
Mini-open sacroiliac joint fusion with direct bone grafting and minimally invasive fixation using intraoperative navigation
Introduction
Low back pain is a common problem in the United States affecting a majority of all adults at some point in their lives (1). The sacroiliac joint has received greater recognition as a possible source of pain in the etiology of chronic low back pain. Up to 30% of patients presenting with low back pain will have contributions from a painful sacroiliac joint, often with concomitant lumbar degenerative findings (2-5).
The diagnosis of sacroiliac pain has historically been challenging. The current gold-standard is a fluoroscopically guided intra-articular injection of local anesthesia (6). Subsequent management is primarily non-surgical. Modalities include anti-inflammatories, physical therapy (PT), local steroid injections, radiofrequency ablation, manipulation, and prolotherapy with arthrodesis reserved for patients failing conservative treatments (6). There is a significant economic burden in the United States for conservative care of degenerative sacroiliac pathology (7).
Open sacroiliac arthrodesis was initially described in the 1920s (8-10) for degenerative sacroiliac changes secondary to tuberculosis, traumatic arthritis, and non-traumatic arthritis. Open sacroiliac fusion techniques have high complication rates, significant surgical morbidity from large incisions and increased blood loss, high nonunion rates, and variable patient satisfaction (11-13).
Within the last 10 years, minimally invasive sacroiliac fusion techniques have proven to be safe and effective, and are becoming the new standard of care for surgical patients. They are reported to reduced morbidity and improve many of the factors that plagued open techniques (14-16). By 2012, 85% of sacroiliac joint (SIJ) fusions utilized the minimally invasive option (17). Various methods have been described in the literature, most frequently including the insertion of triangular titanium implants with an overlying porous titanium plasma spray. These techniques utilize fluoroscopy for implant placement and rely on drilling and broaching over a guidewire across the sacroiliac joint to facilitate fusion. This technique relies on SIJ stabilization by the implants without directly opening or bone grafting the SIJ. Five-year results have shown sustained clinical improvements and radiographic evidence of stability (18).
Continued refinement and improvement of such techniques should however continue. The development of intraoperative 3D imaging plus computer-guided navigation has demonstrated benefits for spinal instrumentation. Compared to conventional fluoroscopy, use of O-arm with navigation results in more accurate pedicle screw placement (19,20) and lower rates of facet joint violation (21). Our institution has modified the minimally invasive technique by utilizing three-dimensional navigation and also has level 1 evidence supporting its use over fluoroscopy for dysmorphic proximal sacral segments requiring sacroiliac screws in trauma (22). There are reports in the literature that describe the use of stereotactic guidance for navigated percutaneous sacroiliac fusion (23,24).
This study describes the initial cohort of patients from our institution who have undergone a modified technique for sacroiliac fusion. This novel technique involves using intraoperative O-arm imaging and navigation to place standard minimally invasive triangular titanium implants and a limited open computer-navigated approach to the sacroiliac joint that allows for the direct decortication and placement of bone graft within the sacroiliac joint.
Methods
Study design
This is an institutional review board (IRB) approved (COMIRB #16-2216) retrospective study of adult patients who underwent our novel technique for mini-open sacroiliac joint fusion. All surgeries were performed by one of the two senior authors, Christopher J. Kleck or Vikas V. Patel, at a single institution. The surgical records were queried to identify all patients who underwent open arthrodesis of the sacroiliac joint with MIS Implants. The electronic medical records were reviewed to include patients who were 18 years or older at time of surgery, underwent primary sacroiliac fusion by the novel open technique described above, and had at least one postop follow-up visit at 6 weeks. Patients having revision sacroiliac procedures, sacroiliac arthrodesis by any other technique, and those undergoing concomitant spine procedures were excluded from the study. These criteria identified 50 patients having 57 open sacroiliac fusions between 2011 and 2016.
The records of each patient fitting the above criteria were reviewed to obtain preoperative lumbopelvic radiographic parameters, perioperative surgical details, and outcomes scores obtained in clinic. Our outpatient clinics prospectively obtain pre- and postoperative Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), and Denver Sacroiliac Joint Questionnaire (DSIJQ) outcomes scores as standard clinical practice. The DSIJQ is a novel outcomes measure for sacroiliac dysfunction devised by our institution and approved by our IRB. The DSIJQ questionnaire has the patient evaluate ten different domains of function including (I) sitting; (II) getting up from a chair; (III) walking; (IV) stairs; (V) getting in and out of a ca; (VI) bending at the waist/kneeling/squatting; (VII) lifting; (VIII) work/recreation/sex/social activities; (IX) sleep; and (X) stability; then choose a descriptive score on a scale of 0 (best) to 5 (worst) that describes their typical symptoms. The maximum (worst) possible points are out of 50. The final score is calculated by (total score/possible score) ×100.
The SIJ patient population had an extensive preoperative workup to determine their eligibility for surgery. The patients have attempted PT and steroidal injections. If the injection relieved the patient’s SIJ pain temporarily, the surgeon deemed it appropriate to undergo surgery. Further, if the SIJ injections did not relieve the patient’s back pain, then the patient did not undergo surgery as the SIJ was determined to not be the source of the pain. Due to the elective nature of the surgery, the patients were nicotine free pre-operatively to help facilitate fusion.
Surgical technique
Patients are positioned prone on a Jackson table with all boney prominences padded. The appropriate side buttocks and lower back are draped in sterile fashion. A 5 mm longitudinal incision is made over the posterior superior iliac spine for placement of the navigation reference frame To provide an imaging reference for the navigated portion of the procedure (24). (Stealth Navigation System, Medtronic, Ireland). An intraoperative 3D scan is performed with the O-arm (O-Arm System, Medtronic, Dublin, Ireland). Using the navigation instruments to identify the posterior-inferior SIJ, a 3 cm incision is made over the distal aspect of the sacroiliac joint and carried deep to the level of the sacroiliac joint capsule. The capsule is opened, allowing access to the joint. Using a navigated cannula, a guide pin is placed into and parallel to the synovial SIJ. A high-speed drill is then passed in slightly varied trajectories into the joint to decorticate the sacroiliac joint surfaces. The channel created within the sacroiliac joint is wide enough to allow placement of the navigation cannula through which a mixture of bone morphogenic protein, demineralized bone matrix, and locally collected autograft bone is introduced directly into the sacroiliac joint.
Navigation is then used to mark the ideal incisions on the posterolateral buttocks for placement of three implants across the sacroiliac joint. The skin is incised, and the muscle fibers are bluntly dissected down to the lateral ilium. A navigated cannula is used to guide placement of each guidewire from the ilium, across the sacroiliac joint, into the sacrum. The most common pattern for placement is two implants within S1 and one implant within S2. The length and diameter of each implant are estimated based on navigated projections. Each guidewire is over-drilled with a cannulated drill to create a pathway for the implant. Bone shavings from the drill are collected and placed into the SIJ at the posterior-inferior exposure. Fixation is provided by cannulated, titanium, porous-coated triangular implants (SI-Bone, San Jose, CA, USA). After placement of the implants, the lateral ilium is palpated to ensure that all implants are seated appropriately (without excess prominence). A repeat intraoperative O-arm scan is performed to confirm implant positioning, an example image is shown in Figure 1A. All wounds are closed in standard fashion. Postoperative restrictions include touch-down weight bearing on the operative extremity for 6 weeks. It is difficult to evaluate fusion of the SIJ without computed topography (CT) scans (25); however, the images do not show any signs of halo formation around the implants. CT imaging would likely show bridging bone; however, CT scans are not standard of care in the facility. In the absence of significant SIJ pain (evaluated by DSIJQ questionnaire and physical exams), the patient was assumed to be fused.

Results
Fifty patients were identified having 57 surgeries with 12 male and 38 female patients (see Table 1 for patient information). There were 32 right and 25 left sacroiliac fusion procedures. All patients received three sacroiliac 7 mm implants with length ranging from 40–55 mm. A 1-year postoperative X-ray is shown in Figure 1B,C. Table 2 displays the outcomes scores. Outcomes scores showed statistically significant improvement at all postoperative time periods in VAS and ODI with a similar trend in the DSIJQ. At 12 months the VAS score improved from 6.2 to 2.8, the ODI improved from 48.9 to 20.8 and the DSIJQ improved from 53.2 to 20.8.
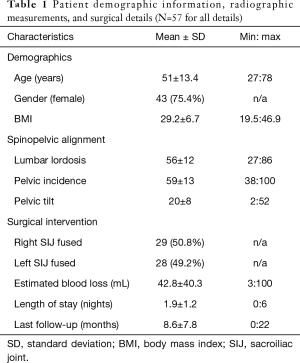
Full table
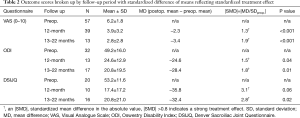
Full table
There were two complications identified in this series. One patient had intraoperative injury to a branch of the inferior gluteal artery following placement of the distal sacroiliac implant. This required an extended surgical exposure to identify the location of the hemorrhage and to place a vascular clip for hemostasis. The patient was taken to interventional radiology after the procedure while still under anesthesia to undergo angiography. No further bleeding was identified; coils were placed in the inferior gluteal artery prophylactically. Thus, this complication caused increased blood loss, surgical time, additional imaging, and an additional procedure. There were no clinical sequelae of this complication postoperatively. The other complication was postoperative buttock wound drainage identified in routine postoperative follow-up that resolved with a course of oral antibiotics.
Discussion
Minimally invasive percutaneous sacroiliac arthrodesis techniques, especially using triangular titanium implants, has gained clinical acceptance. There is a growing body of literature supporting their safety and improved outcomes over conservative care in the medium term with up to 1-year follow-up (14,15,26-29). Medium term results show improved clinical outcomes. One study demonstrates increased probability of returning to work compared to nonsurgical patients (30). There are fewer series published with follow-up greater than 1 year (25,31-35), but they maintain the general trend that minimally invasive sacroiliac arthrodesis with triangular implants is effective at relieving pain, improving outcomes scores postoperatively, and reducing disability. The longest reported series by Rudolf and Capobianco (18) demonstrates favorable results at 12 months that are maintained at 5 years. Though minimally invasive sacroiliac arthrodesis is still a relatively new technique, early results are promising.
MIS sacroiliac fusions are not without complications. A systematic review by Zaidi et al. (36) reviewed several studies which included 299 MIS sacroiliac fusions at an average follow-up of 21 months. Radiographically confirmed fusion rates ranged from 18–100% however this review noted that over 80% of studies did not include image-confirmed anatomic fusion as part of the outcomes assessment. Fusion rates for MIS sacroiliac fusion from other studies with dedicated radiographic imaging have been reported between 87–97% (18,25,37). Reoperation rates ranged from 0–17% (mean 6%). Another recent study by Schoell et al. (16) reviewed complication rates of MIS sacroiliac fusion within a Humana database. They identified a complication rate of 16.4% at 6 months however this included all types of complications including novel lumbar pathology, infection, and postoperative pain.
Some concern also remains regarding the longevity of SIJ stabilization without direct decortication and bone grafting of the joint itself. As many of the MIS techniques rely on stabilization without direct fusion of the joint, the potential for delayed loosening remains. While there is no consensus regarding the number of implants needed to achieve an SIJ fusion, the three-implant construct may provide the most stability. A single implant may allow continued motion, with the implant simply acting as an axis for rotation. Two implants may increase this stability, but by providing the third implant and in a diverging, triangular pattern, the maximum stability for the joint can be created. As with all orthopedic healing models, stability is necessary to achieve solid bony union. As cost is absolutely a factor, this would be an avenue for further research, to evaluate fusion with fewer implants utilizing the mini-open fusion technique.
There are several goals for this study. First, to contribute to the growing body of literature supporting the benefit of minimally invasive sacroiliac arthrodesis. Second, to describe a new surgical technique that allows open placement of bone graft directly into the sacroiliac joint in order to facilitate greater union rates. And third, to analyze and describe these patients’ short-term outcomes.
Average blood loss for this procedure is minimal at less than 100 mL. Most patients have a one or two-night inpatient stay, during which time they work with PT, primarily for touch down weight bearing gait training. There was progressive clinical improvement at all time periods observed in each of our three outcome scores. There was statistical significance (P<0.05) for each interval change in VAS compared to preoperative baseline, and at each interval 3 months and beyond for ODI. We were not able to demonstrate statistical significance using the DSIJQ outcome at 1-year follow-up due to insufficient numbers reporting but the trend was similar. Our complication rate of 2/57 (3.5%) is favorable compared to the described rate of complications for sacroiliac fusion procedures (11,16,35,36).
Specifically, the trials involving SI-Bone’s I-fuse implants were reviewed. Review of outcomes from their two-year follow-up trial describe a complication rate of 22% with five major adverse events deemed secondary to device or procedure and four subjects ultimately requiring revisions. Two of the revisions were after the first-year follow-up, outside the window of our study period. Summative post-market analysis of the iFuse from 2009 to 2014 illustrate one-year revision rates that progressively declined from 9.7% to 1.4% of which the two primary contributors were symptomatic malposition and symptom recurrence. Future studies with implementation of our technique at other centers will allow us to comparably delineate the safety of our technique.
There are several limitations of this study. This is a two-surgeon, single-center, retrospective, non-comparative study with the corresponding risk of bias. Our results may not be generalizable to all centers and populations. This surgical technique relies on having an O-arm and surgical navigation equipment that may not be available in other centers, though the techniques could be mimicked using fluoroscopy.
Conclusions
The scope of this study is to describe the initial safety and clinical efficacy of our modified technique. None of our patients in this series required reoperation during the study period but our follow-up is limited. We believe this technique for navigated, limited-open, sacroiliac joint fusion using minimally invasive implants holds optimistic promise for future study to include longer follow-up with dedicated radiographic analysis to demonstrate improved clinical outcomes, increased sacroiliac fusion, and decreased reoperation rates compared to traditional minimally invasive sacroiliac stabilization.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This is an institutional review board (IRB) approved (COMIRB #16-2216) retrospective study.
References
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-5. [Crossref] [PubMed]
- Bolt PM, Wahl MM, Schofferman J. The Roles of the Hip, Spine, Sacroiliac Joint, and Other Structures in Patients with Persistent Pain after Back Surgery. Semin Spine Surg 2008;20:14-9. [Crossref]
- Sembrano JN, Polly DW. How often is low back pain not coming from the back? Spine (Phila Pa 1976) 2009;34:E27-32. [Crossref] [PubMed]
- Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine 1995;20:31-7. [Crossref] [PubMed]
- Bernard TN Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res 1987.266-80. [PubMed]
- Dreyfuss P, Dreyer SJ, Cole A, et al. Sacroiliac joint pain. J Am Acad Orthop Surg 2004;12:255-65. [Crossref] [PubMed]
- Ackerman SJ, Polly DW, Knight T, et al. Nonoperative care to manage sacroiliac joint disruption and degenerative sacroiliitis: high costs and medical resource utilization in the United States Medicare population. J Neurosurg Spine 2014;20:354-63. [Crossref] [PubMed]
- Smith-Petersen M. Arthrodesis for tuberculosis of the sacro-iliac joint: study of the end-results. JAMA 1926.26-30. [Crossref]
- Smith-Petersen MN, Rogers W. End-result of arthrodesis of the sacro-iliac joint for arthritis-traumatic and non-traumatic. J Bone Jt Surg AM 1926;8:118-36.
- Smith-Petersen MN. Arthrodesis of the Sacroiliac Joint. a New Method of Approach. J Bone Jt Surg 1926;3:400-5.
- Buchowski JM, Kebaish KM, Sinkov V, et al. Functional and radiographic outcome of sacroiliac arthrodesis for the disorders of the sacroiliac joint. Spine J 2005;5:520-8. [Crossref] [PubMed]
- Waisbrod H, Krainick JU, Gerbershagen HU. Sacroiliac joint arthrodesis for chronic lower back pain. Arch Orthop Trauma Surg 1987;106:238-40. [Crossref] [PubMed]
- Schütz U, Grob D. Poor outcome following bilateral sacroiliac joint fusion for degenerative sacroiliac joint syndrome. Acta Orthop Belg 2006;72:296-308. [PubMed]
- Rudolf L. Sacroiliac Joint Arthrodesis-MIS Technique with Titanium Implants: Report of the First 50 Patients and Outcomes. Open Orthop J 2012;6:495-502. [Crossref] [PubMed]
- Duhon BS, Cher DJ, Wine KD, et al. Safety and 6-month effectiveness of minimally invasive sacroiliac joint fusion: A prospective study. Med Devices (Auckl) 2013;6:219-29. [PubMed]
- Schoell K, Buser Z, Jakoi A, et al. Postoperative complications in patients undergoing minimally invasive sacroiliac fusion. Spine J 2016;16:1324-32. [Crossref] [PubMed]
- Lorio MP, Polly DW, Ninkovic I, et al. Utilization of Minimally Invasive Surgical Approach for Sacroiliac Joint Fusion in Surgeon Population of ISASS and SMISS Membership. Open Orthop J 2014;8:1-6. [Crossref] [PubMed]
- Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J 2014;8:375-83. [Crossref] [PubMed]
- Shin MH, Ryu KS, Park CK. Accuracy and safety in pedicle screw placement in the thoracic and lumbar spines: Comparison study between conventional C-arm fluoroscopy and navigation coupled with O-arm?? guided methods. J Korean Neurosurg Soc 2012;52:204-9. [Crossref] [PubMed]
- Van de KE, Costa F, Van der PD, et al. A Prospective Multicenter Registry on the Accuracy of Pedicle Screw Placement in the Thoracic, Lumbar and Sacral Level With the Use of the O-arm® Imaging System and StealthStation® Navigation. Spine (Phila Pa 1976) 2012;37:E1580-7. [Crossref] [PubMed]
- Yson SC, Sembrano JN, Sanders PC, et al. Comparison of cranial facet joint violation rates between open and percutaneous pedicle screw placement using intraoperative 3-D CT (O-arm) computer navigation. Spine (Phila Pa 1976) 2013;38:E251-8. [Crossref] [PubMed]
- Matityahu A, Kahler D, Krettek C, et al. 3D Navigation is more Accurate than 2D Navigation or Conventional Fluoroscopy for Percutaneous Sacroiliac Screw Fixation in the Dysmorphic Sacrum: A Randomized Multicenter Study. J Orthop Trauma 2014;28:707-10. [Crossref] [PubMed]
- Lee DJ, Kim SB, Rosenthal P, et al. Stereotactic guidance for navigated percutaneous sacroiliac joint fusion. J Biomed Res 2016;30:162-7. [PubMed]
- Kleck CJ, Perry JM, Burger EL, et al. Sacroiliac Joint Treatment Personalized to Individual Patient Anatomy Using 3-Dimensional Navigation. Orthopedics 2016;39:89-94. [Crossref] [PubMed]
- Duhon BS, Bitan F, Lockstadt H, et al. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: 2-Year Follow-Up from a Prospective Multicenter Trial. Int J spine Surg 2016;10:13. [Crossref] [PubMed]
- Sturesson B, Kools D, Pflugmacher R, et al. Six-month outcomes from a randomized controlled trial of minimally invasive SI Joint fusion with triangular titanium implants vs conservative management. Eur Spine J 2017;26:708-19. [Crossref] [PubMed]
- Whang P, Cher D, Polly D, et al. Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. Int J spine Surg 2015;9:6. [Crossref] [PubMed]
- Duhon BS, Cher DJ, Wine KD, et al. Triangular Titanium Implants for Minimally Invasive Sacroiliac Joint Fusion: A Prospective Study. Global Spine J 2016;6:257-69. [Crossref] [PubMed]
- Sachs D, Capobianco R. Minimally invasive sacroiliac joint fusion: one-year outcomes in 40 patients. Adv Orthop 2013;2013:536128. [Crossref] [PubMed]
- Saavoss JD, Koenig L, Cher DJ. Productivity benefits of minimally invasive surgery in patients with chronic sacroiliac joint dysfunction. Clinicoecon Outcomes Res 2016;8:77-85. [PubMed]
- Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013;7:14. [Crossref] [PubMed]
- Sachs D, Kovalsky D, Redmond A, et al. Durable intermediate-to long-term outcomes after minimally invasive transiliac sacroiliac joint fusion using triangular titanium implants. Med Devices (Auckl) 2016.213-22. [Crossref] [PubMed]
- Polly DW, Swofford J, Whang PG, et al. Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. Int J Spine Surg 2016;10:28. [Crossref] [PubMed]
- Ledonio CG, Polly DW Jr, Swiontkowski MF, et al. Comparative effectiveness of open versus minimally invasive sacroiliac joint fusion. Med Devices (Auckl) 2014;7:187-93. [Crossref] [PubMed]
- Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg 2015;9:40. [Crossref] [PubMed]
- Zaidi HA, Montoure AJ, Dickman CA. Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. J Neurosurg Spine 2015;23:59-66. [Crossref] [PubMed]
- Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008;21:579-84. [Crossref] [PubMed]


