Surgical treatment of cervical radiculopathy using an anterior cervical endoscopic decompression
Introduction
Cervical radiculopathy (CR) is an inflammatory reaction of the nerve root. Although this neurological disorder is associated with mechanical compression due to reduced space in the nerve root canal (lateral cervical stenosis), recent studies showed that inflammatory cytokines from degenerated intervertebral disc also could be associated with CR symptoms (1,2). Therefore, treatments aimed at these inflammatory reactions inherent to the degenerative cervical disc disease process are potentially efficacious during the neuroforaminal decompression.
The foraminal narrowing can be caused by a herniated disc, presence of osteophytes (degeneration or microfractures of adjacent bony structures), or combination of both. Clinically, CR is characterized by arm pain, paresthesia, altered sensibility, and eventually, weakness (2). Radiating pain and its dermatomal distribution correspond to the affected level. Diagnosis of CR is based on the correlation of physical examination, plain film radiography, and advanced imaging such as MRI (2). However, consensus regarding definitive diagnostic criteria for CR does not exist (2). The clinical course of CR is generally favorable, and the first management option must be a conservative treatment for at least six weeks (1,3). The vast majority of patients (70–90%) responds to conservative care consistent in the use of patient education, analgesics, physiotherapy, short-term immobilization with a cervical collar, epidural steroid injections, and selective nerve blocks (1-3). In those patients who not respond to medical treatment, surgical treatment is indicated.
The objective of the surgical procedure is to decompress the cervical nerve roots and thus relieve pain. Surgical options include open anterior cervical discectomy and fusion (ACDF), cervical disc arthroplasty, and posterior foraminotomy (3). Although Robinson and Smith’s (4) anterior cervical technique for discectomy and fusion ACDF technique continues to be the most popular procedure for CR treatment, pseudarthrosis, and adjacent segments disease remain of concern (5). Intending to minimize those complications, there are several minimally invasive spine disc, preserving surgery options such as the endoscopic anterior and posterior approach (6-8).
The use of monosegmental anterior endoscopic discectomy to manage CR was described by Saringer (9) Choi (10-12) and Ruetten (13). This procedure consists of mechanical and thermal decompression of degenerated tissue compressing nerve structures in the foraminal area under an endoscope view from an anterior percutaneous approach and with the radiofrequency thermal energy. The surgical principle of the anterior cervical endoscopic discectomy (ACED) is the same as in open decompression (9). Endoscopic discectomy and foraminoplasty permits to expand the foraminal window, remove hypertrophic tissue and osteophytes to achieve a complete release of neural structures (14); and the thermal disc decompression and neurolysis theoretically evade the effects of the inflammatory cytokines from degenerated intervertebral disk (15). Another advantage of the ACED is that it can be performed without a fusion (13). ACED is a motion-preserving surgery (5). Moreover, it is an outpatient procedure and can be done with the use of local anesthesia and sedation (15). The purpose of this study is to report the outcomes and complication rates, of the use of ACED with a blunt approach, implemented in patients with CR.
Methods
Patients & selection criteria
A retrospective study was conducted on the clinical charts of patients whose reason for consultation was radiated cervical pain and with clinical signs of CR, and whom were surgically intervened with an ACED at one or two intervertebral disc segments.
Inclusion/exclusion criteria
The inclusion criteria were medical charts of patients with arm pain of more than six months of evolution with no response to conservative treatment, including injections, and MRI concordant with cervical lateral stenosis due to mono and multisegmental disc herniation, disc herniation with lateral soft fragments, and stenosis foraminal produced by osteophytes.
The study excluded medical charts of patients showing axial pain symptoms and imaging consistent with degenerative disc disease, loss of height greater than 50%, intervertebral space collapse, segmental instability, infection, uncontrollable disorders relating to coagulation disease and bleeding, anatomic alterations, severe neurological deficit, migrated hernia, progressive myelopathy, calcified disc protrusion, ossification of posterior longitudinal ligament, previous surgery at the same segment, impossibility to reach affected segment (patients with short neck or excessive obesity), and those medical charts without fully completed assessment criteria.
Surgical technique
The lightly sedated patient was placed in a supine position with cervical extension. The entire endoscopic ACED decompression was done in the awake patient. Adequate oxygenation was maintained via a nasal cannula. Cervical lordosis was accentuated by placing a pillow between the shoulders.
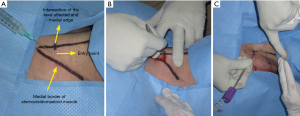
The best skin entry point to the surgical intervertebral disc level(s) was identified using biplanar fluoroscopy. An important anatomical landmark is the medial border of the sternocleidomastoid muscle as it intersects with the corresponding surgical level (Figure 1). To displace the esophagus and trachea medially and the neurovascular bundle including the carotid sheath laterally a surgeon’s finger is firmly pressed on the space between the muscle and the trachea—the tracheoesophageal groove. After local anesthetic infiltration, a 4 mm skin incision was made, and blunt dilators were advanced to the anterior annulus by turning them gently together. This eventually allowed placement of the working cannula at the anterior edge of the cervical annulus. A spinal needle was then advanced through the cannula up to the posterior third of the disc. This step is crucial to reach a blunt technique to avoid an undesirable puncture of a vascular structure (Figure 1).
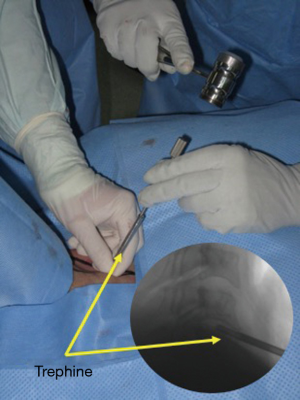
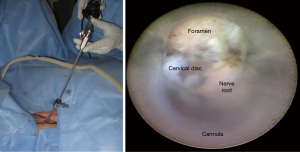
Once the spinal needle was adequately positioned within the posterior third of the surgical intervertebral cervical disc, chromo-discography and provocative discogenic were performed to confirm with the awake patient that the familiar pain generator was being treated. Then, a guidewire was advanced through the intradiscally placed the spinal needle. After removal of the spinal needle, the endoscopic dilators and the working cannula were repositioned, and their docking at the anterior annulus of the surgical cervical disc was verified under direct endoscopic visualization. The spinal endoscope was now advanced until it reached the foraminal area (Figure 2). In order to achieve a better visualization and improve dissection the first step was to remove the anterior cervical prevertebral fascia and to coagulate small vessels with the use of a bipolar radiofrequency probe (Trigger Flex DTF 40, Elliquence LLC, NY, USA). The last endoscopic dilator was then replaced with a trephine to gain access to the disc. The trephine was advanced with a rotating motion toward the disc in order to perform an annulotomy (Figure 3). Using the working channel of the endoscope, discectomy instruments, such as grasping forceps, were inserted to perform a mechanical discectomy. Finally, if necessary, osteophytes located in the foraminal window was endoscopically removed using shaver, burr or chisel. Complete decompression was then verified by directly visualizing the free cervical nerve root (Figure 2).
Clinical outcomes evaluation and statistical analysis
The clinical results were assessed by using two different primary outcome criteria: Macnab and visual analog scale for arm pain (VAS) (16). The pain intensity was measured by using the VAS, and patient satisfaction with the procedure was assessed with Macnab criteria (17). The follow-up was twelve months after the procedure. Data analysis was performed with the statistical software R 3.1.1 for Windows 8. Demographic parameters and descriptive statistics of the variables were established. The descriptive statistics was determined and the Wilcoxon test for related pairs was applied. The statistical significance was P<0.05.
Results
Demographic characteristics
From October 1997 to August 2018 a total of 293 patients were included in the study. There were 167 (57%) female and 126 (43%) male patients having a mean age of 55.9 years [standard deviation (SD) =11.8].
Surgical technique
The average surgical time was 65 minutes. The average blood loss was less than 30 mL. A total of 337 segments were intervened: 249 (85%) patients were intervened at one segment and 44 (15%) patients were treated at two segments. No patient was more than two segments treated. The average of segment per patient was 1.15 (SD =0.357). The most affected segment was C5–C6 (Table 1).
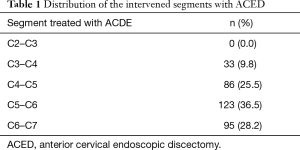
Full table
Clinical outcome
At 12 months follow-up with Macnab criteria 90.1% (n=264) of patients were rate to have had excellent and good outcomes, fair and poor outcomes were reported by 6.8% (n=20) and 3.1% (n=9) of patients, respectively. Finally, VAS score (1 no pain to 10 worst pain possible) on average was reported, preoperatively 7.8 and 2.2 post surgically. VAS was significantly decreased at the final follow-up (P<0.005)
Complications and reinterventions
During the experience we obtained a total of 8 (2.7%) patients with some complications: cervical hematoma: n=3 (Figure 4); carotid lesion: n=2; and transitory dysphonia n=3. The reintervention rate was 3.4% (n=10). No patients were intervened after the first years of the experience. The second surgical procedure was ACED in 3 patients and 7 with open conventional ACDF. The criteria to choose between ACED or ACDF as re-intervention option was the presence or not of some osteophyte or calcified hernia. In the cases with soft fragments were intervened with ACED.
Discussion
CR is a frequent complaint in the primary care setting worldwide (18). Radicular symptoms due to degenerative cervical spine changes are typically from soft disc herniation and osteophytes (19). The “gold standard” procedure is conventional open ACDF surgery (20). Minimally invasive techniques such as the ACED offer significant advantages over ACDF. These include smaller incisions and less tissue trauma, the outpatient nature of the ACED surgery, and conceivably a lesser risk of postoperative adjacent segment disease with instability while providing excellent clinical outcomes. Therefore, the minimally invasive ACED surgery as an excellent option to treat radiating arm pain secondary to CR (3-5,9-15).
In this series, we report on our clinical series of 293 patients treated for symptomatic CR with the ACED and foraminoplasty procedure—an extensive experience which spanned over nearly twenty years. Patients had statistically significant improvement of their average preoperative VAS for arm pain of 7.8 to a mean postoperative VAS score of 2.2; a total VAS reduction of 5.6. The vast majority of patients (90.1%) had Excellent and Good Macnab outcomes. These results are comparable to those previously reported by Ruetten et al. (13). Those authors compared an ACED to open surgery and found a complete resolution of symptoms in 88.5% of their patients. Also, Saringer et al. (9), reported on 16 patients with unilateral radiculopathy treated with anterior cervical endoscopic foraminotomy, with a similar follow-up of 13.8 months. They obtained an improvement rate above 96% and a high overall patient satisfaction of 87.6%. Fessler et al. (21) reported excellent and good resolution of symptoms in 92% of his patients in a series of 25 patients. A more recent study (5) including 210 patients reported an improvement of the VAS from preoperative 6.7 to postoperative 1.7 (5 points) with the procedure. In yet another study, Oh et al. (22) showed VAS improvements from preoperative 7.6 to postoperative 2.7 and successful Macnab outcome improvements with an overall patient satisfaction rate of 98%.
Our complication- and reoperation rates of 2.7% and 3.4%, respectively, were similar to those reported in the literature. Parihar et al. (5) reported a 1% of reintervention using ACDF; nevertheless, their rate of complications was 9%. These authors attributed it to the initial learning curve. Tzaan (23) reported a 1% of reintervention rate, but no complications.
A fundamental factor for the successful implementation of a novel surgical technique is appropriate and sufficient training. The learning curve of the procedure could be steep, and the outcomes are directly related to the surgeons’ skills. We recommended beginning performing first between 10 to 15 cases of a simplified, non-endoscopic fluoroscopy-based thermal cervical decompression (cervical thermodiscoplasty) before attempting ACED. While under supervision of an experienced proctoring surgeon, the apprentice surgeon should perform between 20–30 ACED cases before independently performing the endoscopic directly visualized technique. Also, we strongly suggest attending cadaver labs and workshops in well-recognized training centers.
Appropriate patient selection for the ACED procedure is of utmost importance. This team of authors have benefited from continuous retraining and practicing the ACED procedure in cadaveric specimens, mainly when technology advances are about to be implemented. The authors also recommend integration of ACED training into the core curriculum of surgical residency and fellowship spine training programs to prepare their graduates for what patients and payers alike demand of us—a less complicated, more cost-effective, and reliable solutions to treat CR.
Conclusions
Clinical outcomes obtained by the anterior endoscopic cervical technique in the treatment of stenosis are similar to open conventional techniques in terms of improvement and symptoms resolution. Endoscopic anterior approach outcomes are not significantly different from those reported with open or mini-open techniques. Because of the low complication rate and additional advantages of decreased length of stay, blood loss, postoperative pain, and narcotic utilization, as well as shorter operative times, it is clear that anterior cervical endoscopic decompression is an attractive alternative to open and other MIS techniques.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no direct (employment, stock ownership, grants, patents), or indirect conflicts of interest (honoraria, consultancies to sponsoring organizations, mutual fund ownership, paid expert testimony). The authors are not currently affiliated with or under any consulting agreement with any vendor that the clinical research data conclusion could directly enrich. This manuscript is not meant for or intended to endorse any products or push any other agenda other than to report clinical outcomes associated with ACED. The motive for compiling this clinically relevant information is by no means created and/or correlated to directly enrich anyone due to its publication. This publication was intended to substantiate contemporary endoscopic spinal surgery concepts to facilitate technology advancements.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. IRB approval was obtained for this study (CEIFUS 106-19). Written informed consent was obtained from the patient for publication of this Original Study and any accompanying images.
References
- Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech 2015;28:E251-9. [Crossref] [PubMed]
- Kjaer P, Kongsted A, Hartvigsen J, et al. National clinical guidelines for non-surgical treatment of patients with recent onset neck pain or cervical radiculopathy. Eur Spine J 2017;26:2242-57. [Crossref] [PubMed]
- Gebremariam L, Koes BW, Peul WC, et al. Evaluation of treatment effectiveness for the herniated cervical disc: A systematic review. Spine 2012;37:E109-18. [Crossref] [PubMed]
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 1958;40-A:607-24. [Crossref] [PubMed]
- Parihar VS, Yadav N, Ratre S, et al. Endoscopic anterior approach for cervical disc disease (disc preserving surgery). World Neurosurg 2018;115:e599-609. [Crossref] [PubMed]
- McAnany SJ, Kim JS, Overley SC, et al. A meta-analysis of cervical foraminotomy: Open versus minimally-invasive techniques. Spine J 2015;15:849-56. [Crossref] [PubMed]
- Wu PF, Liu BH, Wang B, et al. Complications of full-endoscopic versus microendoscopic foraminotomy for cervical radiculopathy: a systematic review and meta-analysis. World Neurosurg 2018;114:217-27. [Crossref] [PubMed]
- Yang JS, Chu L, Chen L, et al. Anterior or posterior approach of full-endoscopic cervical discectomy for cervical intervertebral disc herniation?: a comparative cohort study. Spine 2014;39:1743-50. [Crossref] [PubMed]
- Saringer WF, Reddy B, Nöbauer-Huhmann I, et al. Endoscopic anterior cervical foraminotomy for unilateral radiculopathy: anatomical morphometric analysis and preliminary clinical experience. J Neurosurg 2003;98:171-80. [PubMed]
- Choi G. Percutaneous endoscopic cervical discectomy: 16 years of experience and literature review. Coluna/Columna 2009;8:344-8. [Crossref]
- Choi G, Pophale CS, Patel B, et al. Endoscopic Spine Surgery. J Korean Neurosurg Soc 2017;60:485-97. Erratum in: J Korean Neurosurg Soc 2019;62:366. [Crossref] [PubMed]
- Joh JY, Choi G, Kong BJ, et al. Comparative study of neck pain in relation to increase of cervical epidural pressure during percutaneous endoscopic lumbar discectomy. Spine (Phila Pa 1976) 2009;34:2033-8. [Crossref] [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. Int Orthop 2009;33:1677-82. [Crossref] [PubMed]
- Dowling, A. Endoscopic anterior cervical discectomy. In: Lewandrowski KU, Lee SH, Iprenburg M. editors. Endoscopic Spinal Surgery. London: JP Medical, 2013:39-43.
- Ramírez JF, Rugeles JG, Ramírez C, et al. Anterior percutaneous cervical discectomy. Two-year follow-up of a blunt technique procedure. Coluna/Columna 2017;16:261-4. [Crossref]
- Huskisson EC, Jones J, Scott PJ. Application of visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976;15:185-7. [Crossref] [PubMed]
- Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]
- Quillo-Olvera J, Lin GX, Kim JS. Percutaneous endoscopic cervical discectomy: a technical review. Ann Transl Med 2018;6:100. [Crossref] [PubMed]
- Wan Q, Zhang D, Li S, et al. Posterior percutaneous full-endoscopic cervical discectomy under local anesthesia for cervical radiculopathy due to soft-disc herniation: a preliminary clinical study. J Neurosurg Spine 2018;29:351-7. [Crossref] [PubMed]
- Peng CWB, Yeo W, Tan SB. Percutaneous endoscopic discectomy: clinical results and how it affects the quality of life. J Spinal Disord Tech 2010;23:425-30. [Crossref] [PubMed]
- Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery 2002;51:S37-45. [Crossref] [PubMed]
- Oh HS, Hwang BW, Park SJ, et al. Percutaneous endoscopic cervical discectomy (pecd): an analysis of outcome, causes of reoperation. World Neurosurg 2017;102:583-92. [Crossref] [PubMed]
- Tzaan WC. Anterior percutaneous endoscopic cervical discectomy for cervical intervertebral disc herniation: outcome, complications, and technique. J Spinal Disord Tech 2011;24:421-31. [Crossref] [PubMed]