Is Asia truly a hotspot of contemporary minimally invasive and endoscopic spinal surgery?
Introduction
Asia is typically perceived as the hotspot of modern minimally invasive (MIS) and endoscopic spinal (ES) surgery. Many of the key opinion leaders (KOL) reside in Korea, and China and several of the recent advances in contemporary endoscopic spinal surgery have originated from there. These two countries also produced the highest quantity of peer-reviewed journal publication both in MIS and ES surgery within the last five years. While MIS and ES surgery have become a commonplace the world over (1-21), implementation outside Asia seems to lack sufficient traction in spite of pioneers of the method having published their results for the last three decades and proven both the safety and efficacy of the procedures (22-25).
There has been a recent paradigm shift in the accepted surgical indication for spinal endoscopy from herniated disc (26-29) to spinal stenosis (30), and even interventional intradiscal (31) and axial pain management procedures (32,33). As with any surgical technology gaining popularity and becoming more mainstream as an accepted method to treat common degenerative conditions of the lumbar spine, formal training of endoscopic surgery procedures has been initiated by KOL in North America by organizing small workshops under the umbrella of small specialty societies such as the International Intradiscal Therapy Society (IITS), and The International Society for the Advancement of Spine Surgery (ISASS) (34). In Asia, National and International organizations such as the Korean Minimally Invasive Spine Society (KOMISS) and the Pacific and Asian Minimally Invasive Spine Society (PASMISS) have also begun to integrate cadaver workshops and symposia on spinal endoscopy as well into the core curriculum (35-37). In 2018, the program of the 6th World Congress of Minimally Invasive Spine Surgery & Techniques (WMISST) hosted during June 7th–10th in Chongqing, China and held in cooperation with Chinese Medical Doctor Association (CMDA), Chinese Association of Orthopaedic Surgeons (CAOS), North American Spine Society (NASS), EUROSPINE, Minimally Invasive Spine Committee of CAOS, Minimally Invasive Spine Surgery Branch of Spine and Spinal Cord Professional Committee, Chinese Association of Rehabilitation Medicine, Minimally Invasive Spine Surgery Society of SICOT China, Minimally Invasive Surgery Society of Army Orthopedic Association, Spine Endoscopic Committee of Chinese Medical Association, demonstrated a high level of contemporary MIS and ES education. Topics solicited for presentation at WMISST were prioritized in order from (I) microscopic endoscopic surgery, (II) minimally invasive fusion surgery, (III) digital minimally invasive spinal surgery techniques (virtual, navigation, and artificial intelligence), to (IV) other minimally invasive spine innovation technology. In contrast, NASS historically has done little, but for the first time during its 2018 meeting in Los Angeles, USA, included three separate cadaver workshops dedicated to endoscopic spinal decompression procedures.
In North America and Europe, formal accredited MIS and ES surgery fellowship programs are lacking, and only a few mentorship programs exist that are the centers of clinical expertise. The authors of this publication were interested in better understanding what distinguishes MIS and ES surgeons in Asian countries/regions with respect to training background, practice patterns and motivators from surgeons residing in other countries/regions and whether or not they performed MIS and ES surgery at a higher degree of sophistication and innovation.
Methods
The authors solicited responses to an online survey via email, and chat groups in social networks including Facebook, WeChat, WhatsApp, and LinkedIn. The survey was available online and distributed via a link distributed through these social network media. Upon clicking on the link, the prospective surgeon respondent was taken to the typeform website at www.typeform.com where the survey opened automatically. The survey could be answered on the computer, laptop, and any hand-held devices such as an iPad, or a cellular smartphone. The typeform services were chosen because of its ease of use across multiple user-interface platforms. Survey accessibility on the personal smartphone by the surgeon was considered a significant advantage to facilitate recruitment of respondents, ease of use, and respondent’s retention to improve survey completion.
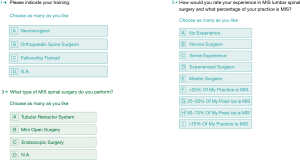
The survey consisted of four questions. The questions were aimed at soliciting information deemed to be important factors of endoscopic MIS implementation, whereas another question requested demographic information of the respondent including the extent of postgraduate residency and fellowship training, and the percentage of his/her practice being devoted to MIS. Instead of user queries with a Likert scale, the survey was constructed of simple multiple-choice questions some of which with multiple possible answers for ease of use and to maximize respondent retention once on the web site and to facilitate survey completion. Some of the survey questions as they appeared on the prospective surgeon respondent’s screen are shown in Figure 1.
Surgeons were asked the following four questions:
1. Please indicate your training?
- Neurosurgery
- Orthopaedic surgery
- Fellowship trained
- N.A.
2. Did you complete a fellowship is spine surgery (YES/NO)?
3. Do you think minimally invasive spinal surgery is considered mainstream in your area and practice setting?
4. What is or was your primary motivation to implement MIS into your clinical practice?
- Personal interest.
- Patient demand.
- I use it for marketing & business development of my medical practice.
- I perceive pressure from my peers and colleagues.
- I am pressured by my organization to implement MIS.
- I am afraid of being left behind and my practice could be perceived as outdated.
5. Which avenue did you use to train for the MIS you currently employ in your clinical practice today?
- I attended workshops and local meetings.
- I attended national and international meetings.
- I learned from likeminded peers in small groups and subspecialty societies.
6. What type of MIS spinal surgery do you perform?
- Tubular retractor system
- Mini-open surgery
- Endoscopic surgery
- N.A.
7. Which obstacles to MISST implementation apply to you?
- There are no obstacles.
- Lack of industry support.
- High upfront equipment cost is hindering me implementing MISST.
- High cost of disposables is problematic.
- Reimbursement is too low to economically justify MISST.
- Health insurance denial.
- MISST is considered experimental, outside the treatment- or coverage guidelines.
8. How would you rate your experience in MIS lumbar spinal surgery and what percentage of your practice is MIS?
- No experience
- Novice surgeon
- Some experience
- Experienced surgeon
- Master surgeon
- <25%
- 25–50%
- 50–75%
- >75%
- I don’t exactly know
9. Tell us a little about yourself:
- What is your gender?
- What is your age?
- What’s your country of residence?
- How many peers/colleagues does your organization have?
The survey ran from October 26 to November 14, 2018. The authors were blinded as to the identity of the responding surgeon at all times. Individual personal identifiers were not recorded. The typeform.com survey created a time-stamp upon initiation of the study and once the completed questionnaire was submitted. Also, a unique network identifier (ID without IP address) was recorded for each responding surgeon. Upon completion of the survey, the responses were downloaded in an Excel file format and imported into IBM SPSS (version 25) statistical software package for further data analysis.
Descriptive statistic measures were used to count responses and calculate the mean, range, and standard deviation as well as percentages. Additional crosstabulation methods were used to assess for any statistically significant association between the different surgeon responses using Pearson Chi-Square and Fisher’s Exact Test. Expected cell counts, continuity corrections, and likelihood ratios were calculated for some analyses. Kappa statistics were performed to test for statistical significance of agreement between the individual responses. As another method to assess for agreement or disagreement between the entered responses, linear regression analysis was performed to determine whether the variances in surgeons’ opinions were normally distributed (agreement) or showed asymmetric distribution (disagreement). The authors also used linear regression analysis in an attempt to measure the presumed consistency of the submitted responses in lieu of unknown sample size required to have sufficient power for clinically meaningful statistical analysis. A P value of 0.05 or less was considered statistically significant. A confidence interval of 95% was considered for all statistical tests.
Results
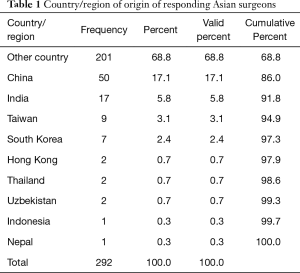
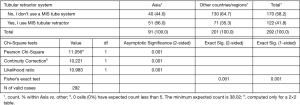
The online survey was accessed by 430 surgeons of which 293 submitted a survey recording 292 submissions as valid responses. The survey site had 500 total visits. The completion rate was 67.4% and the average time to complete the survey was 8 min and 54 s. Twenty-eight surgeons completed the survey on a PC or laptop with 37 total and 34 unique visits with a completion rate of 87.5% and average time to finish 2 min and 30 s. The majority of surgeons [261] responded to the survey using their smartphones during 459 total and 395 unique visits with a completion rate of 66.1% taking an average time of 9 min and 38 s to complete. Only one surgeon used a tablet to complete the survey. As shown in Table 1, 91 of the 292 responding surgeons where from Asian countries/regions with China being in the lead (50/292; 17.1%) followed by India (17/292; 5.8%), Taiwan (9/292; 3.1%), and South Korea (7/292; 2.4%).
Full table
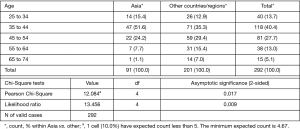
The majority of surgeons (161/292; 55.1%) participating in this survey were orthopaedic surgeons, followed by neurosurgeons (97/292; 33.2%), and a small group of surgeons (34/292; 11.6%) who indicated that they completed another form of a postgraduate residency program. There was no statistically significant difference between the percentage of neuro- versus orthopaedic surgeons in Asian versus other countries/regions (P=0.95). The vast majority (251/292; 86.0%) of the 292 responding surgeons were not fellowship trained in MIS. In contrast, only 14.0% (41/292) of surgeons had completed an MIS fellowship at the time they returned to the survey. There was no statistically significant difference between the percentage of surgeons with or without a fellowship training in Asian versus other countries/regions (P=0.786). The portion of fellowship trained spinal surgeons was slightly lower in Asian countries/regions (9.9%) than in the entire group of surgeons surveyed. A statistically significantly (P=0.017) higher number of surgeons from Asia were between the ages of 35 to 44 (Figure 2; 51.6%) compared to responding surgeons from other countries/regions (35.3%). Nearly a third (29.4%) of surgeons from non-Asian countries/regions were between the ages of 45–54 years of age.
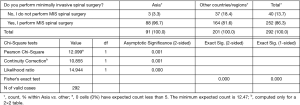
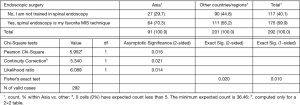
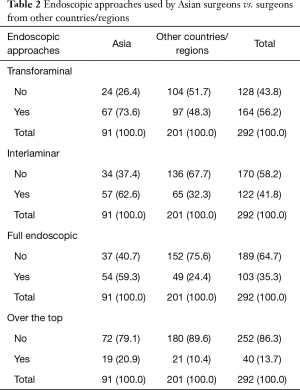
A statistically significantly higher percentage of Asian surgeons (96.7%) compared to non-Asian surgeons (81.6%) indicated that they perform MIS and ES surgery (Figure 3; P=0.001). An example includes the use of a tubular retractor system which was used by 56.0% Asian compared to only 35.3% of non-Asian surgeons (Figure 4; P=0.001). In comparison, spinal endoscopy was employed by 70.3% of Asian versus 55.2% of non-Asian surgeons (Figure 5; P=0.015). Statistically significantly higher percentage of usage of various endoscopic decompression techniques requiring advanced training was reported nearly twice as high by the Asian surgeons than by non-Asian surgeons (Table 2): interlaminar approach 62.6% vs. 32.3%, full endoscopic approach 59.3% vs. 24.4%, and over the top approach 20.9% vs. 10.4%, respectively.
Full table
Surgeons from Asia responded in a similar manner as surgeons from other countries/regions at no statistically significant difference to questions regarding their continued MIS and ES training (P=0.199). Informal sources of education in MIS and ES surgery techniques, such as National meetings (27% vs. 63%), exchange in small groups of like-minded peers (32.6% vs. 69.5%), and International meetings (30.5% vs. 69.5%) were reported by far less frequently by Asian surgeons than surgeons from other countries/regions. The self-reported skill level by Asian surgeons also differed substantially from that of surgeons from other regions. For example, only 25.9% of Asian surgeons rated themselves as unexperienced novice surgeons (versus 74.1% from other countries/regions). The percentage of self-reported master-surgeons was 17.6% amongst Asian surgeons vs. 11.9% amongst non-Asian surgeons. Nearly twice as many Asian (27.5%) versus non-Asian (12.9%) surgeons were reporting that over 75% of their spine practice is devoted to MIS and ES surgery (P=0.002).
Many of the motivators to the implementation of MIS and ES surgery for non-Asian surgeons were less relevant for surgeons from Asia. For example, personal interest was listed only by 30.6% of Asian vs. 69.4% of non-Asian surgeons. Patient demand for MIS and ES surgery was also less commonly reported as a motivator by Asian (31.3%) versus non-Asian (68.8%). Other motivators, such as marketing and business development (33.1% vs. 66.7%), pressure from peers (13.3% vs. 86.7%), pressure from their organization (35.7% vs. 64.3%), and fear of being left behind (27.3% vs. 72.7%) were also reported at lower rates by Asian surgeons than by surgeons from other countries/regions.
Obstacles to MIS and ES surgery implementation were also reported at lower rates by surgeons from Asia than from other countries/regions outside that region. While 71.1% of surgeons from non-Asian countries/regions reported obstacles to the MIS and ES implementation, only 28.9% of Asian surgeons reported to run into implementation problems. Examples include high equipment (26% vs. 74%) and disposable cost (35.5% vs. 64.5%), low reimbursement (28.6% vs. 71.4%), health insurance denial (29.3%% vs. 70.7%), and organizational hurdles (40% vs. 60%), respectively.
Discussion
The authors solicited responses to an online survey from spine surgeons residing in Asia and other countries/regions. The survey was distributed via email and social media. Average response rates have been reported for an in-person survey at 57%, mail survey at 50%, email survey at 30%, online survey at 29%, telephone survey at 18%, an in-app survey of 13%, with an overall average survey response rate of 33% (38-45). Clinical examples include a postal survey sent to 2,048 prospective respondents with a response rate of 46% (46). Another web-based 59-item survey with 260 respondents had a response rate of 60% (47), and a written paper survey reported a response rate of 49.5% (302/610) (48). An online patient satisfaction survey in 9,975 Medicare beneficiaries with 434 unduplicated survey submissions had a response rate of 4.3% (49). Clinical opinion survey research amongst spine surgeons showed response rates ranging from 49% (n=51) obtained in a study on surgical management of spinal stenosis amongst Norwegian spine surgeons (50), to 61.3% (n=357) amongst members of the Scoliosis Research Society surveyed on use of MIS Techniques in the Treatment of Adult Spinal Deformity (51). In comparison, another sizeable online survey study sent to trauma, spine and craniomaxillofacial surgeon members of the AO Foundation, yielded 1,212 valid and completed submission at an overall response rate of 4.1% (52). These examples illustrate that there can be a wide range of survey response rates and that 67.4% obtained in this study is higher than the average reported for clinical online survey research.
This survey on training and skill level of MIS and ES amongst spine surgeons was blinded, and the team of authors had no information as to the identity of the responding spine surgeons, hence, minimizing the impact of intuition and hindsight bias amongst the investigators. With a response rate of 67.4%, the authors also considered the impact of non-response bias less problematic since it was still higher than the average reported response rates in several surveys amongst spine surgeons which were published in well-respected journals. Non-response bias has been recognized as an indicator of survey quality. Although lower response rates in the 20% range have been related to more accurate measurements than surveys with 60% to 70% response rates which are still considered preferable since the missing data has not been found to be random (53). Nonetheless, there could have been geographic bias where the digital communication used in this survey study could have obliterated existing geographic diversity and various cultural perspectives of responding spine surgeons. Therefore, the authors were cautious not to generalize the findings of this survey in the context of their preconceived notions of MISST and to counter the homogenizing effect of the digital data acquisition across multiple cultural boundaries while recognizing its limitations in the quest for genuinely alternative insights by other surgeons. To minimize the potentially distorting effects of such geographic biases, this team of authors from multiple countries/regions in Asia, the Americas, and Europe worked closely together on the survey data analysis and interpretation taking the cultural diversities among respondents in the practice of MISST into account.
The surveys were forwarded to known peers. However, the study investigators did not know the distribution of responses and which underlying trends would emerge when the survey launched. Hence, it was unclear at the outset of the online data acquisition when sufficient statistical sample size would have been achieved to close the study. Linear regression monitoring of the change in response rates to the questions over the three weeks and kappa analysis of agreement in the 292 survey submissions showed a relatively stable distribution of asymmetric variances suggesting that similar percentage response rates could have been reasonably expected with a broader polling sample. This added to the authors’ confidence that results presented herein are in fact representative of current opinions regarding endoscopic MIS and ES training and skill level amongst responding Asian and non-Asian spine surgeons. This team of authors considered the reported differences in skill level, and formal training in MIS and ES spinal surgery not only statistically significant whenever a p-value of less than or equal to 0.05 was found, but also clinically meaningful.
This survey suggests that MIS and ES surgery is more wide-spread and employed by spine surgeons residing in Asian countries/regions than in other regions of the world. This is corroborated by the high number of peer-reviewed articles published by authors from China and Korea within the last years (54). This survey also indicated that hurdles for implementation of MIS and ES surgery are much lower ranging from less concern about equipment and disposable cost to less regard for institutional obstacles, low reimbursement, or lack of prior authorization of health insurance companies. Taking the difference in surgeon motivators into account—with Asian surgeons being much less concerned with patient demand for MIS or ES surgery or using it for marketing and business development, or worrying about peer- or institutional pressure, or being afraid of being left behind—a clear picture emerges: MIS and ES surgery has become much more mainstream among surgeons in the industrialized Asian countries/regions than in other countries/regions with comparable advanced health care systems. This is corroborated by a large number of peer-reviewed journal articles having been published from China and Korea in the last five years. While there is no question that patient demand for less burdensome and simpler outpatient spinal decompression procedures (55-61) for common degenerative conditions of the lumbar spine has contributed to the increase in MIS and ES surgeries in North America and Europe (62), the lower rates of concern for these issues among Asian spine surgeons clearly indicates that the health care systems in the industrialized Asian countries/regions have created mechanisms to integrate MIS and ES surgeries into their coverage and treatment guidelines.
What also became apparent as a result of this survey is that surgeons in Asian countries/regions are much less likely to utilize informal sources of MIS and ES training such as small local meeting of like-minded peers. They were also less likely to report that National and International meetings were the primary sources of MIS and ES training suggesting that such training has been integrated in a formalized manner into the core curriculum of established training programs in their respective countries/regions. This is indeed corroborated by the fact that there was a statistically significantly higher number of self-reported MIS and ES master surgeons in Asian than amongst surgeons from non-Asian countries/regions. Besides, the percentage of Asian novice surgeons was nearly three times lower than amongst surgeons from other regions.
Spinal endoscopy is more frequently adopted by Asian surgeons residing in China, Japan and South Korea, who also seem to perform it at a higher self-reported skill level and employ it to a more significant percentage of their clinical practice. ES training in Asia seems better formalized while surgeons in North America and Europe are still left to wonder where and under whose mentorship to train for these advanced endoscopic procedures as industry-sponsored weekend cadaver workshops rarely can go beyond introducing the endoscopic instrumentation, and basic surgical technique, and offer little in the way of teaching appropriate diagnostic workup, surgical indications, management of complications, and procedural steps commensurate with the clinical context of the various common lumbar degenerative conditions. A steeper learning curve with the endoscopic lumbar spinal surgery has long been recognized by many in the field (63,64), and KOLs have voiced their concerns that the lack of formalized training with an accredited core curriculum could inadvertently give spinal endoscopy an unattractive “high-complication-rate” stigma (65) similar to traditional inpatient open lumbar spine surgery which in current public opinion has been associated with higher blood loss, and higher infection- and revision surgery rates (1,3,5,6,12,15). This training dilemma in countries/regions outside Asia with the lack of accredited formalized endoscopic training programs for spine surgeons is being compounded by some court rulings in the United States where patients have sued non-surgeons performing endoscopic lumbar surgeries and reprimanded by licensing boards for practicing outside the scope of their training in interventional pain management. These lawsuits were typically prompted by poor management of postoperative complications from surgical procedures performed by non-surgeons without formal surgical residency or fellowship training.
The growing evidence of lower complication rates with MIS and ES surgery has become common knowledge among patients (66-68), who are now actively seeking out surgeons and centers (57,58) to receive treatments for sciatica-type low back and leg pain that are less disruptive to their lives, allow earlier social reintegration, and return to work (55-60). From the surgeons point of view, the goals of introducing MIS and ES surgery into one’s routine surgical practice are aimed at reducing postoperative pain, the time to postoperative narcotic independence (69-72) and diminishing the burden of decompensated cardiopulmonary medical problems (66,73-76) often seen in the aging baby-boomer population who suffer the most from sciatica-type low back- and leg pain due to herniated disc and spinal stenosis (77).
Conclusions
This study indicates that spine surgeons from Asian countries/regions have implemented MIS and ES surgery as an integral part of their clinical practice and are performing it at a higher skill level in the majority of their patients. Training requirements for MIS and ES surgery and implementation of privileges vary in countries/regions. With increasing traction and patient demand, minimum adequate training will be part of the ongoing debate. While industry-sponsored weekend cadaver workshops have remained the mainstay of training aspiring endoscopic spinal surgeons in North America and Europe leaving many surgeons to becoming an autodidact, this survey suggests that training is better formalized in Asian countries/regions who deservingly may be considered the hotspot of MIS and ES surgery.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Hartman C, Hemphill C, Godzik J, et al. Analysis of cost and 30-day outcomes in single level transforaminal lumbar interbody fusion (TLIF) and less invasive, standalone lateral transpsoas interbody fusion (LIF). World Neurosurg 2019;122:e1037-40. [Crossref] [PubMed]
- Youn MS, Shin JK, Goh TS, et al. Endoscopic posterior decompression under local anesthesia for degenerative lumbar spinal stenosis. J Neurosurg Spine 2018;29:661-6. [Crossref] [PubMed]
- Ryu DS, Ahn SS, Kim KH, et al. Does minimally invasive fusion technique influence surgical outcomes in isthmic spondylolisthesis? Minim Invasive Ther Allied Technol 2019;28:33-40. [Crossref] [PubMed]
- Godzik J, Walker CT, Theodore N, et al. Minimally Invasive Transforaminal Interbody Fusion with Robotically Assisted Bilateral Pedicle Screw Fixation: 2-Dimensional Operative Video. Oper Neurosurg (Hagerstown) 2019;16:E86-7. [Crossref] [PubMed]
- Minamide A, Simpson AK, Okada M, et al. Microendoscopic Decompression for Lumbar Spinal Stenosis with Degenerative Spondylolisthesis: The Influence of Spondylolisthesis Stage (Disc Height and Static and Dynamic Translation) on Clinical Outcomes. Clin Spine Surg 2019;32:E20-6. [Crossref] [PubMed]
- Elmekaty M, Kotani Y, Mehy EE, et al. Clinical and Radiological Comparison between Three Different Minimally Invasive Surgical Fusion Techniques for Single-Level Lumbar Isthmic and Degenerative Spondylolisthesis: Minimally Invasive Surgical Posterolateral Fusion versus Minimally Invasive Surgical Transforaminal Lumbar Interbody Fusion versus Midline Lumbar Fusion. Asian Spine J 2018;12:870-9. [Crossref] [PubMed]
- Mueller K, Zhao D, Johnson O, et al. The Difference in Surgical Site Infection Rates Between Open and Minimally Invasive Spine Surgery for Degenerative Lumbar Pathology: A Retrospective Single Center Experience of 1442 Cases. Oper Neurosurg (Hagerstown) 2019;16:750-5. [Crossref] [PubMed]
- Park P, Fu KM, Mummaneni PV, et al. The impact of age on surgical goals for spinopelvic alignment in minimally invasive surgery for adult spinal deformity. J Neurosurg Spine 2018;29:560-4. [Crossref] [PubMed]
- Menger R, Hefner MI, Savardekar AR, et al. Minimally invasive spine surgery in the pediatric and adolescent population: A case series. Surg Neurol Int 2018;9:116. [Crossref] [PubMed]
- Khechen B, Haws BE, Patel DV, et al. Comparison of Postoperative Outcomes between Primary MIS TLIF and MIS TLIF as a Revision Procedure to Primary Decompression. Spine (Phila Pa 1976) 2019;44:150-6. [Crossref] [PubMed]
- Komatsu J, Muta T, Nagura N, et al. Tubular surgery with the assistance of endoscopic surgery via a paramedian or midline approach for lumbar spinal canal stenosis at the L4/5 level. J Orthop Surg (Hong Kong) 2018;26:2309499018782546. [Crossref] [PubMed]
- Fanous AA, Liounakos JI, Wang MY. Minimally Invasive Pedicle Subtraction Osteotomy. Neurosurg Clin N Am 2018;29:461-6. [Crossref] [PubMed]
- Anand N, Kong C. Can Minimally Invasive Transforaminal Lumbar Interbody Fusion Create Lordosis from a Posterior Approach? Neurosurg Clin N Am 2018;29:453-9. [Crossref] [PubMed]
- Choy W, Miller CA, Chan AK, et al. Evolution of the Minimally Invasive Spinal Deformity Surgery Algorithm: An Evidence-Based Approach to Surgical Strategies for Deformity Correction. Neurosurg Clin N Am 2018;29:399-406. [Crossref] [PubMed]
- Maugeri R, Basile L, Gulì C, et al. Percutaneous Pedicle-Lengthening Osteotomy in Minimal Invasive Spinal Surgery to Treat Degenerative Lumbar Spinal Stenosis: A Single-Center Preliminary Experience. J Neurol Surg A Cent Eur Neurosurg 2018;79:365-71. [Crossref] [PubMed]
- Kulkarni AG, Kantharajanna SB, Dhruv AN. The Use of Tubular Retractors for Translaminar Discectomy for Cranially and Caudally Extruded Discs. Indian J Orthop 2018;52:328-33. [Crossref] [PubMed]
- Tamburrelli FC, Meluzio MC, Burrofato A, et al. Minimally invasive surgery procedure in isthmic spondylolisthesis. Eur Spine J 2018;27:237-43. [Crossref] [PubMed]
- Park Y, Seok SO, Lee SB, et al. Minimally Invasive Lumbar Spinal Fusion Is More Effective Than Open Fusion: A Meta-Analysis. Yonsei Med J 2018;59:524-38. [Crossref] [PubMed]
- Verla T, Winnegan L, Mayer R, et al. Minimally Invasive Transforaminal Versus Direct Lateral Lumbar Interbody Fusion: Effect on Return to Work, Narcotic Use, and Quality of life. World Neurosurg 2018;116:e321-8. [Crossref] [PubMed]
- Pimenta L, Tohmeh A, Jones D, et al. Rational decision making in a wide scenario of different minimally invasive lumbar interbody fusion approaches and devices. J Spine Surg 2018;4:142-55. [Crossref] [PubMed]
- Kono Y, Gen H, Sakuma Y, et al. Comparison of Clinical and Radiologic Results of Mini-Open Transforaminal Lumbar Interbody Fusion and Extreme Lateral Interbody Fusion Indirect Decompression for Degenerative Lumbar Spondylolisthesis. Asian Spine J 2018;12:356-64. [Crossref] [PubMed]
- Yeung AT, Gore S. In-vivo Endoscopic Visualization of Patho-anatomy in Symptomatic Degenerative Conditions of the Lumbar Spine II: Intradiscal, Foraminal, and Central Canal Decompression. Surg Technol Int 2011;21:299-319. [PubMed]
- Yeung AT, Yeung CA. In-vivo endoscopic visualization of patho-anatomy in painful degenerative conditions of the lumbar spine. Surg Technol Int 2006;15:243-56. [PubMed]
- Yeung AT. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon's Experience Incorporating Adjunctive Techologies. SAS J 2007;1:108-17. [Crossref] [PubMed]
- Yeung AT. Lessons Learned from 27 Years’ Experience and Focus Operating on Symptomatic Conditions of the Spine under Local Anesthesia: The Role and Future of Endoscopic Spine Surgery as a “Disruptive Technique” for Evidenced Based Medicine. J Spine 2018;7:413. [Crossref]
- Shaikh S, Chung F, Imarengiaye C, et al. Pain, nausea, vomiting and ocular complications delay discharge following ambulatory microdiscectomy. Can J Anaesth 2003;50:514-8. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am 2007;38:363-72. [Crossref] [PubMed]
- Tsou PM, Alan Yeung C, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J 2004;4:564-73. [Crossref] [PubMed]
- Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: outcome and technique. Spine J 2002;2:41-8. [Crossref] [PubMed]
- Lewandrowski KU. “Outside-in” technique, clinical results, and indications with transforaminal lumbar endoscopic surgery: a retrospective study on 220 patients on applied radiographic classification of foraminal spinal stenosis. Int J Spine Surg 2014;8:26. [Crossref] [PubMed]
- Yeung AT. Intradiscal Therapy and Transforaminal Endoscopic Decompression: Op¬portunities and Challenges for the Future. J Neurol Disord 2016;4:303. [Crossref]
- Yeung A, Yeung CA. Endoscopic Identification and Treating the Pain Generators in the Lumbar Spine that Escape Detection by Traditional Imaging Studies. J Spine 2017;6:369.
- Yeung AT. Transforaminal Endoscopic Decompression for Painful Degenerative Conditions of The Lumbar Spine: A review of One Surgeon’s Experience with Over 10,000 Cases Since 1991. J Spine Neurosurg 2017;6:2.
- Yeung AT, Roberts A, Shin P, et al. Suggestions for a Practical and Progressive Approach to Endoscopic Spine Surgery Training and Privileges. J Spine 2018;7:414. [Crossref]
- North American Spine Society, 2018 Annual Meeting Los Angeles: Ticketed Session: Solution Showcase: Full Endoscopic Spine Surgery. Available online: http://www.nassannualmeeting.org/AM2018
- North American Spine Society, & 6th Emirates International Neurosurgical Conference NASS GSC: Beginner Endoscopic Solutions for Lumbar Disc Herniation, December 6-8, 2018. Available online: http://www.nassannualmeeting.org/AM2018
- ISMISS. NASSMISS 2018. 3rd Scientific combined meeting NASS / ISMISS, International 36th Course for Percutaneous Endoscopic Spinal Surgery, Sep 11, 2018. Available online: http://www.ismiss.com/4-0-meetings.html
- Surveygizmo. Typical Response Rates for Common Survey Types. Available online: https://www.surveygizmo.com/resources/blog/survey-response-rates/
- Pew research center methods. What Low Response Rates Mean for Telephone Surveys. Available online: https://www.pewresearch.org/methods/2017/05/15/what-low-response-rates-mean-for-telephone-surveys
- Genroe. The Complete Guide to Acceptable Survey Response Rates. Available online: https://www.genroe.com/blog/acceptable-survey-response-rate-2/11504
- National social norms center. What is an acceptable survey response rate? Available online: http://socialnorms.org/what-is-an-acceptable-survey-response-rate/
- Appetitive. Mobile Survey Response Rates: Averages and Benchmarks by App Category. Available online: http://www.apptentive.com/blog/2016/10/04/mobile-survey-response-rates/
- Officevibe. Mind-blowing Employee Survey Statistics. Available online: http://www.officevibe.com/blog/employee-surveys-infographic
- Morgan M. Millar, Don A. Dillman. Improving Response to Web and Mixed-Mode Surveys. Public Opin Q 2011;75:249-69. [Crossref]
- Promoter.7 Secret Ways to Increase Your Survey Response Rate. Available online: https://www.promoter.io/blog/increase-survey-responses
- Todd AL, Porter M, Williamson JL, Patterson JA, Roberts CL. Pre-notification letter type and response rate to a postal survey among women who have recently given birth. BMC Med Res Methodol 2015;15:104. [Crossref] [PubMed]
- Odgaard L, Kothari M. Survey of oral nursing care attitudes, knowledge and practices in a neurorehabilitation setting. J Oral Rehabil 2019;46:730-7. [PubMed]
- Dombrecht L, Deliens L, Chambaere K, et al. Neonatologists and neonatal nurses have positive attitudes towards perinatal end-of-life decisions, a nationwide survey. Acta Paediatr 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Brandt NJ, Cooke CE, Sharma K, et al. Findings from a National Survey of Medicare Beneficiary Perspectives on the Medicare Part D Medication Therapy Management Standardized Format. J Manag Care Spec Pharm 2019;25:366-91. [Crossref] [PubMed]
- Weber C, Lønne G, Rao V, et al. Surgical management of lumbar spinal stenosis: a survey among Norwegian spine surgeons. Acta Neurochir (Wien) 2017;159:191-7. [Crossref] [PubMed]
- Anand N, Agrawal A, Burger EL, et al. The Prevalence of the Use of MIS Techniques in the Treatment of Adult Spinal Deformity (ASD) Amongst Members of the Scoliosis Research Society (SRS) in 2016. Spine Deform 2019;7:319-24. [Crossref] [PubMed]
- Joeris A, Knoll C, Kalampoki V, et al. Patient-reported outcome measurements in clinical routine of trauma, spine and craniomaxillofacial surgeons: between expectations and reality: a survey among 1212 surgeons. BMJ Open 2018;8:e020629. [Crossref] [PubMed]
- Wang J, Alotaibi NM, Ibrahim GM, et al. The Spectrum of Altmetrics in Neurosurgery: The Top 100 "Trending" Articles in Neurosurgical Journals. World Neurosurg 2017;103:883-95.e1. [Crossref] [PubMed]
- Lin GX, Kotheeranurak V, Mahatthanatrakul A, et al. Worldwide research productivity in the field of full-endoscopic spine surgery: a bibliometric study. Eur Spine J 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Zahrawi F. Microlumbar discectomy. Is it safe as an outpatient procedure? Spine (Phila Pa 1976) 1994;19:1070-4. [Crossref] [PubMed]
- Bookwalter JW 3rd, Busch MD, Nicely D. Ambulatory surgery is safe and effective in radicular disc disease. Spine (Phila Pa 1976) 1994;19:526-30. [Crossref] [PubMed]
- Mancuso CA, Duculan R, Cammisa FP, et al. Fulfillment of patients' expectations of lumbar and cervical spine surgery. Spine J 2016;16:1167-74. [Crossref] [PubMed]
- Mancuso CA, Duculan R, Cammisa FP, et al. Proportion of Expectations Fulfilled: A New Method to Report Patient-centered Outcomes of Spine Surgery. Spine (Phila Pa 1976) 2016;41:963-70. [Crossref] [PubMed]
- Tabibian BE, Kuhn EN, Davis MC, et al. Patient Expectations and Preferences in the Spinal Surgery Clinic. World Neurosurg 2017;106:595-601. [Crossref] [PubMed]
- Stambough JL. Matching patient and physician expectations in spine surgery leads to improved outcomes. Spine J 2001;1:234. [Crossref] [PubMed]
- Mehrotra A, Sloss EM, Hussey PS, et al. Evaluation of a center of excellence program for spine surgery. Med Care 2013;51:748-57. [Crossref] [PubMed]
- Adam Schrag 20 things to know about minimally invasive spine surgery. March 01, 2017. Available online: https://www.beckersspine.com/mis/item/35569-20-things-to-know-about-minimally-invasive-spine-surgery.html
- Lee CW, Yoon KJ, Jun JH. Percutaneous Endoscopic Laminotomy with Flavectomy by Uniportal, Unilateral Approach for the Lumbar Canal or Lateral Recess Stenosis. World Neurosurg 2018;113:e129-37. [Crossref] [PubMed]
- Yeung AT. The Role and Future of Endoscopic Spine Surgery. Continuous Research Online Library. ContROL 2017;1:1.
- Kim HS, Paudel B, Jang JS, et al. Percutaneous Full Endoscopic Bilateral Lumbar Decompression of Spinal Stenosis Through Uniportal-Contralateral Approach: Techniques and Preliminary Results. World Neurosurg 2017;103:201-9. [Crossref] [PubMed]
- McClelland S 3rd, Goldstein JA. Minimally Invasive versus Open Spine Surgery: What Does the Best Evidence Tell Us? J Neurosci Rural Pract 2017;8:194-8. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 2016;24:416-27. [Crossref] [PubMed]
- Goldstein CL, Macwan K, Sundararajan K, et al. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res 2014;472:1727-37. [Crossref] [PubMed]
- Zolot J. A Worsening Opioid Epidemic Prompts Action. Am J Nurs 2017;117:15. [PubMed]
- Cheatle MD. Facing the challenge of pain management and opioid misuse, abuse and opioid-related fatalities. Expert Rev Clin Pharmacol 2016;9:751-4. [Crossref] [PubMed]
- Hupp JR. The Surgeon's Roles in Stemming the Prescription Opioid Abuse Epidemic. J Oral Maxillofac Surg 2016;74:1291-3. [Crossref] [PubMed]
- Kee JR, Smith RG, Barnes CL. Recognizing and Reducing the Risk of Opioid Misuse in Orthopaedic Practice. J Surg Orthop Adv 2016;25:238-43. [PubMed]
- Su AW, Habermann EB, Thomsen KM, et al. Risk Factors for 30-Day Unplanned Readmission and Major Perioperative Complications After Spine Fusion Surgery in Adults: A Review of the National Surgical Quality Improvement Program Database. Spine (Phila Pa 1976) 2016;41:1523-34. [Crossref] [PubMed]
- Kim BD, Smith TR, Lim S, et al. Predictors of unplanned readmission in patients undergoing lumbar decompression: multi-institutional analysis of 7016 patients. J Neurosurg Spine 2014;20:606-16. [Crossref] [PubMed]
- Modhia U, Takemoto S, Braid-Forbes MJ, et al. Readmission rates after decompression surgery in patients with lumbar spinal stenosis among Medicare beneficiaries. Spine (Phila Pa 1976) 2013;38:591-6. [Crossref] [PubMed]
- Kocher KE, Nallamothu BK, Birkmeyer JD, et al. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood) 2013;32:1600-7. [Crossref] [PubMed]
- Yeung AT, Yeung CA, Salari N, et al. Lessons Learned Using Local Anesthesia for Minimally Invasive Endoscopic Spine Surgery. J Spine 2017;6:377. [Crossref]