
Early return to activity after minimally invasive full endoscopic decompression surgery in medical doctors
Introduction
The full endoscopic surgery has gained significant traction in the last decade. The technique can be considered to be the evolution of Hijikata’s percutaneous method (1). Yeung et al. popularized the transforaminal approach (2-4). The advantage of the transforaminal approach in full endoscopic surgery lies in its minimal invasiveness utilizing a small 8 mm skin incision under the local anesthesia. When done in the sedate yet awake patient, significant complications can be avoided.
Initially, the full endoscopic surgery was indicated only for herniated nucleus pulposus (HNP) (5,6). Therefore, it was called transforaminal full endoscopic discectomy (TF-FED). Recently, the technique has been applied to the lumbar spinal canal stenosis due to the development of the high-speed drill and other advanced endoscopic instruments. Yeung and co-workers confirmed the importance of residual foraminal stenosis among patients with failed back syndrome (FBS) (7,8). In FBS patients, full endoscopic lumbar foraminoplasty (FELF) is effective and allows most patients to avoid fusion surgery (9). More recently, lateral recess stenosis was shown to be adequately decompressed via a transforaminal route under the local anesthesia (10,11), via the full endoscopic ventral facetectomy (FEVF).
In Japan, outpatient surgeries are still not the norm and admissions even after minimally invasive surgeries may be dictated by the health care system. We have treated six medical doctors who underwent endoscopic decompression for lumbar disorders. We are demonstrating the feasibility of performing effective endoscopic decompression surgery on an outpatient basis with early return to function.
Materials & methods
Patients
Patients were six male physicians. Their age was between 27–63 years of age (mean: 40.0 years). They consisted of one general medicine resident, one orthopedic surgeon, one urologic surgeon, three general surgeons. The orthopedic surgeon, who suffered from lateral recess stenosis at L4–5, underwent FEVF under the local anesthesia. The remaining patients underwent TF-FED for HNP. One patient had the HNP at L5–S1 and remaining four at L4–5. The operative time, estimated blood loss, surgery-related complications, clinical outcome, and the duration of sick leave before returning to work were recorded (Table 1).

Full table
Surgical technique & outcomes
All endoscopic surgeries, including TF-FED and FEVF, were performed under the local anesthesia. The surgical procedure of these surgeries of TF-FED (5,6) and TF-FEVF has been described elsewhere (10,11). Operative time ranged from 71 to 102 min. The estimated blood loss was minimal in all six patients. In the series, we did not encounter the surgery-related complications such as nerve root injury, hematoma, dural tear, surgical site infection, or others. Outcomes were reported in modified Macnab criteria as Excellent, Good, Fair, and Poor (12). In some patients, a foraminoplasty employing the ventral epiduroscopic observation was necessary. This technique has been described elsewhere (13). Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written permission is available for review by the Editor-in-Chief of this journal.
Results
Immediately after the surgery, the leg and back pain decreased in all patients. The earliest returning to was reported by the senior 63-year-old orthopedic surgeons who underwent TF-FEVF. He was highly motivated to return to his clinic and returned to clinical work within two days after the surgery. The most extended sick leave was reported by general medicine resident, who returned to his clinical duties two weeks postoperatively. He was not scheduled for clinical work until two weeks after surgery. However, his pain was had nearly subsided immediately after his surgery, and he attended a wedding ceremony the next day after the surgery. For all physicians, the mean duration of sick leave and return to clinical work responsibilities was 5.8±3.3 days (Table 1). At final follow-up 6 months postoperatively, the clinical outcomes were reported as Excellent in four and as Good in two patients. They were working as a physician in the original activity without any pain. Three illustrative case examples of the 6 patients of this case report are described in the following.
Case 1
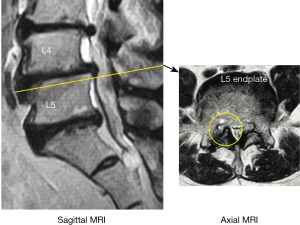
The patient is a 32-year-old general surgeon who failed three-months conservative treatment for unrelenting sciatica-type leg- and back pain. The pain interfered with his job since he had pain when performing surgery. The preoperative MRI scan demonstrated a right-sided L4/5 paracentral herniated disc causing lateral recess and foraminal stenosis. A postoperative MRI scan showed successful removal of the disc herniation with the TF-FED technique (Figure 1). A foraminoplasty was necessary to deal with the hypertrophic facet joint. The patient had an excellent complete resolution of his symptoms and returned to his surgical practice pain-free five days after the FED surgery. He was asymptomatic at final follow-up of two years and 6 months postoperatively. He did not have any symptoms or recurrence. The clinical outcome was rated as Excellent.

Case 2
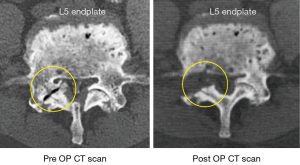
This patient is a 63-year-old orthopedic surgeon. He had been suffering from right leg pain due to L5 radiculopathy for more than a year. The severe right-sided L4/5 lateral recess stenosis at L4-5 was pointed out by himself on his preoperative MRI to this team of spine surgeons (Figure 2). When the pain became worse, and he could not continue to work in his outpatient clinic. In the absence of cauda equina syndrome, he opted for endoscopic surgery. His past medical history was significant for uncontrolled diabetes mellitus and coronary artery disease. Therefore, his uncomplicated endoscopic FEVF decompression surgery was performed successfully without complications under the local anesthesia. His side-by-side comparative pre- and postoperative CT scan is showing successful lateral recess decompression (Figure 3). Since he had to return to managing his private clinic, he quickly returned to his clinical duties two days after the surgery. At the final one-year follow-up, he continued to work at his clinic without any pain. The clinical outcome was rated as Good.
Case 3
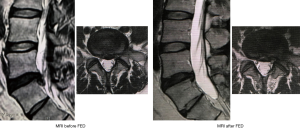
The patient is a 42-year-old male general surgeon. He suffered from symptomatic HNP at the left L5–6, where the L6 was the transitional vertebra. The left leg pain was intolerable, and he could not work as a physician. The neurological examination showed left S1 nerve root impingement signs with 4/5 weakness of flexor halluces longus (FHL), hypoesthesia over the 5th toe, and diminished Achilles tendon reflex. This surgeon patient opted for endoscopic transforaminal FED surgery under local anesthesia because he strongly hoped it would return him to his job. Figure 4 displays the preoperative MRI before FED surgery, demonstrating a slightly caudally migrated fragment resulting in S1 nerve root compression. It was successfully removed with the FEV procedure. Immediately after the surgery, leg pain dramatically decreased and returned to the job as a surgeon six days after the surgery. Numbness and hypoesthesia in the left foot persisted for some time postoperatively. However, six months after the surgery, all the symptoms had disappeared. The clinical outcome at the one-year final follow-up examination was rated as Excellent. The MRI after the surgery was demonstrated in Figure 4. Note the caudally migrated fragment had been removed and the S1 nerve root was shown to be decompressed.
Discussion
Traditional open surgery or microdiscectomy is still the gold standard for surgical intervention for HNP. Based on the recommendation of the North American Spine Society, most people with jobs that are not physically challenging can return to work in two to four weeks or less (14). Patients with jobs that require heavy lifting or operating heavy machinery that can cause intense vibration may need to wait at least six to eight weeks after surgery to return to work. There are no recommendations for physicians. Their job functional job requirements may vary considerably. In this case report of six physicians, we highlight the feasibility of early return to clinical duties after endoscopic full endoscopic decompression under the local anesthesia - a stark contrast to the norm in Japan.
The full endoscopic surgery has allowed extending the indications for minimally invasive endoscopic surgery from herniated disc to spinal stenosis. It allows for an early return to preoperative function. A recent literature review by Birkenmaier et al. corroborated faster postoperative rehabilitation, shorter hospital stays, and faster return to work with full endoscopic discectomy when compared to microsurgical techniques. (15) Ruetten et al. compared the endoscopic discectomy return to work data (25 days) with microsurgical discectomy (49 days) (16). Patients who underwent endoscopic surgery returned to work in half the time required for microdiscectomy patients. Mahesha reviewed his first 100 cases of full endoscopic lumbar discectomy and reported a mean duration for return to work of 36 days ranging from 2 to 100 days (17). In our series, 5 of the 6 physicians could return to their jobs within a week, and the remaining physician returned to his clinical duties within two weeks. Therefore, our return-to-work data compare favorably with the data published in the literature.
In this paper, we reported the early return to the original job by six medical doctors treated for sciatica-type leg- and back pain with the endoscopic decompression (FED/FEVF) under the local anesthesia. The mean duration for the return to clinical duties was 5.8 days postoperatively. These six case examples demonstrate the feasibility of early return to work after the full endoscopic surgery. In the authors' hands, the full endoscopic decompression is the preferred option to return professionals back to work with Excellent and Good clinical outcomes.
Acknowledgments
None.
Footnote
Conflicts of Interest: Koichi Sairyo, is a paid consultant for Japan MDM, Senko Medical, and Surgical Spine. However, his affiliation with these companies does not conflict with the content of this manuscript. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
References
- Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years' experience. Clin Orthop Relat Res 1989.9-23. [Crossref] [PubMed]
- Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med 2000;67:327-32. [PubMed]
- Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27:722-31. [Crossref] [PubMed]
- Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am 2007;38:363-72. abstract vi. [Crossref] [PubMed]
- Sairyo K, Egawa H, Matsuura T, et al. State of the art: Transforaminal approach for percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest. 2014;61:217-25. [Crossref] [PubMed]
- Sairyo K, Nagamachi A. State-of-the-art management of low back pain in athletes: Instructional lecture. J Orthop Sci 2016;21:263-72. [Crossref] [PubMed]
- Yeung A, Gore S. Endoscopic foraminal decompression for failed back surgery syndrome under local anesthesia. Int J Spine Surg 2014. [Crossref] [PubMed]
- Gore S, Yeung A. The "inside out" transforaminal technique to treat lumbar spinal pain in an awake and aware patient under local anesthesia: results and a review of the literature. Int J Spine Surg 2014. [Crossref] [PubMed]
- Yamashita K, Higashino K, Sakai T, et al. Percutaneous full endoscopic lumbar foraminoplasty for adjacent level foraminal stenosis following vertebral intersegmental fusion in an awake and aware patient under local anesthesia: A case report. J Med Invest 2017;64:291-5. [Crossref] [PubMed]
- Sairyo K, Higashino K, Yamashita K, et al. A new concept of transforaminal ventral facetectomy including simultaneous decompression of foraminal and lateral recess stenosis: Technical considerations in a fresh cadaver model and a literature review. J Med Invest 2017;64:1-6. [Crossref] [PubMed]
- Sairyo K, Chikawa T, Nagamachi A. State-of-the-art transforaminal percutaneous endoscopic lumbar surgery under local anesthesia: Discectomy, foraminoplasty, and ventral facetectomy. J Orthop Sci 2018;23:229-36. [Crossref] [PubMed]
- Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am 1971;53:891-903. [Crossref] [PubMed]
- Henmi T, Terai T, Hibino N, et al. Percutaneous endoscopic lumbar discectomy utilizing ventral epiduroscopic observation technique and foraminoplasty for transligamentous extruded nucleus pulposus: technical note. J Neurosurg Spine 2016;24:275-80. [Crossref] [PubMed]
- Patient Education Committee, North American Spine Society. Lumbar (Open) Microscopic Discectomy. Available online: https://www.spine.org/KnowYourBack/Treatments/SurgicalOptions/LumbarMicroscopicDiscectomy
- Birkenmaier C, Komp M, Leu HF, et al. The current state of endoscopic disc surgery: review of controlled studies comparing full-endoscopic procedures for disc herniations to standard procedures. Pain Physician 2013;16:335-44. [PubMed]
- Ruetten S, Komp M, Merk H, et al. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:931-9. [Crossref] [PubMed]
- Mahesha K. Percutaneous endoscopic lumbar discectomy: Results of first 100 cases. Indian J Orthop 2017;51:36-42. [Crossref] [PubMed]


