- Winegar CD, Lawrence JP, Friel BC, et al. A systematic review of occipital cervical fusion: techniques and outcomes. J Neurosurg Spine 2010;13:5-16. [Crossref] [PubMed]
- La Marca F, Zubay G, Morrison T, et al. Cadaveric study for placement of occipital condyle screws: technique and effects on surrounding anatomic structures. J Neurosurg Spine 2008;9:347-53. [Crossref] [PubMed]
- Uribe JS, Ramos E, Vale FL. Feasibility of occipital condyle screw placement for occipitocervical fixation: a cadaveric study and description of a novel technique. J Spinal Disord Tech 2008;21:540-6. [Crossref] [PubMed]
- Uribe JS, Ramos E, Baaj A, et al. Occipital cervical stabilization using occipital condyles for cranial fixation: technical case report. Neurosurgery 2009;65:E1216-7. [Crossref] [PubMed]
- Grob D, Dvorak J, Panjabi M, et al. Posterior occipitocervical fusion. A preliminary report of a new technique. Spine 1991;16:S17-24. [Crossref] [PubMed]
- Bosco A, Venugopal P, Shetty AP, et al. Morphometric evaluation of occipital condyles: defining optimal trajectories and safe screw lengths for occipital condyle-based occipitocervical fixation in Indian population. Asian Spine J 2018;12:214-23. [Crossref] [PubMed]
- Muthukumar N, Swaminathan R, Venkatesh G, et al. A morphometric analysis of the foramen magnum region as it relates to the transcondylar approach. Acta Neurochir (Wien) 2005;147:889-95. [Crossref] [PubMed]
- Naderi S, Korman E, Citak G, et al. Morphometric analysis of human occipital condyle. Clin Neurol Neurosurg 2005;107:191-9. [Crossref] [PubMed]
- Suchomel P, Choutka O, Barsa P. Surgical anatomy. In: Suchomel P, Choutka O. editors. Reconstruction of upper cervical spine and craniovertebral junction. Springer-Verlag, Berlin, Heidelberg; 2011:3-15.
- de Oliveira E, Rhoton AL Jr, Peace D. Microsurgical anatomy of the region of the foramen magnum. Surg Neurol 1985;24:293-352. [Crossref] [PubMed]
- El-Gaidi MA, Eissa EM, El-Shaarawy EA. Free hand placement of occipital condyle screws: a cadaveric study. Eur Spine J 2014;23:2182-8. [Crossref] [PubMed]
- Bono CM, Park WW, Garfin S. Development of the spine. In: Herkowitz H, Garfin S, Eismont F, et al. editors. Rothman-Simeone The Spine. 5th edn. Philadelphia: Saunders, 2006:3-15.
- Helgeson MD, Lehman RA Jr, Sasso RC, et al. Biomechanical analysis of occipitocervical stability afforded by three fixation techniques. Spine J 2011;11:245-50. [Crossref] [PubMed]
- Takigawa T, Simon P, Espinoza Orias AA, et al. Biomechanical comparison of occiput-C1-C2 fixation techniques: C0-C1 transarticular screw and direct occiput condyle screw. Spine (Phila Pa 1976) 2012;37:E696-701. [Crossref] [PubMed]
- Uribe JS, Ramos E, Youssef AS, et al. Craniocervical fixation with occipital condyle screws: biomechanical analysis of a novel technique. Spine (Phila Pa 1976) 2010;35:931-8. [Crossref] [PubMed]
- Oda I, Abumi K, Sell LC, et al. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine (Phila Pa 1976) 1999;24:2377-82. [Crossref] [PubMed]
- Ahmadian A, Dakwar E, Vale FL, et al. Occipitocervical fusion via occipital condylar fixation: a clinical case series. J Spinal Disord Tech 2014;27:232-6. [Crossref] [PubMed]
- Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 2001;26:2467-71. [Crossref] [PubMed]
- Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47-53. [Crossref] [PubMed]


