
Safety and efficacy of direct nerve root decompression via anterior cervical discectomy and fusion with uncinectomy for cervical radiculopathy
Introduction
Cervical radiculopathy is among the most common adult spinal disorders. There is an annual incidence of 107.3 per 100,000 for men and 63.5 per 100,000 for women with a peak incidence in the fourth and fifth decades of life (1,2). Patients with cervical radiculopathy typically present with a combination of pain, paresthesias, sensory deficits, or weakness in specific dermatomal and myotomal distributions. In many cases the diagnosis can be made through a detailed history alone (3). A summary of the sensory and motor findings associated with cervical radiculopathy are highlighted in Table 1.

Full table
Although posterior cervical foraminotomy and conventional anterior cervical discectomy and fusion (ACDF) are the mainstays of treatment for cervical radiculopathy, in a subset of patients with severe bony foraminal stenosis these conventional surgical techniques may result in incomplete nerve root decompression and persistent neurological symptoms. Patient with radiculopathy due to severe bony foraminal stenosis may be candidates for ACDF with complete uncinectomy to achieve complete nerve root decompression. Several studies have demonstrated the feasibility of anterior cervical uncinectomy/foraminotomy (4-7); however, it is a technically demanding procedure that requires careful patient selection and special care to avoid injuring the vertebral artery and exiting nerve root. We describe the technique for ACDF with complete uncinectomy for the treatment of cervical radiculopathy due bony foraminal stenosis, with or without concurrent myelopathy.
Preoperative evaluation
Initial evaluation begins with a detailed history and physical exam. The diagnosis of cervical radiculopathy often can be made by history alone. Physical exam often includes provocative testing including the Spurling test, shoulder abduction test, Valsalva maneuver, and Elveys upper limb tension test (ULTT). Each of these maneuvers results in narrowing of the neural foramen and attempts to reproduce the patient’s symptoms (3,8). The Spurling test is the most sensitive and specific when combined with rotation and extension (8). The shoulder abduction tests assessed for symptom relief with shoulder abduction as the nerve is taken off tension. Increased pain with the Valsalva maneuver and traction of the upper extremity (ULTT) are not well studied. The presence of radiculopathy should prompt an assessment for myelopathy which includes a history of hand clumsiness, difficulty with fine motor task, gait instability, bowel/bladder control issues, as well physical exam findings of hyperreflexia and impaired gait. The presence of cervical radiculopathy with a concomitant peripheral nerve entrapment, the so called “double crush”, should also be excluded. Electromyography (EMG) is often helpful in this scenario. Lastly, shoulder pathology must be excluded since shoulder girdle pain is a common presenting symptom of cervical radiculopathy (9).
Careful review of the preoperative imaging must be performed before proceeding with surgery. AP/lateral cervical X-rays can demonstrate spondylosis and decreased disc height as well as uncinate hypertrophy. Oblique cervical X-rays are especially helpful in demonstrating bony foraminal stenosis and is obtained routinely by the authors. Dynamic imaging (flexion/extension X-rays) is also obtained to rule out any instability. Magnetic resonance imaging (MRI) should be reviewed to confirm foraminal stenosis at the expected level and to assess the spinal cord. Computed tomography (CT) scans can confirm the finding of foraminal stenosis and identify osteophytes or uncinate hypertrophy as the offending etiology. Oblique reconstruction of the cervical spine CT can be especially helpful in demonstrating bony foraminal stenosis.
Surgical technique
Patients are positioned supine on a flatbed Jackson table and undergo general endotracheal intubation. Special care is taken to pad all bony prominences. The patient position as close to the foot of the operating table as possible, so that there is enough room at the cranial end to accommodate the C-arm fluoroscope and prevent it from interfering with the surgeon’s working space. Intraoperative neuromonitoring can be used at the discretion of the treating surgeon.
A folded sheet is placed under the shoulders to provide gentle neck extension. Gentle downward shoulder traction is obtained with 6-inch tape. The neck is prepped and draped in the usual sterile fashion with the skin incision planned using the patient’s native skin crease closest to the intended level(s). The operating microscope is brought into position and a standard Smith-Robinson approach is used to access the spine. The intended level is confirmed with fluoroscopy using a clamp on the longus colli muscle to prevent iatrogenic disc injury from spinal needle in case if the initial localization if off. An assistant retracts the trachea and esophagus medially while a cuff of longus colli muscle is elevated bilaterally with bipolar cautery. Bed-mounted retractors are secured under the muscle cuff and secured to the bed to provide wide, uncinate-to-uncinate exposure.
A standard cervical discectomy is then performed, with preservation of PLL on the side of planned uncinectomy so that the dura is protected during uncinectomy. The lateral border of the uncinate is then identified and a Penfield no. 4 dissector is used to gently dissect the soft tissues, including the vertebral artery, off of the lateral border of the uncinate. One can leave the Penfield 4 or switch to a Penfield No. 2 dissector to protect the artery during the uncinectomy. Alternatively, a ¼ by ¼ cotton patty can be placed lateral to the uncinate to serve as a soft dissector and to protect the vertebral artery. A larger patty can occlude the artery and so prolonged use should be avoided. Soft tissue overlying the uncinate can be carefully removed using monopolar cautery on low setting as the patty and Penfield #2 dissector serves to protect the vertebral artery laterally.
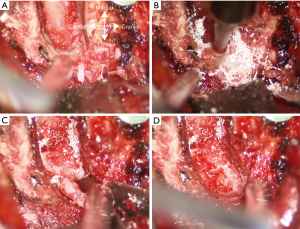
The uncinectomy is performed using a high-speed 2.5 or 3 mm matchstick burr starting as close to the lateral border of the uncinate as possible, while leaving a thin rim of bone to protect the vertebral artery. This is carried down slowly two thirds of the way down with frequent stopping to directly visualize the burr tip (Figure 1). This requires great care to ensure that the burr does not injure the underlying nerve root. Once the ventral 2/3 of the uncinate has been thinned out, the residual dorsal 1/3 can be removed in a medial to lateral fashion to reduce the chance of nerve root injury. Burring is stopped when only a thin rim of bone is left. The egg-shelled bone fragment can then be carefully removed using a small up-going curette. The PLL on the side of uncinectomy is then removed using a Kerrison rongeur. After ensuring complete decompression of the nerve root, meticulous hemostasis is obtained using hemostatic matrix and cotton patties.
The remainder of the procedure is the same as a standard ACDF with bone grafting and anterior cervical plating. We prefer to use custom-cut frozen iliac crest allograft to maximize the surface area of graft-bone interface to maximize fusion potential and to minimize subsidence. The wound is irrigated and closed in a usual fashion with absorbable sutures and with a surgical drain. We prefer a ¼ inch Penrose drain since it has a bigger diameter and less likely to be clogged.
Postoperative management and complications
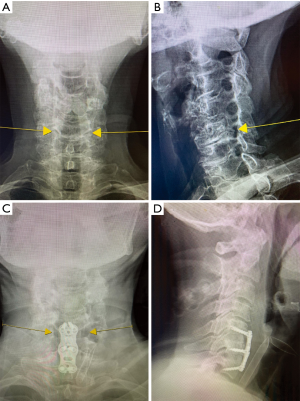
Common complications related to the anterior cervical approach include dysphagia, vocal cord paralysis, and tracheal/esophageal injury. Dysphagia is generally transient and can be treated with a short course of steroids in severe cases. Less common complications include injury to the vertebral artery, spinal cord or nerve root, cerebrospinal fluid leak, and wound infection. Postoperative cervical X-rays with oblique views can demonstrate removal of the hypertrophic uncinate with decompression of the associated neural foramen (Figure 2).
Surgical outcomes
A retrospective review of the last author’s (LAT) single-surgeon experience on ACDF with uncinectomy was performed. A total of 152 uncinectomies were performed in 52 patients undergoing ACDF. Mean age was 58 years (range, 31–77 years) with 56% women. Among these patients, 62% presented with pure radiculopathy, while 38% had radiculopathy with myelopathy. Mean estimated blood loss (EBL) was 45 mL and average length of stay was 3 days. The levels of uncinectomies performed were as follows: five at C3/4, 41 at C4/5, 49 at C5/6, 52 at C6/7, and six at C7/T1. There were three complications in this series. One patient developed transient recurrent laryngeal nerve palsy with vocal cord paralysis that had completely resolution at 6 months. A second patient developed transient C5 palsy which completely resolved at 6 months. The third patient suffered a mechanical fall related to a seizure disorder three months after surgery that resulted in acute graft subsidence requiring reoperation and posterior foraminotomy. There were no vertebral artery injuries, cerebrospinal fluid (CSF) leaks, or wound infections.
Clinical outcomes were assessed by comparing health-related quality of life (HRQOL) measurements preoperatively and at six months. These included the Neck Disability Index (NDI), EuqoQOL-5D (EQ-5D), and Visual Analog Scale (VAS) for neck and arm pain. Mean NDI decreased from 0.43±0.20 to 0.34±0.22 (P=0.15), EQ-5D improved from 0.49±2.6 to 0.72±0.21 (P=0.0005), VAS-neck decreased from 5.81±2.73 to 2.44±2.90 (P=0.0003), and VAS-arm decreased from 4.05±3.48 to 1.62±2.19 (P=0.0015). Among 91 uncinectomies performed to treat myotome-specific weakness, 80 (88%) improved, 10 (11%) had no change, and 1 (1%) worsened at the 6-week follow-up visit. The patient who worsened had a C4/5 uncinectomy with associated C5 palsy that completely resolved by the 6-month follow-up visit. Among 66 uncinectomies performed for dermatome-specific numbness, 57 (86%) were associated with complete resolution and 9 (14%) with no improvement at 6 weeks. No patient developed worsening sensory symptoms.
Conclusions
ACDF with uncinectomy is a safe and effective treatment for patients with cervical radiculopathy with or without myelopathy, especially in those with severe bony foraminal stenosis. Spine surgeons should keep this technique in their armamentarium to provide optimal surgical outcome in appropriately selected patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. LAT serves as the unpaid editorial board member of Journal of Spine Surgery from Jan. 2019 to Jan. 2021 and served as the unpaid Guest Editor of the series. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kelsey JL, Githens PB, Walter SD, et al. An epidemiological study of acute prolapsed cervical intervertebral disc. J Bone Joint Surg Am 1984;66:907-14. [Crossref] [PubMed]
- Radhakrishnan K, Litchy WJ, O'Fallon WM, et al. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994;117:325-35. [Crossref] [PubMed]
- Wainner RS, Gill H. Diagnosis and nonoperative management of cervical radiculopathy. J Orthop Sports Phys Ther 2000;30:728-44. [Crossref] [PubMed]
- Chen BH, Natarajan RN, An HS, et al. Comparison of biomechanical response to surgical procedures used for cervical radiculopathy: posterior keyhole foraminotomy versus anterior foraminotomy and discectomy versus anterior discectomy with fusion. J Spinal Disord 2001;14:17-20. [Crossref] [PubMed]
- Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: a new approach to cervical disc herniation. J Neurosurg 1996;84:155-60. [Crossref] [PubMed]
- Johnson JP, Filler AG, McBride DQ, et al. Anterior cervical foraminotomy for unilateral radicular disease. Spine (Phila Pa 1976) 2000;25:905-9. [Crossref] [PubMed]
- Saringer W, Nobauer I, Reddy M, et al. Microsurgical anterior cervical foraminotomy (uncoforaminotomy) for unilateral radiculopathy: clinical results of a new technique. Acta Neurochir (Wien) 2002;144:685-94. [Crossref] [PubMed]
- Rubinstein SM, Pool JJ, van Tulder MW, et al. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J 2007;16:307-19. [Crossref] [PubMed]
- Rhee JM, Yoon T, Riew KD. Cervical radiculopathy. J Am Acad Orthop Surg 2007;15:486-94. [Crossref] [PubMed]


