
Hybrid decompression and reconstruction technique for cervical spondylotic myelopathy: case series and review of the literature
Background
Cervical spondylotic myelopathy (CSM) is the most common cause of non-traumatic spinal cord dysfunction in adults (1). Based on the progressive natural history of this disorder, the primary management of patients with CSM remains prompt surgical intervention for neural decompression (2). While there is an abundance of evidence highlighting the effectiveness of surgery in improving patient outcomes, there remains considerable variability in the specific surgical approaches utilized. Fehlings et al. found a nearly two-fold difference in the frequency of anterior versus posterior cervical decompression surgeries utilized in Europe and Latin America (3). When dealing with multilevel CSM, the spectrum of operative considerations increases even further. Within the context of anterior cervical decompression, options have traditionally been between multiple anterior cervical discectomy and fusion (ACDF) versus anterior cervical corpectomy fusion (ACCF) depending on certain radiographic features (2). However, a growing number of studies have looked at various hybrid surgery (HS) models aimed at maximizing the benefits of these surgical techniques (4,5). Previous reviews of the literature on surgical management of multilevel CSM have been limited to clinical studies to reduce the heterogeneity of data. There are, however, biomechanical and radiographic studies that can provide additional insights for the decision-making process (6-8).
The purpose of this study was to review the evidence on the clinical and biomechanical outcomes of cervical fusion hybrid decompression and reconstruction techniques in patients with multilevel CSM and characterize preoperative patient variables that may benefit from a hybrid technique.
Methods
Case series
A retrospective review was performed on consecutive patients who received hybrid anterior decompression and reconstruction at Rush University between 2013–2018. The inclusion criteria were: (I) adult patients (≥18 years) with a new diagnosis of CSM; (II) preoperative MRI confirming multilevel disease; (III) underwent hybrid decompression and reconstruction surgery. Patients with other indications for surgery such as spine tumor, infection and trauma were excluded. This study was approved by the Rush University Institutional Review Board (19070801-IRB01-AM01).
Data abstraction was obtained from hospital and clinic records and included patient demographics, clinical, and radiographic variables. Preoperative consultation notes were examined to identify specific surgical indications and operative approaches considered by the surgeons. Imaging analysis consisted of preoperative cervical spine MRI and a postoperative cervical spine X-ray. Radiographs were digitally analyzed using PACS software for the sagittal Cobb angle (angle between inferior endplates of C2 and C7). Preoperative and postoperative patients’ health status was measured using patient-reported outcomes (PRO) including a visual analogue scale for neck pain (VAS) and modified Japanese Orthopedic Association scale (mJOA). Lastly, the cases were individually reviewed with the primary surgeon to confirm their reasons for choosing the hybrid technique.
Surgical technique
The traditional anterior approach to the cervical spine was utilized for all of the cases. Patients were positioned supine with the head supported in a donut headrest and neck slightly extended. While not necessary in our case series, surgeons in our institution regularly utilize Gardner-Wells tongs connected to weights at the head of the bed for additional distraction. To improve intraoperative fluoroscopic visualization, patients’ shoulders were taped and pulled caudally. For all of the cases, a transverse incision was planned centered at the corpectomy level using an intraoperative X-ray. The preferred side of surgery for the cervical spine remains a contentious topic with some surgeons emphasizing higher risk to the recurrent laryngeal nerve associated with the right-sided surgery. Anecdotal experience at our institution, where both right and left-sided surgeries are regularly performed, does not provide support for preferential use of left-sided surgery.
For all of the cases, a generous subplatysmal dissection prior to fascial dissection allowed adequate surgical exposure through a transverse incision without postoperative dysphagia. Blunt dissection through the superficial and deep cervical fascia was performed following the anterior border of the sternocleidomastoid muscle with the carotid sheath positioned laterally and trachea and esophagus medially. After identifying the prevertebral fascia, subperiosteal dissection of the longus colli bilaterally was performed prior to retractor positioning. With the index vertebra with the greatest canal narrowing confirmed on intraoperative fluoroscopy, standard discectomy at the cranial and caudal levels were performed with a combination of high-speed drill and Kerrison punches. Discectomy at the adjacent level for the ACDF was performed at the same time. With the uncinate processes exposed, corpectomy was then performed with removal of greater than 80% of the vertebral body leaving narrow columns of bone laterally to project the vertebral arteries. After completion of the bony resection, careful resection posterior longitudinal ligament was performed to ensure decompression of the neural elements. The anterior column reconstruction was performed using various strut graft options, including allograft, PEEK, titanium mesh cage, or carbon fiber cage. All of the cases were supplemented with an anterior cervical plate spanning both corpectomy and discectomy levels. Screws for the cervical plate were placed aiming for bicortical purchase to ensure maximal pullout strength. Postoperatively, cervical collars were utilized only in two cases with poor bone quality and screw purchase.
Systematic review and meta-analysis
We performed a systematic review of the literature using PubMed, the Cochrane Library, Scopus, and included citations to identify clinical studies on hybrid decompression and reconstruction techniques in patients with three-level CSM. The systematic review and meta-analysis were conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. Specific MeSH terms and keywords including “anterior cervical hybrid fusion”, “hybrid surgery”, “corpectomy combined with discectomy”, “anterior cervical corpectomy and fusion”, “vertebrectomy”, “anterior cervical discectomy and fusion”, “cervical spondylosis”, and “cervical spondylotic myelopathy” were used to identify studies of interest. Additional manual searches through cited references were performed.
Studies were included in meta-analysis if they met the following criteria: (I) cohort or case-control comparative studies; (II) patients with 3-level CSM; (III) studies comparing the clinical outcomes of the hybrid fusion technique versus ACCF and/or versus ACDF; (IV) outcome assessments included duration of surgery, blood loss, surgical complications, fusion rate, radiographic outcomes including measured C2-7 lordosis, patient-related outcomes included mJOA score, Neck Disability Index (NDI). Studies were excluded if they involved (I) posterior surgical approaches, (II) inclusion of cervical arthroplasty within analysis, (III) 4 level CSM or surgery on non-contiguous levels, (IV) mean follow-up less than 1 year (V) if full-text articles could not be obtained, (VI) non-English publications, editorials, conference abstracts, errata, book chapters, and case reports were excluded.
Statistical analysis
Descriptive statistics was performed to characterize patient demographic, clinical, and surgical data in our case series using STATA 14.3 (StataCorp LLC, College Station, Texas, 2018). Statistical analysis for the systematic review and meta-analysis was performed using RevMan 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). An I2 test was performed for each study to test statistical heterogeneity. An I2>50% was considered to indicate substantial heterogeneity and a random-effects model was used for meta-analysis. When I2 was less than 50% a fixed-effects model was used. An odds ratio and 95% confidence interval were calculated for dichotomous outcomes whereas a standardized mean difference and 95% confidence interval were calculated for continuous outcomes. A P value <0.5 was considered to be statistically significant.
Results
Case series
After reviewing the charts of patients who received corpectomy between 2013 to 2018, a total of 10 patients met the inclusion criteria. The mean age of the patients was 66 (range, 57–90) years old consisting of 4 females and 6 males. Their preoperative BMI ranged from 21.5 to 38.9 with an average of 28. Of the 10 patients, the most frequent medical comorbidities were hypertension (n=10), dyslipidemia (n=6), and diabetes (n=4). Two patients were active smokers at the time of the procedure.
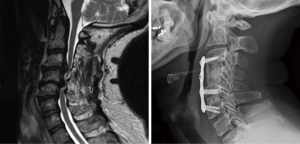
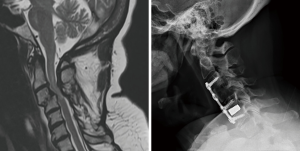
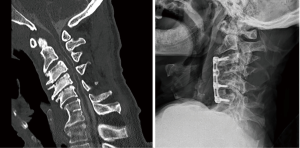
In determining the specific surgical approach, the most common indication for corpectomy over multiple discectomies was the presence of stenosis posterior to the vertebral body due to caudally or cranially herniated disc or thickened/calcified posterior longitudinal ligament (Figure 1). Other reasons included short segment kyphotic deformity and spondylolisthesis (Figure 2). In addition, these patients underwent a hybrid technique of corpectomy and discectomy over two-level corpectomies to allow three levels of fixation. There were two cases where the hybrid technique was used to address a single degenerated mobile segment between the corpectomy level and auto-fused vertebrae two levels adjacent to it (Figure 3). Two out of 10 patients were placed in cervical collars after surgery. The duration of postoperative cervical immobilization of these patients was between 6 and 12 weeks.
Clinical data and details of the surgical intervention are summarized in Table 1. The average surgical blood loss was 107.5 mL (range, 50–200 mL). The average postoperative sagittal Cobb angle was 11.8 degrees lordotic (range, 2.5–29.6). The overall complication rate was 40% with 2/10 patients experiencing transient postoperative dysphagia, 1/10 patients experiencing a myocardial infarction during hospitalization, and 1/10 patients developing an epidural fluid collection requiring surgical decompression. One patient required additional posterior decompression and instrumentation due to persistent stenosis during initial hospitalization. Five patients had a postoperative follow-up longer than 1 year. At the end of the follow-up period, no one developed symptomatic pseudoarthrosis requiring additional surgical intervention. The postoperative PRO showed an average VAS of 1.8 (range, 0–4) and average mJOA of 11 (range, 6–14).

Full table
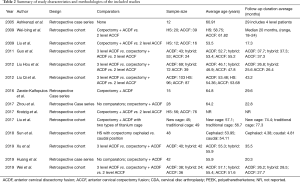
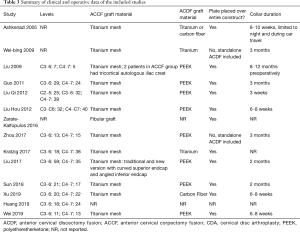
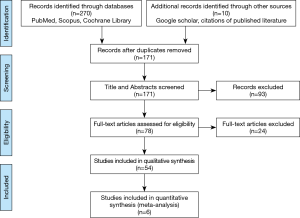
Systematic review
In total, 171 abstracts were reviewed of which 93 were excluded. Seventy-eight full-text articles were assessed of which 24 were excluded. Several articles were excluded for including arthroplasty within the HS group (9-28). Articles were also excluded if they included HS for 4 level CSM, or if they included non-contiguous constructs (29-32). Fourteen manuscripts including both case series of hybrid fusion constructs as well as retrospective cohorts comparing hybrid fusion to ACDF and/or ACCF are summarized in Table 2 with operative data regarding hybrid fusion summarized in Table 3 (5,8,33-44). Of these, six manuscripts met the predefined inclusion criteria for meta-analysis with data summarized in Table S1 (5,34,36,37,42,43). A flow chart of study inclusion and exclusion is shown in Figure 4 (45).
Full table
Full table

Full table
Meta-analysis
Of the six retrospective cohorts included in meta-analysis, only four studies included all three surgical arms of three-level ACDF, hybrid fusion, and two-level ACCF (5,36,37,43). Liu et al. 2009 compared patients undergoing hybrid fusion and patients undergoing two-level ACCF whereas Xu et al. 2019 compared patients undergoing hybrid fusion and patients undergoing three-level ACDF (34,42). The six eligible studies were published between 2009 and 2019 and included 293 patients undergoing three-level ACDF, 299 patients undergoing hybrid fusion, and 202 patients undergoing two-level ACCF. The average follow-up ranged from 17.3 to 43.2 months. The average age of patients undergoing each procedure ranged from 46.1 to 57.1 years, 46.9 to 55.9 years and 47.8 to 55.2 years for ACDF, hybrid fusion, and ACCF respectively. All patients undergoing corpectomies in the included manuscripts had placement of titanium mesh grafts except for 2 patients in Liu et al. 2009 who underwent placement of autologous iliac crest. Polyetheretherketone (PEEK) grafts were used in all patients during ACDF except for in Xu et al. 2019 where carbon fiber grafts were favored. All patients had complete coverage of their construct with a titanium plate; no stand-alone grafts were included in the meta-analysis. All studies reported collar duration which ranged from 3 weeks postoperatively in Liu, Qi, et al. 2012 to 3 months in Guo et al. 2011. Liu et al. 2009 was the only study to discuss preoperative collar placement which ranged from 8–12 months.
Operative time
Four studies compared operative time in ACDF and hybrid fusion showing no significant difference in operative time between the two groups (SMD 0.22; 95% CI, −0.57, 1.01; P=0.59). Similarly, three studies comparing operative time in hybrid fusion and ACCF found no significant difference in operative time between the two groups (SMD 0.35; 95% CI, −0.71, 1.4; P=0.52).
Blood loss
Four studies compared blood loss in ACDF and hybrid fusion with significantly less estimated blood loss ranged in the ACDF group (102.3–172.1 mL) than in the hybrid group (141.3–193.2 mL) (SMD −1.34; 95% CI, −2.39, −0.30; P=0.01). Three studies compared blood loss in hybrid fusion and ACCF showing a statistically significant reduction in blood loss in the hybrid group than in the ACCF group (SMD −0.61; 95% CI, −0.88, −0.34; P<0.00001).
Cervical lordosis
Four studies compared C2–7 cervical lordosis at follow-up in ACDF and hybrid fusion. The mean cervical lordosis in the ACDF group was similar to the hybrid group (14.9–24.27 degrees vs. 12.8–23.21 degree, respectively; SMD 0.26; 95% CI, −0.23, 0.75; P=0.31). Three studies compared C2–7 cervical lordosis at follow-up in hybrid fusion and ACCF. The mean cervical lordosis ranged from 17.3 degrees to 23.21 degrees in the hybrid group and 11.4 degrees to 15.63 degrees in the ACCF group. With an I2 of 0%, a fixed-effects model meta-analysis was used and there was a statistically significant increased C2–7 cervical lordosis at follow-up in the hybrid fusion group compared to the ACCF group (SMD 0.76; 95% CI, 0.49, 1.03; P<0.00001).
Change in cervical lordosis from preoperative to follow-up in ACDF and hybrid fusion was compared in three studies. The mean change in cervical lordosis in the ACDF group was statistically higher than in the hybrid group (4.9–15.1 vs. 1.8–8.1 degrees, respectively; SMD 0.56; 95% CI, 0.14, 0.99; P=0.009). Change in cervical lordosis from preoperative to follow-up in hybrid fusion and ACCF was compared in two studies. The mean change in cervical lordosis ranged from 4.5 to 8.1 degrees in the hybrid group and 1.7 to 2.7 degrees in the ACCF group. There was a statistically significant increased change in C2–7 cervical lordosis in the hybrid fusion group compared to the ACCF group (SMD 1.09; 95% CI, 0.71, 1.46; P<0.00001).
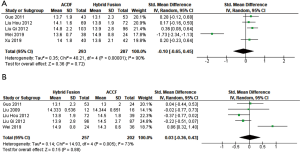
Patient reported outcomes
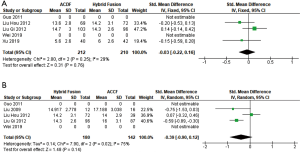
Five separate studies compared JOA score at follow-up in ACDF and hybrid fusion with comparable mean JOA score at follow-up ranged from 13.6 to 14.8 in the ACDF group and 13.1 to 14.9 in the hybrid group (SMD −0.10; 95% CI, −0.65, 0.45; P=0.72) (Figure 5A). Five separate studies compared JOA score at follow-up in hybrid fusion and ACCF also showed comparable postoperative JOA scores between groups (SMD 0.03; 95% CI, −0.36, 0.43; P=0.88) (Figure 5B).
Three separate studies compared NDI at follow-up in ACDF and hybrid fusion with similar mean NDI score at follow-up ranged from 5.6 to 14.7 for ACDF and 6 to 14.3 for hybrid fusion (SMD −0.03; 95% CI, −0.22, 0.16; P=0.76) (Figure 6A). Three separate studies compared postoperative NDI in hybrid fusion and ACCF with similar mean NDI scores at follow-up ranged from 14.2 to 14.9 for hybrid fusion and 14 to 17.19 for ACCF (SMD −0.39; 95% CI, −0.90, 0.12; P=0.14) (Figure 6B).
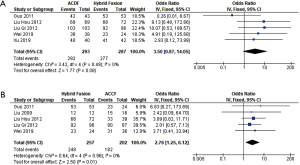
Fusion
Five separate studies compared the percentage of patients who were fused at follow-up in ACDF and hybrid fusion. The percentage of patients fused at follow-up ranged from 97.7% to 100% in the ACDF group and 94.4% to 100% in the hybrid fusion group (OR 3.50; 95% CI, 0.87, 14.05; P=0.08) (Figure 7A). Five separate studies compared the percentage of patients who were fused at follow-up in hybrid fusion and ACCF. The percentage of patients fused at follow-up in the hybrid fusion group was significantly higher than in the ACCF group (94.4–100% vs. 84.6–95.8%, respectively; OR 2.76; 95% CI, 1.25, 6.12; P=0.01) (Figure 7B).
Complications
Five studies compared the frequency of total complications in ACDF and hybrid fusion groups. The total complication rates were similar between the two groups (OR 0.70; 95% CI, 0.44, 1.13; P=0.14). Five studies comparing complication rates in hybrid fusion and ACCF groups showed significantly lower complication rates in the hybrid group compared to ACCF group (0–22.92% vs. 6.2–43.6%, respectively; OR 0.54; 95% CI, 0.34, 0.84; P=0.006). Four studies compared the frequency of implant failure or mesh subsidence in hybrid fusion and ACCF. The frequency of implant failure or mesh subsidence in the hybrid group ranged from 4.17% to 9.4% fusion which was significantly lower than in ACCF that ranged from 8.05% to 19.4% (OR 0.42; 95% CI, 0.20, 0.88; P=0.02).
Discussion
Degenerative cervical myelopathy, with an annual incidence of 41 per million in North America, is among the most common indications for cervical spine surgery (1,2). While cervical myelopathy has a variable natural history, patients often experience progressive symptoms that ultimately require surgical intervention (2,3,46). Although there is a near consensus that patients with progressive degenerative cervical myelopathy require treatment, there is a wide range of surgical option. Retrospective studies have examined anterior versus posterior approaches without clear superiority in radiographic and patient outcomes (2,47). Regarding anterior only approaches, surgeons have utilized a variety of surgical approaches to address spinal cord compression. ACDF has been employed to treat cervical spinal cord compression without postvertebral involvement. When there is stenosis behind the vertebral body, an ACDF may not be sufficient and an ACCF is required. The ACCF’s downsides include increased operative blood loss, increased hardware complications including device subsidence, and less ability to create and maintain cervical lordosis. ACDF also has shown to have increased rates of pseudoarthrosis with multi-level procedures (4,43,48,49). We have presented a case series of patients undergoing hybrid fusion and performed a meta-analysis to analyze the superiority of three-level ACDF, two-level corpectomy, and hybrid fusion in the treatment of three-level degenerative cervical myelopathy.
In terms of radiographic parameters, we analyzed cervical lordosis at follow-up and overall change in cervical lordosis. In our case series, we found an average postoperative C2–7 cervical lordosis of 11.8 degrees which was less than the range of average postoperative C2–7 cervical lordosis of the hybrid group included in the meta-analysis. When comparing hybrid fusion to ACCF there was a statistically significant increase in postoperative cervical lordosis in the hybrid group. Regarding the change in cervical lordosis from preoperative to follow-up; ACDF showed a statistically significant increase when compared to hybrid fusion which showed a statistically significant increase compared to ACCF. Zhao et al. 2018, a meta-analysis that analyzed pre and postoperative C2-7 cervical lordosis between ACDF and hybrid groups were additionally unable to find a statistically significant difference in postoperative lordosis between the two procedures (50). Shamji et al. 2013 also showed a statistically significant increase in change in cervical lordosis with ACDF as compared to HS (4). Comparing hybrid fusion to ACCF, Liu et al. 2015 showed a trend towards increased postoperative C2-7 cervical lordosis in the hybrid group however their results, unlike ours, were not statistically significant (51). A notable difference between their meta-analysis and ours, however, is that they included Odate et al. 2016, a study that focused on four-level degenerative cervical myelopathy and included three-level corpectomies in the ACCF group (31). We excluded that study as our meta-analysis was focused only on three-level procedures.
Regarding PRO we found an average postoperative JOA of 11 (range, 6–14) in our case series of hybrid fusion patients which was less than the mean postoperative JOA included in the meta-analysis. We were unable to find a statistically significant difference between the three surgical approaches with meta-analysis in terms of JOA at follow up, JOA recovery rate, and NDI at follow up. However, when Wei et al. 2019 was removed from the meta-analysis, there was a statistically significant increase in postoperative JOA in the ACDF group over the hybrid group and a near statistically significant increase in postoperative JOA in the ACCF group over the hybrid group. The reason that results from Wei et al. 2019 favored hybrid fusion in terms of postoperative JOA when compared to ACCF and ACDF is unclear but represents a fairly significant outlier in data collected thus far. Wei et al. 2019 only included patients with intramedullary increased signal intensity (ISI) on preoperative MRI and showed that patients undergoing hybrid fusion had a statistically significant improvement in ISI over patients undergoing ACDF or ACCF, this factor may explain why postoperative JOA (a clinical measure of cervical myelopathy) was so favored in the hybrid group (43). Our outcomes agree with Zhao et al., however regarding postoperative JOA, only agree with the conclusions of Shamji et al. when Wei et al. is excluded (4,50).
We analyzed multiple operative factors including estimated blood loss, operative time, fusion, and complications. Regarding operative blood loss, our case series of 10 patients undergoing hybrid fusion for three-level degenerative cervical myelopathy had an average estimated blood loss of 107.5 mL, significantly less than average estimated blood loss in the hybrid group used in meta-analysis. From our meta-analysis, we found that patients undergoing three-level ACDF had significantly less blood loss than patients undergoing hybrid fusion who in turn had significantly less blood loss than patients undergoing two-level ACCF. This relationship directly follows the number of corpectomies that occur in each procedure, which is where the majority of operative blood loss occurs and has been previously shown in other meta-analyses that involve hybrid fusion (50,51). Regarding operative time our meta-analysis failed to show a statistically significant difference between the three procedures. Regarding fusion, our case series had a postoperative fusion rate of 100%, however, one patient did require additional posterior fusion during the initial hospitalization, although this was reportedly for persistent stenosis. Regarding hybrid fusion and ACCF, our meta-analysis definitively showed that hybrid fusion had a statistically significant increased fusion rate. This is synonymous to the conclusion of meta-analysis Liu et al. 2015 (51). The overall conclusion that fusion rate is highest in ACDF followed by hybrid Fusion and lowest in ACCF may be supported by the decreased rigidity of a multilevel construct (48). The risk of instrumentation failure after a two-level corpectomy is well known and posterior instrumentation is often required especially in patients with significant loss of cervical lordosis. The total complication rate from our case series was 40% with postoperative dysphagia being most common. This is higher than the total complication rate from our meta-analysis which ranged from 0% to 22.9%. Regarding ACDF and hybrid fusion, our meta-analysis showed a trend towards decrease in frequency of total complications in the ACDF group however this was not statistically significant. Zhao et al. 2018 did show a statistically significant decrease in the frequency of complications with ACDF compared to hybrid fusion, however, used a publication in their meta-analysis which is not available to be read in English. Without that publication, they would have been unable to show significance (50). Regarding hybrid fusion and ACDF, our meta-analysis did show a statistically significant decrease in the frequency of complications with hybrid fusion. This agrees with previous data shown by meta-analysis Liu et al. (51). When further analyzing complications for implant failure and corpectomy device subsidence we found a statistically significant decrease in the hybrid group when compared to the ACCF group.
Two biomechanical studies have been done that explain some of the relationships shown in our meta-analysis. Singh et al. compared the rigidity of three anterior cervical constructs (ACDF, ACCF, HS) using three-dimensional motion analysis (6). The authors noted that multiple ACDF and HS provided a higher degree of rigidity in flexion/extension and lateral bending compared to two-level ACCF. Hussain et al. examined motion, disc stress, and facet loading at the adjacent level in three anterior cervical techniques using finite element modeling (52). They found that the ACCF model showed the greatest disc stress and facet loading followed by HS and ACDF. In addition, these biomechanical changes were seen more in the cephalad adjacent level. Anterior cervical plating after HS constructs has more points of fixation than ACCF allowing for more rigidity and decreased modes of failure. Together these biomechanical properties may explain why hybrid fusion is superior to ACCF in fusion percentage, frequency of complications, frequency of implant failure/mesh subsidence, and C2-7 cervical lordosis at follow-up.
There are several limitations to our study. No randomized-controlled trials were included in our meta-analysis and the included data was all retrospective. Articles were limited to English only which did leave out previous articles included in the meta-analysis of this topic. Relatively few studies, although more than in any other meta-analysis on this topic, were included and increasing the number of studies may increase the power to identify more statistically significant relationships on this topic. Follow-up was relatively short in the included studies.
Conclusions
To our knowledge this study presents the largest published meta-analysis of patients undergoing three-level ACDF, two-level corpectomy, and hybrid fusion in the treatment of three-level degenerative cervical myelopathy. We have shown that in comparison to three-level ACDF, hybrid fusion has a similar outcome, complication, and fusion success rate. Hybrid fusion has increased postoperative C2–7 cervical lordosis, a higher fusion rate, lower total complication rate, lower implant failure/mesh subsidence rate, and lower average blood loss than two-level cervical corpectomy. A hybrid cervical fusion for patients with post-vertebral degenerative cervical myelopathy and three-level degenerative cervical myelopathy is preferable to a two-level cervical corpectomy.
Acknowledgments
We would like to acknowledge the Rush University Department of Neurological Science Research team for their help in this paper.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nouri A, Tetreault L, Singh A, et al. Degenerative Cervical Myelopathy: Epidemiology, Genetics, and Pathogenesis. Spine (Phila Pa 1976) 2015;40:E675-93. [Crossref] [PubMed]
- Wilson JR, Tetreault LA, Kim J, et al. State of the Art in Degenerative Cervical Myelopathy: An Update on Current Clinical Evidence. Neurosurgery 2017;80:S33-45. [Crossref] [PubMed]
- Fehlings MG, Ibrahim A, Tetreault L, et al. A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: results from the prospective multicenter AOSpine international study on 479 patients. Spine (Phila Pa 1976) 2015;40:1322-8. [Crossref] [PubMed]
- Shamji MF, Massicotte EM, Traynelis VC, et al. Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976) 2013;38:S195-209. [Crossref] [PubMed]
- Guo Q, Bi X, Ni B, et al. Outcomes of three anterior decompression and fusion techniques in the treatment of three-level cervical spondylosis. Eur Spine J 2011;20:1539-44. [Crossref] [PubMed]
- Singh K, Vaccaro AR, Kim J, et al. Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine (Phila Pa 1976) 2004;29:845-9. [Crossref] [PubMed]
- Aghayev K, Doulgeris JJ, Gonzalez-Blohm SA, et al. Biomechanical comparison of a two-level anterior discectomy and a one-level corpectomy, combined with fusion and anterior plate reconstruction in the cervical spine. Clin Biomech (Bristol, Avon) 2014;29:21-5. [Crossref] [PubMed]
- Zhou J, Li X, Zhou X, et al. Anterior decompression and hybrid reconstruction with titanium mesh cage plus plate and self-locking stand-alone cage for the treatment of three-level cervical spondylotic myelopathy. J Clin Neurosci 2017;43:196-201. [Crossref] [PubMed]
- Kang L, Lin D, Ding Z, et al. Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics 2013;36:e88-94. [Crossref] [PubMed]
- Grasso G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 2015;24 Suppl 7:842-8. [Crossref] [PubMed]
- Shin DA, Yi S, Yoon DH, et al. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine (Phila Pa 1976) 2009;34:1153-9; discussion 1160-1. [Crossref] [PubMed]
- Hey HW, Hong CC, Long AS, et al. Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 2013;22:116-22. [Crossref] [PubMed]
- Ding F, Jia Z, Wu Y, et al. Fusion-nonfusion hybrid construct versus anterior cervical hybrid decompression and fusion: a comparative study for 3-level cervical degenerative disc diseases. Spine (Phila Pa 1976) 2014;39:1934-42. [Crossref] [PubMed]
- Mao N, Wu J, Zhang Y, et al. A Comparison of Anterior Cervical Corpectomy and Fusion Combined With Artificial Disc Replacement and Cage Fusion in Patients With Multilevel Cervical Spondylotic Myelopathy. Spine (Phila Pa 1976) 2015;40:1277-83. [Crossref] [PubMed]
- Chang HC, Tu TH, Chang HK, et al. Hybrid Corpectomy and Disc Arthroplasty for Cervical Spondylotic Myelopathy Caused by Ossification of Posterior Longitudinal Ligament and Disc Herniation. World Neurosurg 2016;95:22-30. [Crossref] [PubMed]
- Zhu Y, Fang J, Xu G, et al. A hybrid technique for treating multilevel cervical myelopathy: Cervical artificial disc replacement combined with fusion. Oncol Lett 2019;17:360-4. [PubMed]
- Hung CW, Wu MF, Yu GF, et al. Comparison of sagittal parameters for anterior cervical discectomy and fusion, hybrid surgery, and total disc replacement for three levels of cervical spondylosis. Clin Neurol Neurosurg 2018;168:140-6. [Crossref] [PubMed]
- Wang KF, Duan S, Zhu ZQ, et al. Clinical and Radiologic Features of 3 Reconstructive Procedures for the Surgical Management of Patients with Bilevel Cervical Degenerative Disc Disease at a Minimum Follow-Up Period of 5 Years: A Comparative Study. World Neurosurg 2018;113:e70-6. [Crossref] [PubMed]
- Jang SR, Lee SB, Cho KS. A Comparison of Anterior Cervical Discectomy and Fusion versus Fusion Combined with Artificial Disc Replacement for Treating 3-Level Cervical Spondylotic Disease. J Korean Neurosurg Soc 2017;60:676-83. [Crossref] [PubMed]
- Wu TK, Wang BY, Cheng D, et al. Clinical and radiographic features of hybrid surgery for the treatment of skip-level cervical degenerative disc disease: A minimum 24-month follow-up. J Clin Neurosci 2017;40:102-8. [Crossref] [PubMed]
- Wu TK, Wang BY, Deng MD, et al. A comparison of anterior cervical discectomy and fusion combined with cervical disc arthroplasty and cervical disc arthroplasty for the treatment of skip-level cervical degenerative disc disease: A retrospective study. Medicine (Baltimore) 2017;96:e8112. [Crossref] [PubMed]
- Tu TH, Wu JC, Cheng H, et al. Hybrid cervical disc arthroplasty. Neurosurg Focus 2017;42:V5. [Crossref] [PubMed]
- Chen J, Xu L, Jia YS, et al. Cervical anterior hybrid technique with bi-level Bryan artificial disc replacement and adjacent segment fusion for cervical myelopathy over three consecutive segments. J Clin Neurosci 2016;27:59-62. [Crossref] [PubMed]
- Shi JS, Lin B, Xue C, et al. Clinical and radiological outcomes following hybrid surgery in the treatment of multi-level cervical spondylosis: over a 2-year follow-up. J Orthop Surg Res 2015;10:185. [Crossref] [PubMed]
- Lee SB, Cho KS, Kim JY, et al. Hybrid surgery of multilevel cervical degenerative disc disease: review of literature and clinical results. J Korean Neurosurg Soc 2012;52:452-8. [Crossref] [PubMed]
- Barbagallo GM, Assietti R, Corbino L, et al. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J 2009;18 Suppl 1:29-39. [Crossref] [PubMed]
- Cardoso MJ, Mendelsohn A, Rosner MK. Cervical hybrid arthroplasty with 2 unique fusion techniques. J Neurosurg Spine 2011;15:48-54. [Crossref] [PubMed]
- Chin K, Pencle F, Coombs A, et al. Safety and Outcome of Outpatient 2-Level Hybrid Anterior Cervical Discectomy and Fusion plus Adjacent Total Disc Replacement. West Indian Med J 2017;66:440.
- Lian XF, Xu JG, Zeng BF, et al. Noncontiguous anterior decompression and fusion for multilevel cervical spondylotic myelopathy: a prospective randomized control clinical study. Eur Spine J 2010;19:713-9. [Crossref] [PubMed]
- Li Z, Wang H, Tang J, et al. Comparison of Three Reconstructive Techniques in the Surgical Management of Patients With Four-Level Cervical Spondylotic Myelopathy. Spine (Phila Pa 1976) 2017;42:E575-83. [Crossref] [PubMed]
- Odate S, Shikata J, Kimura H, et al. Hybrid Decompression and Fixation Technique Versus Plated 3-Vertebra Corpectomy for 4-Segment Cervical Myelopathy. Clin Spine Surg 2016;29:226-33. [Crossref] [PubMed]
- Kan L, Kang J, Gao R, et al. Clinical and radiological results of two hybrid reconstructive techniques in noncontiguous 3-level cervical spondylosis. J Neurosurg Spine 2014;21:944-50. [Crossref] [PubMed]
- Ashkenazi E, Smorgick Y, Rand N, et al. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine 2005;3:205-9. [Crossref] [PubMed]
- Liu Y, Yu KY, Hu JH. Hybrid decompression technique and two-level corpectomy are effective treatments for three-level cervical spondylotic myelopathy. J Zhejiang Univ Sci B 2009;10:696-701. [Crossref] [PubMed]
- Wei-bing X, Wun-Jer S, Gang L, et al. Reconstructive techniques study after anterior decompression of multilevel cervical spondylotic myelopathy. J Spinal Disord Tech 2009;22:511-5. [Crossref] [PubMed]
- Liu Y, Hou Y, Yang L, et al. Comparison of 3 reconstructive techniques in the surgical management of multilevel cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2012;37:E1450-8. [Crossref] [PubMed]
- Liu Y, Qi M, Chen H, et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J 2012;21:2428-35. [Crossref] [PubMed]
- Zárate-Kalfopulos B, Araos-Silva W, Reyes-Sanchez A, et al. Hybrid Decompression and Fixation Technique for the Treatment of Multisegmental Cervical Spondylotic Myelopathy. Int J Spine Surg 2016;10:30. [Crossref] [PubMed]
- Krätzig T, Mohme M, Mende KC, et al. Impact of the surgical strategy on the incidence of C5 nerve root palsy in decompressive cervical surgery. PLoS One 2017;12:e0188338. [Crossref] [PubMed]
- Liu X, Chen Y, Yang H, et al. The application of a new type of titanium mesh cage in hybrid anterior decompression and fusion technique for the treatment of continuously three-level cervical spondylotic myelopathy. Eur Spine J 2017;26:122-30. [Crossref] [PubMed]
- Sun K, Sun J, Wang S, et al. Placement of Titanium Mesh in Hybrid Decompression Surgery to Avoid Graft Subsidence in Treatment of Three-Level Cervical Spondylotic Myelopathy: Cephalad or Caudal? Med Sci Monit 2018;24:9479-87. [Crossref] [PubMed]
- Xu Z, Rao H, Zhang L, et al. Anterior Cervical Discectomy and Fusion Versus Hybrid Decompression and Fusion for the Treatment of 3-level Cervical Spondylotic Myelopathy: A Comparative Analysis of Cervical Sagittal Balance and Outcomes. World Neurosurg 2019;132:e752-8. [Crossref] [PubMed]
- Wei L, Cao P, Xu C, et al. Comparison of Three Anterior Techniques in the Surgical Treatment of Three-Level Cervical Spondylotic Myelopathy with Intramedullary T2-Weighted Increased Signal Intensity. World Neurosurg 2019;126:e842-52. [Crossref] [PubMed]
- Huang Y, Lan Z, Xu W. Analysis of sagittal alignment parameters following anterior cervical hybrid decompression and fusion of multilevel cervical Spondylotic myelopathy. BMC Musculoskelet Disord 2019;20:1. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am 2013;95:1651-8. [Crossref] [PubMed]
- Fehlings MG, Barry S, Kopjar B, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976) 2013;38:2247-52. [Crossref] [PubMed]
- Emery SE. Anterior approaches for cervical spondylotic myelopathy: which? When? How? Eur Spine J 2015;24 Suppl 2:150-9. [Crossref] [PubMed]
- Song KJ, Lee KB, Song JH. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J 2012;21:1551-7. [Crossref] [PubMed]
- Zhao CM, Chen Q, Zhang Y, et al. Anterior cervical discectomy and fusion versus hybrid surgery in multilevel cervical spondylotic myelopathy: A meta-analysis. Medicine (Baltimore) 2018;97:e11973. [Crossref] [PubMed]
- Liu JM, Peng HW, Liu ZL, et al. Hybrid Decompression Technique Versus Anterior Cervical Corpectomy and Fusion for Treating Multilevel Cervical Spondylotic Myelopathy: Which One Is Better? World Neurosurg 2015;84:2022-9. [Crossref] [PubMed]
- Hussain M, Nassr A, Natarajan RN, et al. Relationship between biomechanical changes at adjacent segments and number of fused bone grafts in multilevel cervical fusions: a finite element investigation. J Neurosurg Spine 2014;20:22-9. [Crossref] [PubMed]


