Sagittal alignment of the cervical spine: do we know enough for successful surgery?
Introduction
Restoration of the spine’s sagittal profile has been recognised as an important objective in adult deformity surgery (1). Early studies have focused mainly on achieving sagittal spinal balance—as determined by the sagittal vertical axis (SVA)—and the relationship between lumbar lordosis (LL) and pelvic incidence (PI). These concepts are still actively evolving but remain good guidelines which govern the basis of adult deformity surgery of the thoracic and lumbar spine.
In contrast, cervical spine alignment targets are less well established. This is due partly to the large variation in cervical spine alignment across normal individuals (2,3), as well as the conflicting evidence regarding cervical spine alignment and clinical outcomes (4,5). Unlike the lumbar spine that is almost always lordotic, cervical spine alignment varies based on the need to maintain horizontal gaze and to compensate for more caudal spinal alignment changes.
Burgeoning interest in this field of research over the past decade has furthered our understanding of the sagittal alignment parameters which influence clinical outcomes. It was once thought that restoration of cervical lordosis was the sole end goal for surgery to the cervical spine. This is now known to be just one part of the puzzle, with the complex interplay between local and regional cervical alignment, as well as with the caudal spinopelvic complex and global sagittal balance as a whole being gradually explicated. We present here a synthesis of the currently available evidence surrounding the sagittal alignment of the cervical spine.
Radiographic sagittal cervical spine alignment parameters
There have been myriad radiographic parameters used to define sagittal alignment of the cervical spine (6), with no consensus as to which should be used, unlike in the caudal spine segments where more established guidelines exist for measurement of deformity angles (7). Table 1 shows some of the most frequently used parameters for cervical spine sagittal alignment, with some newly proposed parameters shown in Table 2.

Full table

Full table
‘Normal’ cervical spine alignment
With cervical fusion continuing to be the gold standard procedure for numerous cervical spine pathologies, it is vital to recognise the normal variations in cervical spine sagittal profile which in turn will help determine the optimal cervical spine alignment for fusion for each individual to maximise function while minimising complications. Unlike the lumbar spine which should almost invariably be lordotic to enable bipedal standing, and likewise the thoracic spine which should be kyphotic for the ribcage to counterbalance the caudal lumbar spine, cervical spine alignment varies considerably. This is due to the need for the cervical spine to balance overall caudal alignment changes with the impetus to maintain horizontal gaze. Conventional wisdom on the ‘normal’ lordotic cervical spine (8) likely does not apply universally, and is still being debated in the current literature.
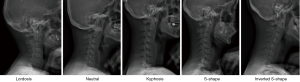
The cervical spine takes one of five distinct sagittal profiles—lordosis, neutral, kyphosis, S-shaped, and inverted S-shaped (Figure 1) (9-11). Whether or not lordosis should be the expected finding in the cervical spine is still under question. Several studies have investigated the cervical spine alignment in asymptomatic subjects and have found that significant proportions did not have lordotic cervical spines. Takeshima et al. (9) found that only about 23.5% of their study cohort had cervical lordosis with 26%, 19.6%, 17.6% and 13.2% of their cohort falling within the other subgroups. Hey et al. (11) similarly found that only 27% of their asymptomatic cohort had cervical spine lordosis. Another study (12) classified their cohort of asymptomatic volunteers into lordotic and non-lordotic subtypes, with the latter being further subclassified into straight, sigmoid and kyphotic patterns. In that study with 10-year follow up, only 44.6% of subjects under 40 years or 55.8% of subjects overall had lordotic cervical spines. A recent meta-analysis of 15,364 asymptomatic subjects found that approximately 36% of them had non-lordotic cervical spines (13).
Lordotic vs. non-lordotic sagittal profiles—is the latter pathological?
The evidence correlating these sagittal alignment subtypes to clinical symptoms is mixed and inconclusive. A study of young patients (14) found no significant difference in pain scores between various cervical spine alignment subgroups, and concluded that the differences in cervical spine alignment was not due to degenerative changes or muscular spasm. In addition, they theorised that the postural habits of modern society such as the need for television/computer gazing and reading may be responsible for the change in cervical spine alignment with time. This is in line with the concept of ligamentous muscular counterbalancing (LMC) recently proposed by Hey et al. (15), which describes the natural tendency of every individual to adopt energy-conserving postures—there is a resultant impetus towards spinal kyphosis in order to rely on the posterior tension band of the spine. Yu et al. (10) studied the cervical spine alignment in a Chinese population, finding that the sagittal alignment in an asymptomatic cohort and those with symptomatic cervical spondylosis, was not significantly different. Patients with whiplash injuries have also been shown to have a similar cervical spine alignment distribution compared to an asymptomatic cohort (16), suggesting that loss of lordosis may not be a result of neck pain. It raises the clinical concern as to whether the restoration of lordosis for every patient undergoing cervical fusion is an appropriate surgical strategy. Cervical lordosis may not truly be physiological in every individual (11), and better outcomes may be achieved with patient-specific realignment targets.
The other school of thought is that a loss of cervical lordosis is always a pathological event, and that the lack of symptoms may simply mean that they have not yet had time to develop. A correlation has been reported between patients with acute or chronic neck pain and reduced cervical lordosis below 20° compared to asymptomatic subjects (12). Another study showed that global cervical sagittal alignment correlated with health-related quality of life indices (17); a kyphotic cervical spine theoretically places the neck musculature at more strain when supporting the weight of the head, with persistently increased pressures on the intervertebral discs resulting in accelerated degeneration and worsening deformity. This finding is also highlighted in several other studies in which a kyphotic cervical spine predisposed patients to an increased risk of developing neck pain (4,12) and neurovascular deficit including cervical myelopathy (18).
Overall alignment reflects a combination of angular and translational parameters
The concept of cervical sagittal balance has continued to evolve over the past decade. It suggests that it may not be the shape of the cervical spine alone that is important, but how this shape achieves global cervical sagittal balance and balance with the entire spinopelvic column. A commonly used translational marker for cervical spine sagittal balance is the C2-C7 SVA. Iyer et al. (19) found that in patients undergoing cervical spine surgery, their pre-operative sagittal alignment correlated to the degree of reported disability—higher C2-C7 SVA values predicted higher neck disability index (NDI) values, while higher values of cervical lordosis and T1-slope correlated to lower NDI scores. A multi-centre trial from North America of 56 patients with cervical spondylotic myelopathy undergoing surgery found that pre-operative C2-C7 SVA, but not C2-C7 lordosis (or kyphosis) were associated with modified Japanese Orthopaedic Association scores (20). Interestingly, they found that while in lordotic cervical spines the lower spinal cord cross sectional area on MRI correlated with lower mJOA scores as expected, in kyphotic cervical spines an inverse relationship was seen. These findings were echoed by Mohanty et al. (21); in their study of 124 patients undergoing surgery for cervical spondylotic myelopathy, patients with cervical kyphosis had increased T2 spinal cord signal on MRI and lower mJOA scores with increasing C2-C7 SVA, whereas those with cervical lordosis did not display this same relationship. These findings suggest that it is the combination of cervical spine sagittal morphology and balance, represented by both angular (kyphosis or lordosis) and translational parameters, that is important in determining patient outcomes.
Horizontal gaze and its effect on cervical sagittal alignment
Gaze direction in the sagittal plane is thought to be one of the major drivers of cervical sagittal alignment, and the ability to maintain horizontal gaze is a crucial goal in realignment surgeries. The current most widely used radiographic surrogate for this is the CBVA, first described for use by Simmons in the early 90s clinically and subsequently via clinical photographs. Its importance has been emphasised by its inclusion in the recently introduced Ames-ACD cervical deformity classification system (22). A CBVA ranging from 10–20° was associated with the highest degree of satisfaction in patients with ankylosing spondylitis (23). Overcorrection of CBVA in patients with ankylosing spondylitis is associated with poorer patient satisfaction with regard to gaze-related activities (24).
While several authors have reported successful surgical correction of CBVA and improvements in horizontal gaze following correction of cervicothoracic deformity (25,26), direct evidence relating CBVA correction to improved patient reported outcomes is limited. Lafage et al. (27) found that in their cohort of 303 patients who had not undergone any surgery, CBVA values correlated with Oswestry Disability Index (ODI) scores. ODI scores were however only available for less than a third of their original cohort. A study by Diebo et al. (28) looked into the associations between the various spinal alignment parameters and horizontal gaze in patients without neck symptoms and found that 29% of their patient cohort was still able to maintain horizontal gaze with a kyphotic cervical spine. They concluded again that cervical kyphosis alone may not be universally abnormal, and it is its relationship with overall spinal sagittal alignment which is important.
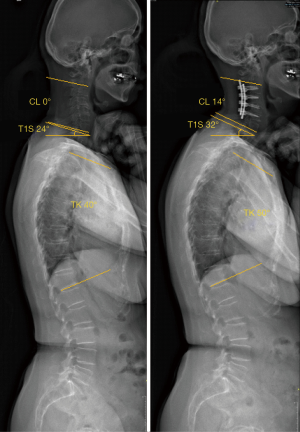
Radiographic assessment of gaze direction and horizontal gaze
Several studies (27,29) have pointed out that CBVA (Figure 2A) measurements are often not possible on standard lateral cervical spine radiographs due to exclusion of the relevant anatomical landmarks, and as such other markers of horizontal gaze have been proposed (30) including the slope of line of sight (Figure 2B) and McGregor’s slope (Figure 2C), both of which have been found to correlate well with CBVA (29). Hey et al. (30) previously showed that the assessment of horizontal gaze is often confounded by inconsistencies in patient posture during imaging despite standardised verbal and visual protocols. In that study, only about 75% of the study subjects capable of assuming horizontal gaze did so during imaging, and this was improved with stringent enforcement of measures such as a visual target, closer supervision by the radiographer, and the rejection of radiographs with suboptimally-positioned patients. The authors described a direct method of determining gaze direction based on the ‘3-6-12 rule’, referring to a mean vertical offset from the sella turcica of 3 mm, and a 6° horizontal convergence angle made by an imaginary line adjoining the centre of orbit to the internal occipital protuberance, both with 95% confidence interval of ±12 mm or degrees respectively (Figure 2D). These landmarks are more commonly visible on conventional cervical X-rays and the method can be employed both on EOS and conventional X-ray images.
Relationship between cervical spine alignment and caudal spine segments
The high degree of mobility of the cervical spine allows it to compensate for alignment changes caudally. Most consistently, a T1-slope is known to correlate with sagittal alignment of the cervical spine, with larger T1-slopes corresponding to larger degrees of cervical lordosis (11,19,31,32) in asymptomatic adults. This is an unsurprising finding given T1 is simply an extension of the adjacent cervical spine. In the same vein, T1-slope also reflects the degree of thoracic kyphosis, and accordingly increased thoracic kyphosis typically correlates to increased cervical lordosis (10,31,33), as the cervical spine compensates to maintain horizontal gaze. The converse also holds true, wherein decreased thoracic kyphosis is found to associate with the development of cervical kyphosis (34).
SVA is the other important parameter relating the sagittal alignment of the cervical spine to the caudal spine segments (15), and reflecting overall global sagittal balance. Apart from needing to counterbalance a large thoracic kyphosis and a high T1-slope, the need for compensatory cervical lordosis also increases in the presence of positive global sagittal balance. In these patients with positive spinal or whole body balance, cervical lordosis increases in an attempt to keep the body within the cone of economy, although the impact of this is likely less profound than that of T1-slope (11). Moreover, the same phenomenon is observed with changes in posture. It has been shown that when transitioning from a standing to sitting position, T1-slope, thoracic kyphosis and global SVA all increase with a resultant increase in cervical lordosis, and vice-versa (35).
Despite relatively consistent correlations shown between adjacent segments of the caudal spinopelvic complex—for instance between PI and LL (36), PI, pelvic tilt and sacral slope (37), thoracic kyphosis and LL (38)—all these studies looking at sagittal balance interrelationships have failed to find similar correlations between non-adjacent spinal segments (e.g., between lumbar and cervical lordosis).
Cervical spine sagittal alignment fusion targets—lordosis or kyphosis?
The relationship between sagittal cervical spine alignment and symptoms in patients prior to undergoing surgery remains imprecise, and the evidence for its influence on post-operative clinical outcomes is similarly mixed. It is generally accepted that in patients undergoing cervical fusion surgery for a variety of indications, fusion in kyphosis—whether regional or global—should be avoided as it is thought to lead to increased rates of adjacent segment degeneration (39,40). It has been demonstrated biomechanically that intradiscal pressures increased more in cervical spine segments adjacent to increasingly kyphotic fused segments, as the force required to maintain horizontal gaze increased with worsening forward imbalance (41). Restoration of cervical lordosis allows optimal distribution of weight to the posterior column of the cervical spine and more efficient energy expenditure by the neck muscles.
Despite this, the evidence linking this to clinical outcomes is not robust. A systematic review by Hansen et al. (40) found only a low level of evidence supporting post-fusion global or segmental kyphosis resulting in higher rates of adjacent segment degeneration. This review however contained only five retrospective studies, with only one looking at sagittal balance as a separate entity (and not merely as a construct of cervical lordosis or kyphosis). Additionally the International Spine Study Group recently reviewed their multi-centre database of patients undergoing surgical cervical deformity correction, identifying several factors predisposing patients to distal junctional kyphosis following cervical fusion (42). These included significant pre-operative sagittal imbalance (C2-C7 SVA >56.3 mm) and cervical kyphosis (>12°). These parameters were not however assessed on post-operative radiographs, and so we are unable to draw any conclusions regarding the adequacy of alignment correction. Finally, there is some early evidence to suggest that kyphotic segmental fusions may result in increased axial neck symptoms (43,44).
Is avoidance of kyphotic fusion, enough to achieve good outcomes? Villavicencio et al. (5) found that patients in whom the fused segment alignment was maintained or more lordosed post-operatively had larger improvements in post-operative NDI and Short Form-36 (SF-36) physical component summary (PCS) scores compared to those in whom the fused segments became more kyphosed. They did not however find any correlation between global cervical spine alignment and post-operative outcomes. In contrast, Tang et al. (4) reported that patients with worse cervical spinal imbalance (higher C2-C7 SVA values) had worse SF-36 PCS and NDI scores, and proposed a target threshold value of 40 mm for post-operative C2-C7 SVA to define cervical sagittal malalignment. These findings were supported by Roguski et al. (45) who corroboratively found that post-operative C2-C7 SVA values of patients with cervical spondylotic myelopathy were inversely correlated with SF-36 PCS and mJOA scores at 1 year, but not NDI.
Are fusion outcomes related to type of approach?
The potential risks and benefits of anterior versus posterior sagittal spinal realignment are well described, and it is possible that the inherent differences in surgical morbidity between the two approaches could theoretically confound interpretation of patient-reported results. This may be related to factors such as the adequacy of decompression, strength in correcting and maintaining spinal alignment, as well as influence on stabilising structures of the spine. Cabraja et al. (46) compared 48 patients undergoing surgery for cervical spondylotic myelopathy via either anterior or posterior approaches, finding that there was more correction of C2-C7 lordosis in the anterior group compared to the posterior group, where the cervical spine actually became more kyphosed at mean follow up durations of over two years, post-operatively. They also reported marginally more loss of correction in the anterior versus posterior groups. All patients however had improved mJOA scores with no significant difference between the two groups. Recent systematic reviews comparing outcomes of anterior and posterior surgery (47,48) did not find any difference in improvement in mJOA scores, but also did not look into patient-reported outcome scores. Fehlings et al. (49) found no differences in disease-specific and global patient outcome scores between the two approaches, and while a more recent study did report statistically superior outcomes for the anterior approach, this was found not to be clinically significant (50). It appears based on current evidence that the approach in itself does not account for differences in outcome.
Are fusion outcomes more dependent on pre-operative alignment?
The dearth of direct evidence linking sagittal imbalance to poorer surgical outcomes may reflect its overemphasised importance as a surgical goal. Shamji et al. (51) found that patients with cervical kyphosis pre-operatively demonstrated poorer mJOA recovery compared to those with cervical lordosis. Of note, they reported that this dichotomy in outcomes persisted despite restoration of cervical lordosis. Eighty-seven percent of their subgroup of 42 patients with pre-operative cervical kyphosis achieved cervical lordosis post-operatively and owing to the relatively small numbers, no comparison was possible with patients in whom sagittal alignment was not sufficiently corrected. More likely, it may simply be a matter of insufficient follow up duration, and that the adverse effects of sagittal imbalance take time to manifest. Longer-term follow up studies may be illuminating in this regard. More work is also required to elucidate the appropriate degree to which correction of cervical alignment should be attempted.
Sagittal alignment changes following spinal fusion surgery in the cervical and caudal spinal segments
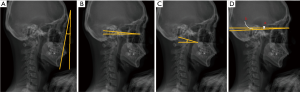
Reciprocal changes in sagittal alignment of the cervical and thoracolumbar spine often occur following corrective fusion surgery. Ha et al. (52) retrospectively reviewed their cohort of adult patients undergoing thoracolumbar deformity correction surgery finding that restoration of global sagittal alignment reduced the compensatory curve of the cervical spine (representative example in Figure 3); patients with more lordotic cervical spines with higher C7 SVA values pre-operatively had reduced cervical lordosis post-operatively, and vice-versa. This phenomenon was also reported independently by the International Spine Study Group (53) and Blondel et al. (54) following lumbar pedicle subtraction osteotomy with correction of global sagittal balance. They later compared patients with thoracolumbar spinal deformities who did or did not undergo corrective surgery, finding that those who underwent surgery were significantly more likely to develop cervical sagittal imbalance at up to two years post-operatively (55). Additionally, C2-C7 SVA worsening was associated with worse ODI scores at 1 year.
At the same time, pre-operative cervical sagittal balance also influences outcomes of surgery on the caudal spine. Scheer et al. (56) found that in patients undergoing thoracolumbar deformity correction, those with pre-operative cervical sagittal imbalance (defined at C2-C7 SVA >40 mm) had worse outcomes than those without. 53.5% of their cohort had persistent cervical sagittal imbalance post-operatively but again due to small subgroup numbers, no comparison was possible against those who had their imbalance corrected.
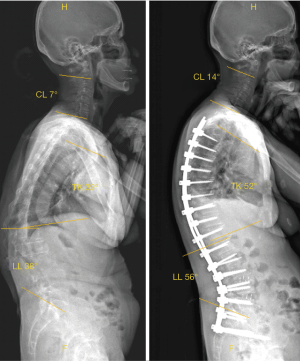
The converse relationship is also seen, with surgical alteration of cervical sagittal alignment affecting adjacent thoracic spine alignment. Lee et al. (57) found that surgical correction of cervical kyphosis resulted in concordant increases in T1-slope and thoracic kyphosis (representative example in Figure 4). The same correction of cervical spine alignment has however not been consistently seen in patients with adolescent idiopathic scoliosis (AIS) undergoing corrective surgery. Higher proportions of AIS patients were found to have hypolordotic or frankly kyphotic cervical spines pre-operatively, related to relative thoracic hypokyphosis (2,34,58). All these studies however, have consistently found that despite adequate restoration of thoracic kyphosis, cervical sagittal alignment does not become more lordotic as expected, and in some instances, it even decompensates and becomes more kyphotic. More recently, Pepke et al. (59) have found that while subaxial cervical lordosis (C2-C7) similarly did not increase in AIS patients post-operatively, there was a consistent increase in lordosis if the cervicothoracic junction was included (C2-T3). This suggests that compensatory alignment changes may be present and the use of functional landmarks such as inflexion vertebrae to assess sagittal curve profiles, may allow a more complete and thorough understanding of alignment adaptations. Understanding the direction and quantum of these changes is an area of active research.
Sagittal alignment in non-fusion surgery
Motion preservation surgery in the cervical spine includes both anterior and posterior varieties, with choice of approach dependent greatly on the specific spine pathology being addressed. While artificial discs may have a theoretical advantage in sagittal realignment, the literature supporting this is not strong. Endoscopic cervical procedures have become popular over the last decade but their impact on cervical spine alignment is still unknown. Non-fusion posterior surgeries are known to be kyphosing procedures, with laminoplasties and laminectomies often (60) resulting in incrementally more loss of lordosis compared with laminectomy and fusion. This may again be related to disruption of the posterior tension band effect of the spine, resulting in accelerated kyphosis due to the drive to assume an energy-conserving posture (15). The clinical impact of this radiological finding is controversial. Kaptain et al. (61) reported an incidence of post-laminectomy kyphosis of up to 21%, with no effect on clinical outcome at a mean of four years follow up. Lee at al. (62) similarly showed the kyphosing effect of cervical laminoplasty, with 70% of their 50 patients with ossified posterior longitudinal ligaments having global C2-C7 kyphosis post-operatively. No correlation to improvements in mJOA, visual analogue score (VAS) or patient-reported outcomes (SF-36 or NDI) however, were found at a mean follow up of 18.4 months. Chiba et al. (63) followed 80 patients who underwent cervical laminoplasties up to a mean of 14 years post-operatively, and found that while only 52% of them maintained lordotic alignments at final follow up, these did not translate to worse clinical outcomes or neurological deterioration. These reports suggest that radiological findings of post-surgical kyphosis may not have a large impact on patient outcomes.
Contrary to this, Suda et al. (64) found in their series of 114 patients undergoing laminoplasty that local and global post-operative kyphosis correlated with poorer recovery rates in mJOA. They recommended that patients with local kyphotic segment values exceeding 13° should undergo simultaneous alignment correction. They found also that increasing axial neck pain was seen with progressively more destabilising procedures, laminectomy and fusion followed by laminoplasty followed by laminectomy alone. Moreover, the higher degree of kyphosis seen in the group who underwent laminectomy alone was thought to contribute to reduced mJOA recovery rate compared to the other two subgroups. These findings were supported by Miyamoto et al. (65) who found that patients with pre-operative local kyphosis had worse rates of neurological recovery with laminoplasty alone without correction of sagittal alignment. There was no significant difference in neurological outcomes between the lordotic patients undergoing laminoplasty and kyphotic patients who had simultaneous sagittal alignment correction, suggesting a benefit in surgically reducing local segmental kyphosis when possible.
Several factors are known to predict the development of either immediate or delayed post-operative kyphosis including T1-slope (66) and greater degrees of pre-operative sagittal imbalance (67), however there has yet to be any consistent evidence linking these to clinically worse outcomes.
Conclusions
Cervical sagittal balance is undoubtedly a vital concept that must be considered with surgery to the cervical spine. As it stands however, our understanding of its exact role and impact is incomplete and primitive. Patients with pre-operative cervical kyphosis with sagittal imbalance are known to have worse outcomes post-operatively. It is unclear whether and to what extent correcting this imbalance should be pursued, as it must be shown to result in clinically superior outcomes. A greater understanding of its relationship with overall global spinal balance will also be required in order to accurately determine personalised surgical correction targets for individual patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Lee A. Tan and Ilyas S. Aleem) for the series “Advanced Techniques in Complex Cervical Spine Surgery” published in Journal of Spine Surgery. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: The series “Advanced Techniques in Complex Cervical Spine Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine 2005;30:2024-9. [Crossref] [PubMed]
- Canavese F, Turcot K, De Rosa V, et al. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur Spine J 2011;20:1141-8. [Crossref] [PubMed]
- Kuntz C 4th, Levin LS, Ondra SL, et al. Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine 2007;6:104-12. [Crossref] [PubMed]
- Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 2012;71:662-9. [Crossref] [PubMed]
- Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011;68:1309-16. [Crossref] [PubMed]
- Ling FP, Chevillotte T, Thompson W, et al. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur Spine J 2018;27:8-15. [Crossref] [PubMed]
- O’Brien MF, Kuklo TR, Blanke KM, et al. Spinal Deformity Study Group Radiographic Measurement Manual. 2008. Available online: https://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual.pdf. Accessed 14 September 2019 2019.
- Harrison DD, Troyanovich SJ, Harrison DE, et al. A normal sagittal spinal configuration: a desirable clinical outcome. J Manipulative Physiol Ther 1996;19:398-405. [PubMed]
- Takeshima T, Omokawa S, Takaoka T, et al. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine 2002;27:E348-55. [Crossref] [PubMed]
- Yu M, Zhao WK, Li M, et al. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur Spine J 2015;24:1265-73. [Crossref] [PubMed]
- Hey HWD, Lau ETC, Wong GC, et al. Cervical Alignment Variations in Different Postures and Predictors of Normal Cervical Kyphosis. Spine 2017;42:1614-21. [Crossref] [PubMed]
- Okada E, Matsumoto M, Ichihara D, et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur Spine J 2009;18:1644-51. [Crossref] [PubMed]
- Guo GM, Li J, Diao QX, et al. Cervical lordosis in asymptomatic individuals: a meta-analysis. J Orthop Surg Res 2018;13:147. [Crossref] [PubMed]
- Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine 1986;11:521-4. [Crossref] [PubMed]
- Hey HWD, Kimberly-Anne T, Chin BZ, et al. Comparison of whole body sagittal alignment during directed vs natural, relaxed standing postures in young, healthy adults. Spine J 2019;19:1832-9. [Crossref] [PubMed]
- Matsumoto M, Fujimura Y, Suzuki N, et al. Cervical curvature in acute whiplash injuries: prospective comparative study with asymptomatic subjects. Injury 1998;29:775-8. [Crossref] [PubMed]
- Harrison DD, Harrison DE, Janik TJ, et al. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 2004;29:2485-92. [Crossref] [PubMed]
- Katsuura A, Hukuda S, Saruhashi Y, et al. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 2001;10:320-4. [Crossref] [PubMed]
- Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine 2016;41:371-7. [Crossref] [PubMed]
- Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine 2013;38:S161-70. [Crossref] [PubMed]
- Mohanty C, Massicotte EM, Fehlings MG, et al. Association of preoperative cervical spine alignment with spinal cord magnetic resonance imaging hyperintensity and myelopathy severity: analysis of a series of 124 cases. Spine 2015;40:11-6. [Crossref] [PubMed]
- Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83. [Crossref] [PubMed]
- Song K, Su X, Zhang Y, et al. Optimal chin-brow vertical angle for sagittal visual fields in ankylosing spondylitis kyphosis. Eur Spine J 2016;25:2596-604. [Crossref] [PubMed]
- Suk KS, Kim KT, Lee SH, et al. Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine 2003;28:2001-5. [Crossref] [PubMed]
- Simmons ED, DiStefano RJ, Zheng Y, et al. Thirty-six years experience of cervical extension osteotomy in ankylosing spondylitis: techniques and outcomes. Spine 2006;31:3006-12. [Crossref] [PubMed]
- Etame AB, Wang AC, Than KD, et al. Outcomes after surgery for cervical spine deformity: review of the literature. Neurosurg Focus 2010;28:E14. [Crossref] [PubMed]
- Lafage R, Challier V, Liabaud B, et al. Natural head posture in the setting of sagittal spinal deformity: validation of chin-brow vertical angle, slope of line of sight, and McGregor's slope with health-related quality of life. Neurosurgery 2016;79:108-15. [Crossref] [PubMed]
- Diebo BG, Challier V, Henry JK, et al. Predicting cervical alignment required to maintain horizontal gaze based on global spinal alignment. Spine 2016;41:1795. [Crossref] [PubMed]
- Moses MJ, Tishelman JC, Zhou PL, et al. McGregor's Slope and Slope of Line of Sight: Two Surrogate Markers for Chin-Brow Vertical Angle in the Setting of Cervical Spine Pathology. Spine J 2019;19:1512-7. [Crossref] [PubMed]
- Hey HWD, Tan KA, Ho VCL, et al. Radiologically defining horizontal gaze using EOS imaging-a prospective study of healthy subjects and a retrospective audit. Spine J 2018;18:954-61. [Crossref] [PubMed]
- Lee SH, Son ES, Seo EM, et al. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 2015;15:705-12. [Crossref] [PubMed]
- Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 2010;10:994-8. [Crossref] [PubMed]
- Hardacker JW, Shuford RF, Capicotto PN, et al. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 1997;22:1472-80. [Crossref] [PubMed]
- Hilibrand AS, Tannenbaum DA, Graziano GP, et al. The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop 1995;15:627-32. [Crossref] [PubMed]
- Hey HWD, Teo AQA, Tan KA, et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J 2017;17:799-806. [Crossref] [PubMed]
- Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 2006;15:415-22. [Crossref] [PubMed]
- Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 2005;87:260-7. [Crossref] [PubMed]
- Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: biomechanical approach. Eur Spine J 2011;20:578. [Crossref] [PubMed]
- Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. Journal of Neurosurgery: Spine 2013;19:141-59. [Crossref] [PubMed]
- Hansen MA, Kim HJ, Van Alstyne EM, et al. Does postsurgical cervical deformity affect the risk of cervical adjacent segment pathology? A systematic review. Spine 2012;37:S75-84. [Crossref] [PubMed]
- Patwardhan AG, Khayatzadeh S, Havey RM, et al. Cervical sagittal balance: a biomechanical perspective can help clinical practice. Eur Spine J 2018;27:25-38. [Crossref] [PubMed]
- Passias PG, Vasquez-Montes D, Poorman GW, et al. Predictive model for distal junctional kyphosis after cervical deformity surgery. Spine J 2018;18:2187-94. [Crossref] [PubMed]
- Kawakami M, Tamaki T, Yoshida M, et al. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord 1999;12:50-6. [Crossref] [PubMed]
- Kwon B, Kim DH, Marvin A, et al. Outcomes following anterior cervical discectomy and fusion: the role of interbody disc height, angulation, and spinous process distance. J Spinal Disord Tech 2005;18:304-8. [Crossref] [PubMed]
- Roguski M, Benzel EC, Curran JN, et al. Postoperative cervical sagittal imbalance negatively affects outcomes following surgery for cervical spondylotic myelopathy. Spine 2014;39:2070. [Crossref] [PubMed]
- Cabraja M, Abbushi A, Koeppen D, et al. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurg Focus 2010;28:E15. [Crossref] [PubMed]
- Lawrence BD, Jacobs WB, Norvell DC, et al. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: a systematic review. Spine 2013;38:S173-82. [Crossref] [PubMed]
- Luo J, Cao K, Huang S, et al. Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J 2015;24:1621-30. [Crossref] [PubMed]
- Fehlings MG, Barry S, Kopjar B, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine 2013;38:2247-52. [Crossref] [PubMed]
- Audat ZA, Fawareh MD, Radydeh AM, et al. Anterior versus posterior approach to treat cervical spondylotic myelopathy, clinical and radiological results with long period of follow-up. SAGE Open Med 2018;6:2050312118766199. [Crossref] [PubMed]
- Shamji MF, Mohanty C, Massicotte EM, et al. The association of cervical spine alignment with neurologic recovery in a prospective cohort of patients with surgical myelopathy: analysis of a series of 124 cases. World Neurosurg 2016;86:112-9. [Crossref] [PubMed]
- Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 2014;23:552-9. [Crossref] [PubMed]
- Smith JS, Shaffrey CI, Lafage V, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy: Presented at the 2012 Joint Spine Section Meeting. J Neurosurg Spine 2012;17:300-7. [Crossref] [PubMed]
- Blondel B, Schwab F, Bess S, et al. Posterior global malalignment after osteotomy for sagittal plane deformity: it happens and here is why. Spine 2013;38:E394-401. [Crossref] [PubMed]
- Jalai CM, Passias PG, Lafage V, et al. A comparative analysis of the prevalence and characteristics of cervical malalignment in adults presenting with thoracolumbar spine deformity based on variations in treatment approach over 2 years. Eur Spine J 2016;25:2423-32. [Crossref] [PubMed]
- Scheer JK, Passias PG, Sorocean AM, et al. Association between preoperative cervical sagittal deformity and inferior outcomes at 2-year follow-up in patients with adult thoracolumbar deformity: analysis of 182 patients: Presented at the 2015 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves. J Neurosurg Spine 2016;24:108-15. [Crossref] [PubMed]
- Lee DH, Ha JK, Chung JH, et al. A retrospective study to reveal the effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic sagittal alignment. Eur Spine J 2016;25:2286-93. [Crossref] [PubMed]
- Hwang SW, Samdani AF, Tantorski M, et al. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine 2011;15:491-6. [Crossref] [PubMed]
- Pepke W, Almansour H, Lafage R, et al. Cervical spine alignment following surgery for adolescent idiopathic scoliosis (AIS): a pre-to-post analysis of 81 patients. BMC Surg 2019;19:7. [Crossref] [PubMed]
- Du W, Wang L, Shen Y, et al. Long-term impacts of different posterior operations on curvature, neurological recovery and axial symptoms for multilevel cervical degenerative myelopathy. Eur Spine J 2013;22:1594-602. [Crossref] [PubMed]
- Kaptain GJ, Simmons NE, Replogle RE, et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg 2000;93:199-204. [Crossref] [PubMed]
- Lee CK, Shin DA, Yi S, et al. Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine 2016;24:100-7. [Crossref] [PubMed]
- Chiba K, Ogawa Y, Ishii K, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine 2006;31:2998-3005. [Crossref] [PubMed]
- Suda K, Abumi K, Ito M, et al. Local kyphosis reduces surgical outcomes of expansive open-door laminoplasty for cervical spondylotic myelopathy. Spine 2003;28:1258-62. [Crossref] [PubMed]
- Miyamoto H, Maeno K, Uno K, et al. Outcomes of surgical intervention for cervical spondylotic myelopathy accompanying local kyphosis (comparison between laminoplasty alone and posterior reconstruction surgery using the screw-rod system). Eur Spine J 2014;23:341-6. [Crossref] [PubMed]
- Kim TH, Lee SY, Kim YC, et al. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine 2013;38:E992-7. [Crossref] [PubMed]
- Sakai K, Yoshii T, Hirai T, et al. Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Spine 2016;41:299-305. [Crossref] [PubMed]