
Technology advancements in spinal endoscopy for staged management of painful spine conditions
The history
The development of endoscopy, in general, reflects the medical history of the last 200 years in an extraordinary way. It is so extraordinary because endoscopy expanded into almost all fields of medicine, including ENT, urology, gynecology, orthopedics, and neurosurgery. Success in these subspecialties inspired the development of new fields of operative techniques and clinical subspecialties. Modern endoscopy incorporates many technical innovations that initially were not developed for medical purpose but stemmed from military developments or consumer products. The desire to look inside the human body cavities, to establish a diagnosis and to treat disease is at least 6,000 years old. However, the first product of an endoscopic diagnostics system consisting a light source, optics, and a housing assembly was the brainchild of the Frankfurter physician Philipp Bozzini, who also developed specula shaped instruments to create access to a body cavity (1).
The crucial achievement of Philipp Bozzini was to divide the tube in half (2). This principle is valid until today. Through one channel, the light is directed to the object and then viewed through the other by the reflected image through a lens system. The Bozzini light guide was equipped with a lens, an eyepiece, and a candle serving as a light source. Due to the insufficient illumination by candlelight, the invention had nearly no practical value. With his idea, however, he inspired the following generations of engineers to continue development of endoscopy into its current state of the art. Additional developments and related inventions were driven by substantial knowledge gains in the fields of electricity, optics, and precision mechanics.
In 1973, Parvis Kambin introduced the concept of a transforaminal approach with the use of percutaneously placed Craig’s cannula’s through which he performed microdiscectomy in a non-visualized fashion (3-5). The introduction of a specially modified arthroscope into the intervertebral disc, and, thus, the first visualized microdiscectomy, was first reported by Forst and Hausman in 1983 (6). Coaxial endoscopes were developed because they offered the option to visualize and remove the painful pathology. The addition of a motorized shaver was described by Onik in 1985 which led to the coining of the term “Automated Percutaneous Nucleotomy” (7). Kambin published his first “discoscopic views” from within the disc in 1988 and later emphasized the importance of epidural visualization as well (8). One year later, Schreiber described the injection of indigo carmine dye into the disc to stain abnormal nucleus pulposus and annular fissures (9). Kambin also first described the “safe” or “working” zone in 1990 as the triangle bordered by the exiting nerve root, the inferior endplate and the superior articular process of the inferior vertebra, and medially by the traversing nerve root (10).
The paradigm shift
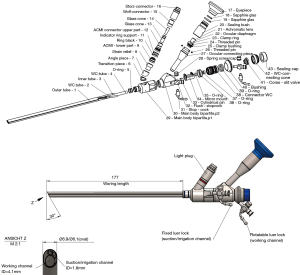
With the development of miniature cameras (1980) such as the tube color camera (Lemke/Storz), the operating area was no longer viewed directly through the endoscope but on a monitor (11,12). This changed both the handling of endoscopes and the ergonomic and organizational processes of endoscopic examinations and treatments. The first minimally invasive procedures using a visualization system were performed laparoscopically. Professor Kurt Semm developed insufflators, surgical instruments, and pelvic trainers for many years. The connection with a miniature camera system provided all the components that formed the basis for minimally invasive procedures (13). At first controversial, the minimally invasive endoscopic surgery conquered almost all medical subspecialities within a few years. Nowadays, it is an integral part of routine diagnostic and therapeutic protocols in spinal surgery as well. In 1967, when no more than 1% of all medical procedures were performed with the help of an endoscope, currently, more than 50% are employing an endoscope worldwide. Companies, such as Karl Storz or Richard Wolf, Smith and Nephew, Stryker and Olympus, who have recognized this trend early. Now, new OEM companies are joining in, and continue as prolific innovators. An example of the senior authors preferred OEM spinal endoscope is shown in Figure 1. It combines ergonomic advantage with good image reproduction and durability in routine use in frequent sterilization cycles at the senior authors surgery center.

Illumination problems in early spinal endoscopes
The ability to illuminate cavities inside the human body was the first significant milestone in the history of endoscopy. The use of a platinum glow wire at the tip of an endoscope is attributed to many inventors. Max Nitze and the instrument maker Josef Leiter developed a useful instrument in 1879 and published the application and results worldwide (2). In 1887, the platinum glow wire was replaced by a miniaturized light bulb developed by Alva Edison. Josef Leiter was awarded the first patent for an endoscope following the standards of high-quality design and inventive level. In 1906, Prof. Dr. Ringleb, the Zeiss physicist von Rohr and Georg Wolf, significantly improved the optical system by calculating the glass path and lenses as well as the use of the Amici prism (2). Prof. Dr. Ringleb contributed the geometric data for the mechanics, which Georg Wolf transformed into a product that set the quality standard for the next 60 years (1).
In the early 1990ies, multichannel endoscopes with optics, illumination, a working channel, and flushing function appeared on the market. Yeung designed the first usable multichannel endoscope in cooperation with Wolf. Other products were simultaneously developed by Schreiber and Leu (Zurich) (9) in cooperation withKarl Storz Endoskopie, Tuttlingen, and by Hal Matthews, who introduced the first fiber-optics endoscope in cooperation with Danek Inc., Memphis (14). Since the endoscope was directed via the posterolateral approach into the lumbar neuroforamen, the surgical technique was called “Foraminoscopy”. The Danek foraminoscope was produced by Citation Medical Corp., Reno NV, and was introduced for the first time at the Laser Conference 1991 by Hal Matthews in San Francisco. Danek, Inc. held 10% Shares and had a world-wide exclusive licensing agreement. The Danek foraminoscope used fiber bundles for image transmission and therefore offered only a viewing angle of 0°. The working length was 210 mm with a 3.5 mm Ø inner working channel which allowed the use of instruments up to that size. The outer Ø was 6.5 mm. The concept behind this design was to use the Danek foraminoscope for median and paramedian herniations intraforaminal herniations. Unfortunately, this concept design failed for several reasons. In most cases, the foraminoscope did not fit through the foramen, and the 0° optic was not suitable for visualization of herniations located in the central canal. Moreover, the fiber optical system delivered a poor image quality and the single-use endoscope raised the case cost above reimbursement level for the procedure. Subsequently, the product was removed from the market in 1994.
Illumination and lens diameter, however, traditionally has been the limiting factor dictating design constraints for spinal endoscopes as a minimum diameter for the lens was required to transport the image of the intraspinal anatomy to perform surgery adequately. Hence, the size of the working and irrigation channels in some designs had to be reduced to accommodate an appropriate lens system. Newer designs employing advanced illumination technologies have overcome these problems in part. Advances in the spinal endoscopy platform demanded by expert surgeons who are attempting to perform more complex endoscopic decompression and reconstructive surgeries will likely continue to push the limits of contemporary design constraints and stimulate the quest for workarounds based on new technologies.
Advanced optics & next generation spinal endoscopes
At the end of the 50ies, the physicist Harald H. Hopkins developed rod lenses for endoscopy, which were based on the inversion principle. The proportion of glass in the endoscope was increased significantly, and the air chambers were substantially reduced. The result was a higher contrast, and a brighter and sharper image. Only Karl Storz recognized the meaning of the invention in the middle of 1960 and executed an exclusive contract with H. H. Hopkins. Through the use of glass fibers and halogen lamps, Karl Storz redefined the illumination of body cavities under the name “cold-light source.” He was awarded numerous patents for his inventions. By rod lenses and cold light source, the quality of the intracorporeal observation of body cavities reached new quality standard that were previously considered impossible (15).
The Leu foraminoscope was designed for treatment of foraminal and extraforaminal herniations. It was produced by Karl Storz and its clinical use was demonstrated by Dr. Leu in 1991 (16). The Storz-built endoscope used a Hopkins rod lens system with a 6° viewing angle which was acceptable for the chosen indications. The working length was 145 mm and the inner working channel allowed the use of instruments up to 3.0 mm in diameter. It had several advantages with a brilliant image, and ample number of instruments required to do the endoscopic discectomy surgery. It could be sterilized and therefore was suitable multi-use. Not needing disposable endoscopes lowered the case cost during routine clinical operation significantly. Moreover, large capital purchases for proprietary videoendoscopic tower equipment were not necessary since the Leu-designed and Storz produced foraminoscope easily connected to existing Video Towers. The foraminoscope designed by Hans-Jörg Leu was offered by Karl Storz until 2012 when it was replaced by more contemporary products after a 21-year run.
Endoscopes with a wider optical viewing angle were introduced by Schreiber in 1989 allowing dorsal vision around an annular tear (9). Kambin and Zhou demonstrated the use of a 30-degree endoscope recognizing that lateral recess stenosis can hamper the effectiveness of the procedure (17). Foley (18), Mathews (14), and Ditsworth (19) furthered the field of endoscopic spinal surgery by popularizing the transforaminal approach in their clinical studies published between 1998 and 1999. In 1997, Yeung introduced The Yeung Endoscopic Spine System (YESS) using a multichannel, wide-angled endoscope produced by Richard Wolf (20). The System consisted of a multi-channel, oval-shaped endoscope with a 207 mm working channel of 2.7 mm Ø for use of 2.5 mm surgical instruments, an irrigation channel, and a rod lens. It was designed for intradiscal decompression for protrusions, for foraminal and extraforaminal herniations and for foraminoplasty with lasers and radiofrequency. The YESS system set itself apart from its competitor’s systems as a leap forward in quality with excellent visualization consisting of high-quality optics, camera, cold light projector and monitor (21).
Endoscopy as minimally invasive spine surgery
At the beginning of the 1900s, physicians tried to create artificial access to body cavities in addition to the natural entry ways to body cavities in several subspecialties, including ENT, gynecology, urology, and thoracic surgery. Laparoscopy is an examples of this development. In the 1970ies, the introduction of chip technology enabled the production of miniature camera systems and electronic CO2 insufflation and flushing devices. From 1962 and onward, Kurt Semm, a physician and engineer, developed CO2-insufflation devices and surgical instruments that were capable of performing laparoscopic surgery. Norbert Lemke produced cameras for Prof. Wolfgang Mauermeyer since the early 1970s (1). In conjunction with endoscopes, these cameras enabled the video transfer of live surgeries to seminar rooms (11). Karl Storz recognized at an early stage the potential of the development of video visualization systems, consisting of an endoscope, cold light source, miniaturized color camera, video monitor, and a recording system. An exclusive contract between Storz and Lemke was signed in 1980. The first mobile video towers were created, consisting of these components (11).
In 1992, Dr. Thomas Hoogland was one of few surgeons, who bought the Danek System when its European headquarter was established in Germany. He quickly realized that the Danek foraminoscope had significant shortcomings and was unsuitable to treat intracanal, foraminal, extraforaminal herniations, and herniations with free fragments in lumbar spine. In 1994, he concluded that a foraminoplasty was necessary to treat the variety of disc herniations frequently encountered in clinical practice. He went on to develop a system of reamers, and drills which was deployable over special guidance system, called “Tom Shidi”. This system was produced in 1994 by an OEM manufacturer according to Hoogland’s exact dimensions. At the time, he had the experience of several thousand of minimally invasive spine surgeries. But none of the endoscopes commercially available at the time were specifically produced for removal of herniated disc. It required to break away from traditional time-proven concepts from neurosurgical and urological product lines. New optical designs based on unproven calculations were required. Eventually, Hoogland also found and a manufacturer capable of producing a foraminoscope allowing him reach intracanal herniations by a target-oriented approach which is also known as the outside-in technique (22).
In 1998 Dr. Hoogland found a German OEM producer who was willing to invest in a new endoscope design. The OEM calculated the rod lens optical system thoroughly and developed also all mechanical parts specially for this purpose. The result was a multichannel endoscope with a length of 180 mm, a working channel of Ø 3.6 mm for instruments up to Ø 3.5 mm, an irrigation channel, a fiber glass illumination system with 0° and 30° optic variants, and an outer diameter of 6.3 mm. The OEM was able to realize these specifications by the use of 1.9 mm Ø rod-lens system without having to compromise on image quality. To date, this OEM offers still the widest range of coaxial endoscopes with working channel in many different lengths, diameters of the working channel and outer diameter. In 2001, Dr. Hoogland became the co-founder of joimax®. At the time, he brought his wealth of clinical knowledge of some 5,000 endoscopic surgeries during the development of the THESSYS method to the table. THESSYS is still used by many spine surgeons around the world. In 2004, Hoogland separated from joimax® and founded his own company maxmore® Hoogland Spine Products Inc in 2006. In 2001, Knight et al. showed that endoscopic foraminoplasty with a side-firing Ho: YAG laser can be useful in neural element decompression (23). The advent of lasers also stimulated electrothermal annuloplasty for low back pain which was also described by Tsou and Yeung in 2002 (24). Soon thereafter, more contemporary systems were introduced by Antony Yeung in 2003 with new custom instruments and cannula configurations following the lauch of the Yeung Endoscopic Spine System (YESS™) in 1998, which was designed around the transforaminal endoscopic approach for intradiscal and epiduroscopic procedures (25).
Image quality drives clinical protocols
Image quality in endoscopy is perceived by magnification, depth of field, resolution, color truth, and high image contrast as well as low distortion and homogeneous illumination up to the edge of the image. The image quality is visible to the viewer on the screen. The direct view through the endoscope is only rarely used. The image is transported from its place of origin inside the human body over a large number of individual components to the screen. Only if all individual parts of the visualization system are perfectly coordinated with each other, a high-quality image is produced. With the introduction of HD flat screens and HD video cameras starting 2005 and direct marketing to consumers, even the layman was able to detect a significant improvement in image quality. The endoscope manufacturers were essentially forced by the appearance of this invention on the consumer market to develop endoscopes that provided optimized image quality for the HD Video chain. Some of these technological advancements in the 2000 coincided with introduction of endoscope into transforaminal spinal surgery. Future advances in clinical protocols will likely be driven by higher image quality standards that may provide the basis for artificial intelligence applications in image recognition, robotics, integration and automatization of surgical processes.
Rigid endoscopes as the backbone of modern spine surgery
At the distal end of the spinal endoscope is the lens. The image that a lens produces from an object is a so-called real image. From the lens, the image must be transported to the other end, to the eyepiece. The installation of rod lenses does this. Rod lenses are glass rods with optically processed ends, the spaces between the rod lenses are referred to as air lenses. Each rod lens generates an intermediate image that creates another intermediate image from the air lens and the next rod lens. According to the desired length of an endoscope as many rod lenses must be used until the image plane of the eyepiece is reached to allow viewing or forwarding of the image to the camera. The quality of the optical system depends on the type of glass selected for the rod lens. The calculation of the glass path, which is the path the light beam travels from the lens to the eyepiece and is worked out by a physicist (7). The glass surface of the rod lens is typically tempered. By refraction of the light in a converging lens, the propagation direction changes. Due to the calculated surface shape of the lens, the incident light rays are collected at the focal point and thus produce an intermediate image.
While this rod-lens design is time-proven for simple discectomies, newer designs of spinal endoscopes will likely address some of the common problems encountered during contemporary spinal stenosis decompression- and reconstructive fusion procedures. For example, the lens is near the surgical decompression area in the spine and is subject to abuse not only by surgical instruments, including power burs but also to the thermal stress of repetitive sterilization cycles. Failure of the lens seal resulting in leakage is a common mode of failure in spinal endoscopes with acute image deterioration during surgery. Technology advancements in that area by replacing epoxy-based glues with gold soldering have improved the durability of spinal endoscopes substantially. Another problem arises from the use of glass rod lenses. Modern power drills, burs, and aggressive decompression tools including chisels, and large rongeurs may put the structural integrity of the glass rod system at risk due to vibration or hammering when these instruments are employed through the inner working channel of the spinal endoscope. Common failure modes include scratching of the lens or breakage of the rod lenses or failure of the seal between them. Several manufacturers have now endoscopes on the market with large irrigation and working channels to accommodate these motorized instruments and to effectively remove the debris they create from the surgical site. Surgeons who are expanding clinical indications to replace traditional translaminar surgeries with further miniaturized versions of them are the impetus for implementing technology advances into the build of a spinal endoscope which requires better illumination and image quality. While such support infrastructure advances may be fueled by technology transfers from the space-, military- or consumer sector developments in the area of illumination, image quality, and high-definition video quality, development of more and stress-resistant spinal endoscopes capable of carrying out the endoscopic spine surgeries of the future will likely hinge on continued expert surgeon input.
Aberrations & image quality
Spinal endoscopes suffer from limitations inherent to any optical system. When transporting the image over several lens systems, aberrations occur. The aberrations can be detected in the context of a geometric optics (4,5). They can be divided into four groups:
- Image sharpness error (spherical aberration, astigmatism, field curvature, coma);
- Image scale error (distortion);
- Chromatic aberration;
- Image illumination error (vignetting, scattered light, and reflections).
To deal with these types of aberrations, one needs to consider how a beam emanating from a particular object point behaves after passing through the lens system. Ideally, the rays intersect at one point. Due to the aberrations, there is instead a narrow constriction of the beam, which may also be in the wrong place (distortion or field curvature). In the case of aberrations, the beam behaves indifferently. For example, in spherical aberration, the rays do not meet in one point, which leads to blurring. Astigmatism, on the other hand, occurs when objects are outside the optical axis and, hence, are blurred. The cause is the different focal lengths. The coma arises when light enters the system obliquely to the optical axis beam. Aplanatic lenses correct both the spherical aberration and the coma. If an image is created on a curved surface instead of a flat surface, field curvature is created. Image sharpness decreases towards the edge. Additional aberrations may arise from chromatic aberrations resulting in color errors. The refractive index of optical glass depends on the wavelength of the incident light. This phenomenon is called dispersion. It is the cause of the chromatic aberration. The Gaussian error occurs when colors spread at different speeds depending on the frequency of the light and split at optical interfaces. The dependence of a physical parameter on the frequency of a wave is the definition of dispersion. Such decomposition of white light into its spectral colors occurs as it passes through a prism, where the light rays diverge outward. The dispersion of the optical lenses causes a variation of the remaining aberrations with the wavelength. Correcting for these aberrations is of critical importance when attempting to construct a high-quality spinal endoscope. Aberrations are corrected in endoscopy by combining different types of glass and partially using aspherical surfaces. It is obvious that this a cost factor and determines the overall quality and longevity of the spinal endoscope in routine clinical use where endoscopes should be usable for 200 to 250 sterilization cycles (surgeries).
The mechanics of spinal endoscopy
A modern spinal endoscope consists of a large number of mechanical parts such as the cladding tube, the body, spacers, fixation screws, snap rings and many other items—all in all approximately 150 parts. These mechanical parts assemble the optical system in a way that prevents shifting of the optical components. A shift in these components would result in a significant reduction in image quality and negate the benefits of optical enhancements to HD quality. These mechanical parts have to be designed, manufactured with the highest possible precision, and assembled and adjusted by long-term experienced technicians (26). The effort required and the impact on the overall quality of an endoscope are often underestimated. An example of a mechanical parts of high-end modern spinal endoscope is shown in Figure 2. The use of CNC multi-axis machines enables the production of high-precision mechanical parts, even in the micro range. The high-resolution, high-contrast color reproduction and sharpness display screen have prompted manufacturers of endoscopes and visualization systems to optimize all components such as endoscope, camera, processor, and display for HD image quality. The improved detail recognition, the greater depth of focus, and color truth help to assess images more accurately, which will likely form the basis for integration of artificial intelligence and robotics in endoscopic spine surgery. The use of CNC-Machines also had a significant influence on the production of precise surgical instruments. Richard Wolf offered the opportunity to produce surgical instruments of the highest standard and developed with Anthony Yeung the YESS™—instrumentation. The design of the working cannula was tricky because the end was shaped in a slope, so the nerve and exiting root could be retracted and protected. Because of all the indications Anthony Yeung had in mind, he designed a wide range of instruments which he showcased routinely during IITTS training courses at his Phoenix Squaw Peak Surgical Facility through a mentorship program.
Optimized spinal endoscopes
Extra-low-dispersion glass (ED glass) produces remarkably sharp, high-contrast images. ED glass is a fluoride-rich glass melt (FL glass) from which apochromatically corrected lenses are manufactured. ED glass can focus the entire color spectrum more precisely and almost eliminates the color fringing caused by chromatic aberration. Barrel and pillow-shaped distortions are avoided.
An objective lens consists of several individual lenses. For a lateral viewing angle, a prism is used, this is not necessary at 0° viewing direction. Additional components consist of distal end glass (sapphire glass), entrance pupil, aperture, and the objective lens. In the camera lens area, the focal length and the depth of field are determined. The aperture influences the image brightness. All individual components influence each other and lead to aberrations. The optimized production of rod lenses is based on physical calculation, testing with the latest measuring equipment and production on the latest production machines. Also necessary are the adhesives used and the surface finish used. An eyepiece consists of a lens system, which is coupled via a PEEK ring to the camera head. The PEEK ring prevents the ingress of stray light. An eyepiece consists of field diaphragm, lenses, filter thread, and socket. Due to the different arrangement of lenses, there are a variety of eyepiece types. The characteristics of an eyepiece are defined by focal length, exit pupil, and field of view (Figure 1). The same rules apply to HD optimization as to rod lenses.
The image quality of an endoscope can be optimized by measuring the following parameters: the intensity of the optical fibers, light intensity, and quality of the lens system, color truth, sharpness and focus, viewing angle, the field of view (visible surface). For a detailed evaluation of an optical system, it is not enough, only to consider individual aberrations. To adequately describe the performance of the optics, consideration of the modulation transfer function is essential. Excellent image quality is characterized by the fact that individual delicate structures are reproduced not only separately (resolution), but also with a sufficient difference between light and dark (contrast).
Full HD playback
For the HD optimization of the endoscopic image during spinal endoscopy, light generation and transmission to the spinal anatomy is crucial. Xenon light sources with 300 watts or light sources with LED and laser light technology achieve the best possible illumination for full HD image reproduction. A HD camera consists of camera head and processor (CPU). The clamping ring at the proximal end of the camera head establishes the connection between the eyepiece and the camera sensor. The optical image is converted into electrical signals. Behind it is the focus ring; it is used to focus the image. Once set, the zoom ring can be used to zoom the image without the need for refocusing (parfocal zoom). With the optical zoom, the high image quality is maintained because the image section is mechanically enlarged, and thus the high resolution is not changed. Digital zoom will extrapolate an image section, but details may be lost. C-MOS sensors have proven themselves for HD image transmission. C-MOS sensors convert the incident light into voltage. The conversion of the light is done by transistors, which are located directly on the pixel. Specific data such as photosensitivity, pixel number, readout speed, dynamic range, and chip size achieve outstanding values. The image noise is mostly suppressed.
HD screen
The surgeons are highly aware of the technology advancements introduced by industry into the consumer market since the ongoing improvements in high quality of flat panel displays has become affordable for home audio-video applications. The terms HD, Full HD, 4K, and 8K refer to the number of pixels that are spread across the screen and relate to the resolution. Current flat screens offer more than high sharpness and a clear picture. Behind a wealth of terms hide technological innovations that significantly affect the image quality. The earliest technology was offered as LCD (Liquid Chrystal Display). As liquid crystals only modulate the light but do not emit light themselves, the backlight is placed behind the display for televisions, whereby the image information is displayed in transmitted light. LED TV are televisions that use light-emitting diodes (LEDs) for backlighting. More appropriately, such devices may have been called “LED background Illuminated LCD TVs”. HDR stands for High Dynamic Range Image and denotes a high-contrast image. In principle, this technology approaches the eyesight of the human eye by using high bit values to achieve a large number of brightness levels. Image files are generated, which better capture natural brightness. HRD Video uses a color depth of 10 bits and thus achieves a high dynamic range. By adding three subpixels of the primary colors red, green and blue, colors appear in the television picture. Above all, HDR improves the appearance of saturated light colors and very dark colors. The HDR technique also avoids over- and under-exposure. OLED (organic light-emitting diode)—an organic light-emitting diode is a luminous thin-film component made of organic semiconducting materials. The difference to the LCD technology is that every single pixel itself shines. This results in a significant improvement of the image contrast because each pixel assumes arbitrary brightness levels and produces a much-improved color fidelity. OLED screens offer several advantages:
- OLED thin-film components are inexpensive to manufacture;
- OLEDs do not require backlighting as they emit light themselves;
- OLEDs can emit light in different colors, while LCDs require additional color filters;
- The energy consumption of OLED screens is lower;
- Shorter electro-optical response times.
The disadvantage of OLED technology is currently a much shorter life cycle. The OLED technology is subject to further improvements and may eventually find implementation in the spinal endoscopy infrastructure prompting surgeons to identify and validate new clinical protocols.
Information technology & integration
Modern information technology (IT) is the basis for advanced OR integration. First systems enabled recording and storage of still images and simple video sequences for electronic documentation. Another step up was the development of software programs for storing image data and video sequences with interfaces for hospital PACS systems (8). These systems, in combination, provide the foundation for the paperless electronic health records (EHR). With EHR, large amounts of data can be stored in a small space and while providing ready access to work stations over the healthcare organization. The purpose of the OR Integration concept is to bring together actions that can be optimized through electronic recording and control processes to enable faster action and safer operations (9). Software programs create an easy-to-use interface that enables sterile control of electronic devices through a touch screen, as well as the retrieval and storage of intraoperative data by the surgeon, assistant or nurse, and is also developed for specialized disciplines and common types of surgery. Complex workplaces, which contain all the equipment required for the intervention, are recorded, controlled and their use monitored by data management. Other data sources of intraoperative modalities such as Navigation, Endoscopy, C-arm, and CT are also connected via interfaces, and the image, text, and vital data are displayed on large monitors. The surgeon is key to creating integration OR systems that assist in the clinical problem solving.
Key future technologies
Nanotechnology is used in semiconductor and surface physics combined with chemical processes. Nanotechnology is also used in sub-areas of mechanical engineering and food production. Nanotechnology will likely reach significance in endoscopy by in coating processes. The coating of endoscope cavities, of endoscope lenses but also screens (nanotubes) is conceivable. Photonics describes the technical mastery and use of light in every form. Why photons play such a unique role in science and industry is due to the extraordinary properties of light that benefit humans. Photonics can be found in all critical areas of modern society and economy. Examples can be found in medicine, industrial production with laser systems or energy-efficient illumination with LEDs and OLEDs. Photonics offers excellent potential to deliver innovative solutions for the markets and challenges of tomorrow.
Artificial Intelligence (AI) will likely play a crucial role in the development of health technology, including endoscopy (10). If the current trend continues an increasing amount of healthcare data will be processed without the need for intervention or processing by clinical staff. The shortage of highly trained clinical personnel and increasing pressure for cost-cutting are additional drivers of this trend. AI could take over routine tasks that do not require the specific expertise of a professional (11). It may aid during delicate portions of the spinal endoscopy procedure. Examples imaged based recognition of anatomical structures or defining the three-dimensional extent of interventional or surgical procedures such as the bony decompression procedure. Additional benefits may play out in decreasing operative times, or improved quality assurance, and standardization. Very likely a combination of AI and robotics will appear in clinical applications in one form or another.
Conclusions
The spine surgeon users expect technological improvements of spinal endoscopes and their supporting video equipment to improve clinical outcomes and expand the indications for the procedure. Transfer of innovative key technologies from other industries and the consumer market will likely continue leading to improvements in the efficacy and safety of spinal endoscopy.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Reuter MA. Geschichte der Endoskopie: Handbuch und Atlas (German Edition) (German) Hardcover. Reuter M, Volume 1-4, 1998.
- Reuter MA. Geschichte der Endoskopie: Handbuch und Atlas (German Edition) (German) Hardcover. Reuter M, Volume 5-7, 1998.
- Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res 1986.37-43. [PubMed]
- Kambin P, Brager MD. Percutaneous posterolateral discectomy. Anatomy and mechanism. Clin Orthop Relat Res 1987.145-54. [PubMed]
- Kambin P, Schaffer JL. Percutaneous lumbar discectomy. Review of 100 patients and current practice. Clin Orthop Relat Res 1989.24-34. [Crossref] [PubMed]
- Forst R, Hausmann B. Nucleoscopy--a new examination technique. Arch Orthop Trauma Surg 1983;101:219-21. [Crossref] [PubMed]
- Onik G, Helms CA, Ginsberg L, et al. Percutaneous lumbar diskectomy using a new aspiration probe: porcine and cadaver model. Radiology 1985;155:251-2. [Crossref] [PubMed]
- Kambin P, Nixon JE, Chait A, et al. Annular protrusion: pathophysiology and roentgenographic appearance. Spine (Phila Pa 1976) 1988;13:671-5. [Crossref] [PubMed]
- Schreiber A, Suezawa Y, Leu H. Does percutaneous nucleotomy with discoscopy replace conventional discectomy? Eight years of experience and results in treatment of herniated lumbar disc. Clin Orthop Relat Res 1989.35-42. [Crossref] [PubMed]
- Kambin P, Zhou L. History and current status of percutaneous arthroscopic disc surgery. Spine (Phila Pa 1976) 1996;21:57S-61S. [Crossref] [PubMed]
- Birkfellner W. Applied Medical Image Processing: A Basic Course. Second Edition ed. Vienna 2014.
- Diethelm V. Physik Mittelstufe: Optik, Magnetismus, Elektrizitätslehre, Atomphysik (Mentor Lernhilfen Physik) Taschenbuch. Langenscheidt Fachv; 1998.
- Kramme R. Medizintechnik. Verfahren - Systeme - Informationsverarbeitung: Springer Reference Technik 2017. Springer-Verlag Berlin Heidelberg, 2017.
- Mathews HH. Transforaminal endoscopic microdiscectomy. Neurosurg Clin N Am 1996;7:59-63. [Crossref] [PubMed]
- Pedrotti FL. Introduction to Optics. Pearson; 3rd ed.
- Leu HJ, Hauser R. Die perkutan posterolaterale Foraminoskopie: Prinzip, Technik und Erfahrungen seit 1991. Arthroskopie 1996;9:26-31.
- Kambin P, Zhou L. Arthroscopic discectomy of the lumbar spine. Clin Orthop Relat Res 1997.49-57. [Crossref] [PubMed]
- Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 1999;7:e5. [Crossref] [PubMed]
- Ditsworth DA. Endoscopic transforaminal lumbar discectomy and reconfiguration: a postero-lateral approach into the spinal canal. Surg Neurol 1998;49:588-97; discussion 597-8. [Crossref] [PubMed]
- Yeung AT. Minimally Invasive Disc Surgery with the Yeung Endoscopic Spine System (YESS). Surg Technol Int 1999;8:267-77. [PubMed]
- Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med 2000;67:327-32. [PubMed]
- Hoogland T, van den Brekel-Dijkstra K, Schubert M, et al. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation: a prospective, cohort evaluation of 262 consecutive cases. Spine (Phila Pa 1976) 2008;33:973-8. [Crossref] [PubMed]
- Knight MT, Goswami A, Patko JT. Cervical percutaneous laser disc decompression: preliminary results of an ongoing prospective outcome study. J Clin Laser Med Surg 2001;19:3-8. [Crossref] [PubMed]
- Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722-31. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Advances in endoscopic disc and spine surgery: foraminal approach. Surg Technol Int 2003;11:255-63. [PubMed]
- Krause W. Konstruktionsmerkmale der Feinmechanik. Werner Krause. 4th Edition ed.


