
Anterior osteotomy for rigid cervical deformity correction
Introduction
Deformity of the cervical spine can be associated with significant pain, disability, and impaired quality of life. Patients often present with neck pain, myelopathy, or sensorimotor symptoms. In cases of severe deformity with cervical kyphosis, patients can also have difficulty maintaining normal horizontal gaze. Cervical deformity has gained significant attention over the past decade with novel classification schemes (1,2) and a growing body of literature describing outcomes after cervical deformity surgery (3-6).
Historical treatments have utilized posterior-based approaches including the opening wedge osteotomy (7,8) and pedicle subtraction osteotomy (PSO) (9,10), however the later technique is limited to the lower cervical or upper thoracic levels due to the presence of the vertebral artery. Furthermore, preservation of cervical nerve roots and their sensitivity to compression makes the PSO even more challenging. Ames et al. proposed a cervical osteotomy classification scheme that ranges from least invasive to most invasive and includes: (I) partial facet joint resection, (II) complete facet joint/Ponte osteotomy, (III) partial or complete corpectomy, (IV) complete uncovertebral join resection to transverse foramen, (V) opening wedge osteotomy, (VI) closing wedge osteotomy, and (VII) complete vertebral column resection (11). Tan et al. presented an algorithmic approach for treating cervical deformity that highlights the critical importance of preoperative planning and an algorithm for the use of anterior and posterior surgical techniques for cervical deformity correction (12,13). Anterior techniques provide the advantage of utilizing a classic, well-recognized approach and the ability to reconstruct multiple levels of the anterior column and generate a powerful and relatively safe deformity correction.
The anterior Riew osteotomy, defined as an osteotomy through the cervical disc space and uncovertebral joints back to the level of the transverse foramen bilaterally, is a powerful correction technique that can be applied throughout the cervical spine (14). In patients with “ear-on-shoulder” deformities, asymmetric anterior osteotomies can be utilized to provide correction in the coronal plane. This review will summarize the use of the anterior osteotomy for correction of rigid cervical deformity.
Preoperative evaluation
The initial evaluation must include a thorough history and physical exam with comprehensive review of imaging studies including AP/lateral, oblique, and dynamic (flexion/extension) cervical X-rays, scoliosis films, computed tomography (CT) scans, and magnetic resonance imaging (MRI). The presence of any neurologic deficits should be documented with careful attention to imaging studies to identify sites of symptomatic compression, which should be integrated into the final treatment plan. The presence of symptoms or exam findings that are not congruent with the imaging studies should prompt additional work-up for non-spine related etiologies such as peripheral neuropathy, nerve entrapment syndromes, or neuromuscular disorders. Patients with a history of previous anterior cervical spine surgery should undergo formal vocal cord function studies by an otolaryngologist.
Distinct imaging modalities provide unique information to guide surgical planning. Cervical X-rays can assess the severity of deformity, flexibility, apex location, and sites of foraminal stenosis. Scoliosis films provide information on global balance and may reveal underlying thoracolumbar deformities that may be contributing to a given patient’s cervical deformity. Important radiographic parameters include cervical lordosis, C2–C7 sagittal vertical axis, T1 slope, and chin-brow vertical angle (15). CT scans provide allow for careful evaluation of the vertebral body, disc spaces, and facet joints to assess for any preexisting fusion. In cases where posterior fusion is present, the surgical plan may require additional posterior facet releases to achieve the desired deformity correction. MRI allows for identification of neural element compression at the cord or nerve root level. Patients who cannot undergo MRI may benefit from CT myelogram.
The decision of approach side for anterior cervical surgery requires review of several factors. In patients with vocal cord dysfunction related to prior surgery, an ipsilateral approach should be used to avoid bilateral vocal cord injury. In patients with normal vocal cord function, we prefer a left-sided approach due to the longer course of the recurrent laryngeal nerve. In patients with significant coronal deformity, an approach from the convex side is generally easier. Additionally, the anatomy and course of the vertebral arteries should be carefully reviewed on preoperative imaging.
Surgical technique
Prior to surgery, the surgeon and anesthesia team should evaluate the patient’s airway, degree of spinal cord compression, and potential spinal instability to determine the safest approach for endotracheal intubation, which in complex cases may require awake fiber intubation. In general, cervical deformity cases should be performed with intraoperative neuromonitoring. In cases with spinal cord compression or instability, baseline should be obtained prior to manipulating the head and neck for final positioning. In patients with spinal cord compression, the mean arterial pressure (MAP) should be maintained above 80 mmHg during intubation and throughout the operation.
The surgeon must anticipate the course of the entire operation during positioning, which includes pushing the head backwards after completion of the anterior osteotomy. For rigid deformities that require an anterior osteotomy, folded sheets are placed under the upper thoracic region such that the head is suspended in air. More folded sheets can then be used to support the head. We then place Gardner-Wells tongs with approximately 15 lbs of traction. This helps to maintain proper rotational and coronal alignment. After completing the anterior osteotomy, the surgeon will ask the anesthesiologist to remove the sheets one at a time from under the head while the surgeon pushes on the forehead of the patient thru the sterile drapes. This will result in osteoclasis of the posterior fusion mass in a controlled manner. After the deformity has been corrected, the head will be resting on the operating table so the greater the magnitude of the desired correction, the higher the head must be off of the table.
After final position is complete the neck is prepped and draped in the usual sterile fashion. We recommend use of the operating microscope throughout the case. The anterior spine is exposed using the standard Smith-Robinson approach and all levels are confirmed with intraoperative fluoroscopy. Exposure of the apex of kyphosis can be challenging since it will be located much deeper in the wound than a traditional approach for degenerative disease. A combination of blunt and sharp dissection is used to expose the area of interest. Once location is confirmed on fluoroscopy, the longus colli muscles are detached and stripped from their attachment at the mid-vertebral body using bipolar cautery, with special care to leave a muscular cuff. We often transect the longus colli muscles in kyphotic patients, as they contribute to neck flexion. Care is taken to avoid injuring the sympathetic chain at the lateral edge of the longus colli.
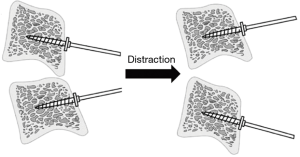
We recommend use of table-mounted retractors inserted under the longus colli cuff to maintain exposure. The Leksell ronguer is used to remove any anterior osteophytes, which facilitates exposure of the disc space. Caspar pins are placed into the vertebral body at the level of the intended osteotomy and in cases of osteoporotic bone, two sets of pins can be used to increase the strength of bony purchase. Special care must be taken to ensure the pins are placed perpendicular to the anterior plane of the spine at each vertebral body (Figure 1); this may result in divergent pins, however it will allow for lordosis when the pins are distracted after completion of the osteotomy.
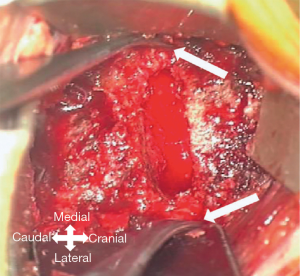
The anterior osteotomy can be performed using a high-speed 2.5 mm matchstick burr. The bony resection should be perpendicular to the spine in the same plane as the disc space to ensure symmetric resection in the coronal plane. In patients with mixed coronal and kyphotic deformities, the bony resection can be asymmetric to restore alignment in the coronal and sagittal planes. The osteotomy is carried back to the posterior longitudinal ligament (PLL) across the disc space up to the uncovertebral joints laterally. Attention is then turned to the lateral osteotomy, which is performed in a careful, step-wise fashion to avoid iatrogenic vertebral artery injury. A combination of upgoing curette and Penfield No. 4 dissector are used to dissect and expose the lateral uncinate process (Figure 2). A Penfield No. 2 dissector is then inserted lateral to the uncinate process to visualize the lateral margin of the bony resection and to protect the vertebral artery during drilling of the uncinate. A thin rim or shell of bone is left along the lateral border of the uncinate to protect the vertebral body and can be carefully removed using a curette. Once the nerve root is identified, the foraminotomy can be completed using curettes, which will allow for definitive decompression of the exiting nerve root and completion of the osteotomy.
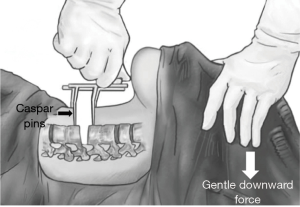
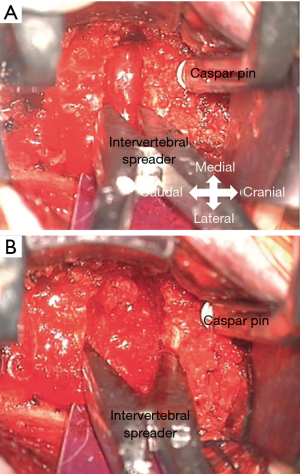
After the osteotomy has been carried back to the neural foramen bilaterally, attention is turned to deformity correction. The sheets or padding under the patient’s head are slowly and sequentially removed while the surgeon applies gentle downward pressure on the forehead (Figure 3). This provides the greatest biomechanical leverage with the lowest risk of Caspar pin loosening or vertebral body fracture during correction. In addition to Caspar pins, we use sequentially larger disc space sizers from a stand-alone cervical cage set, starting with a 5-mm height. After placing each sizer in the disc space, it is gently rocked cranially and caudally while also pushing down on the forehead (Figure 4). The Caspar distractor is widened to maintain the correction. Once the back of the head reaches the operating table, the anterior portion of the kyphosis correction is generally complete. In cases where additional lordosis is needed, the anesthesia team can carefully place a folded sheet under the patient’s shoulder to elevate the head so it can be pushed further posteriorly. At this point, additional weight can be added to the Gardner-Wells tongs (up to 25 lbs.) to maintain the desired correction. In patients with previous posterior fusion or instrumentation, partial correction of the deformity can generally be achieved since the posterior fusion mass will flex a few degrees, although 3.5 mm cobalt chromium rods pose the greatest challenge given their rigidity and strength.
Bone graft is then inserted into the distracted osteotomy site. It is important to recognize that since the bone across the osteotomy site is typically cancellous, there is a high likelihood of graft subsidence and therefore the largest bone graft should be utilized to maximize surface area and structural support. If an adequate deformity correction is achieved, an anterior cervical plate with fixed angle screws is placed. However, if additional posterior releases are required to achieve the desired correction, we recommend use of a trapezoid shaped bone graft that only contacts the anterior osteotomy site so that additional lordosis can be achieved. In these cases, we often use a standalone cage fixed with a single screw, however an interference screw or buttress plate can also be used to prevent graft extrusion during the posterior stage.
Meticulous hemostasis is obtained and the wound closed in standard fashion. We recommend a Penrose drain instead of closed-suction drain since they will never occlude and can theoretically allow for hematoma to be manually expressed through and around the drain site. The wound is then covered with a heavy abdominal pad with watertight dressing. We recommend immediate posterior fixation, however in the event of a delay, a halo or rigid cervical collar is used until the definitive posterior procedure.
Postoperative management
For cases with less than 3 hours of anterior retraction time, the patient is typically extubated after surgery. However, in cases with more than 3 hours of retraction, consideration is given to keeping the patients intubated overnight with a cuff-leak test the next morning prior to extubation. The fewer the number of levels operated on, the more time the retractor has been compressing the soft tissues. So a 4-level osteotomy that takes 3 hours of retraction time is much less likely to result in airway edema than a 1-level taking the same amount of time. Hourly neurologic exams are performed overnight and in the absence of a neurologic deficit, the blood pressure can be transitioned to normotension. The Penrose drain is maintained until the dressing is dry for 8 consecutive hours, which generally occurs on postoperative day 1 or 2. Patients are placed in a cervical orthosis and participate in physical therapy starting postoperative day 1. A soft collar can be used for most cases, however if there is concern over the strength of posterior fixation or unusually soft bone, a rigid collar is used.
Complications
Common complications related to the anterior cervical approach include dysphagia, vocal cord paralysis, and tracheal/esophageal injury. Dysphagia is generally transient and can be treated with a short course of steroids in severe cases. Less common complications include injury to the vertebral artery, spinal cord or nerve root, cerebrospinal fluid leak, and delayed issues including wound infection, instrumentation failure, graft subsidence, and pseudarthrosis. Wound infections are typically rare for anterior procedures but the risk is higher when used in combination with a posterior approach. Care must be taken to eliminate dead space by closing in multiple layers and adding vancomycin powder into the wound. Pseudarthrosis rates are typically low when the anterior osteotomy is supplemented with posterior fixation. Rates of major medical complications range from 3.1–44.4%, neurologic complications approximately 13.5%, and mortality 3.1–6.7% (16). Appropriate patient selection, thoughtful surgical planning, meticulous surgical technique, and tailored postoperative care can all minimize complications in this particularly high-risk patient demographic. Patient satisfaction rates are often very high given the degree of preoperative pain and disability associated with cervical deformity (17).
Case illustration
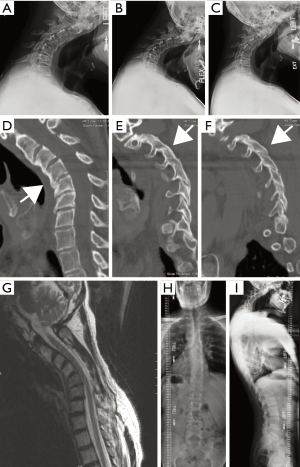
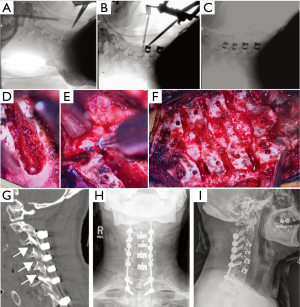
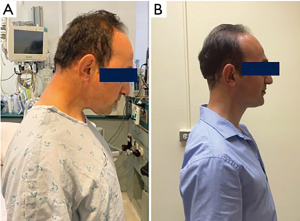
A 42-year-old male presented with 3 years of progressive neck and shoulder pain along with neck stiffness, decreased range of motion, and difficulty looking straight. Pain originated in the neck and radiated into bilateral shoulders (right worse than left) and upper arms. Physical exam was notable for normal strength and sensation, normal deep tendon reflexes, and inability to keep the head upright or maintain horizontal gaze with decreased range of motion. X-rays demonstrated a rigid cervical kyphotic deformity without significant coronal or sagittal imbalance. CT scan showed autofusion of several facets with bridging anterior osteophytes. MRI showed no evidence of significant spinal cord compression or cord signal change. Preoperative imaging is summarized in Figure 5. The patient underwent C3–7 ACDF C3–4 and C4–5 anterior osteotomies followed by C2–T2 posterior instrumented fusion with C3–4, C4–5, and C5–6 posterior column osteotomies. Intraoperative and postoperative imaging is summarized in Figure 6. The patient tolerated surgery without complication. He was started on a regular diet postoperative day 1 and discharged home on postoperative day 3 in good condition. The patient was doing well with improved neck posture at the 6-week follow-up visit (Figure 7).
Conclusions
The anterior Riew osteotomy is a powerful technique for the correction of rigid cervical deformity. Patients with “chin-on-chest” or “ear-on-shoulder” can be safely and effectively treated with this approach. Patient selection, preoperative planning, and surgical technique all contribute to the success of the operation.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. LAT serves as the unpaid editorial board member of Journal of Spine Surgery from Jan. 2019 to Jan. 2021 and served as the unpaid Guest Editor of the series. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83. [Crossref] [PubMed]
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity-Part 1: Biomechanics, Radiographic Parameters, and Classification. Neurosurgery 2017;81:197-203. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Kim HJ, et al. Comparison of Best Versus Worst Clinical Outcomes for Adult Cervical Deformity Surgery. Global Spine J 2019;9:303-14. [Crossref] [PubMed]
- Passias PG, Horn SR, Bortz CA, et al. The Relationship Between Improvements in Myelopathy and Sagittal Realignment in Cervical Deformity Surgery Outcomes. Spine (Phila Pa 1976) 2018;43:1117-24. [Crossref] [PubMed]
- Poorman GW, Passias PG, Horn SR, et al. Despite worse baseline status depressed patients achieved outcomes similar to those in nondepressed patients after surgery for cervical deformity. Neurosurg Focus 2017;43:E10. [Crossref] [PubMed]
- Ailon T, Smith JS, Shaffrey CI, et al. Outcomes of Operative Treatment for Adult Cervical Deformity: A Prospective Multicenter Assessment With 1-Year Follow-up. Neurosurgery 2018;83:1031-9. [Crossref] [PubMed]
- Mason C, Cozen L, Adelstein L. Surgical correction of flexion deformity of the cervical spine. Calif Med 1953;79:244-6. [PubMed]
- Urist MR. Osteotomy of the cervical spine; report of a case of ankylosing rheumatoid spondylitis. J Bone Joint Surg Am 1958;40-A:833-43. [Crossref] [PubMed]
- Deviren V, Scheer JK, Ames CP. Technique of cervicothoracic junction pedicle subtraction osteotomy for cervical sagittal imbalance: report of 11 cases. J Neurosurg Spine 2011;15:174-81. [Crossref] [PubMed]
- Wollowick AL, Kelly MP, Riew KD. Pedicle subtraction osteotomy in the cervical spine. Spine (Phila Pa 1976) 2012;37:E342-8. [Crossref] [PubMed]
- Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 2013;19:269-78. [Crossref] [PubMed]
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity-Part 2: Management Algorithm and Anterior Techniques. Neurosurgery 2017;81:561-7. [Crossref] [PubMed]
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity-Part 3: Posterior Techniques, Clinical Outcome, and Complications. Neurosurgery 2017;81:893-8. [Crossref] [PubMed]
- Kim HJ, Piyaskulkaew C, Riew KD. Anterior cervical osteotomy for fixed cervical deformities. Spine (Phila Pa 1976) 2014;39:1751-7. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 2013;19:141-59. [Crossref] [PubMed]
- Etame AB, Wang AC, Than KD, et al. Outcomes after surgery for cervical spine deformity: review of the literature. Neurosurg Focus 2010;28:E14. [Crossref] [PubMed]
- Smith JS, Ramchandran S, Lafage V, et al. Prospective Multicenter Assessment of Early Complication Rates Associated With Adult Cervical Deformity Surgery in 78 Patients. Neurosurgery 2016;79:378-88. [Crossref] [PubMed]


