
Editorial on “Screening for adolescent idiopathic scoliosis: US preventive services task force recommendation statement”
The US Preventive Services Task Force (USPSTF) recently concluded that the current evidence is insufficient to assess the clinical benefits of adolescent idiopathic scoliosis (AIS) screening for children and adolescents aged 10 to 18 years (1). The recommendation differs from the 2004 USPSTF recommendation against AIS screening when it concluded that harms of screening exceeded the potential benefits. The decision to screen for AIS continues to be controversial in 2018, but there is a growing body of evidence over the last decade that show improved quality of life, aesthetics and curve progression with early scoliosis intervention. We will aim to critically evaluate the statement released by the USPSTF regarding the appropriateness of early AIS screening and assess recent guidelines presented by other societies that promote early AIS screening.
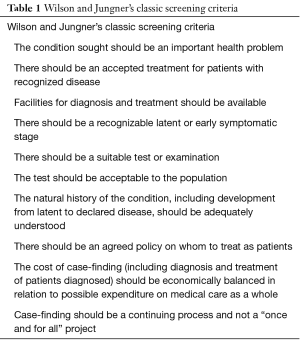
There are some important definitions and numbers to overview prior to discussing the 2018 USPSTF statement on AIS screening. Screening tests in medicine are defined as tools used to identify asymptomatic undiagnosed disease in a population, which will facilitate earlier care and prevent worsening of the disease. Wilson and Jungner’s screening criteria published by the World Health Organization (WHO) in 1968 still remains as the basic principle for a successful screening test (Table 1) (2). There are many well accepted screenings tests in medicine, which are routinely prescribed in the US due to their high diagnostic qualities and effective treatment methods on preventing or eliminating disease progression. Some screening tests, like the mammography, have varying degrees of acceptance in the community because they can lead to false-positive results and consequently unnecessary intervention, which may overshadow the potential benefits of the test (3).
Full table
AIS (defined as a Cobb angle ≥10°) is a condition in children to adolescent population (age 10–18 years old) with an estimated prevalence of 0.2–1.1% (4). There are known gender differences in curve characteristics (5). AIS is undeniably a prevalent issue in the community that can lead to significant impact in the patient’s life if they are untreated. Many publications over the last decade discuss the positive roles of non-operative management from bracing to scoliosis specific physical therapy for disease management. Given that AIS affects up to 1.1% of the pediatric population (age 10–18 years old), an effective screening tool is necessary to assess asymptomatic patients with AIS who needs further close observation or treatment from a spine surgeon. AIS fits nicely into most of the Wilson and Jungner’s screening criteria, but controversy exists on the validity of AIS screening because we still have limited understanding for the accepted treatment, natural history and benefit to risk ratio of a positive test for the patient and community as a whole. Currently, less than half of the states in the US offer school scoliosis screening and screening practices vary across the world (6).
The recently published 2018 USPSTF AIS recommendation statement begins by highlighting the accuracy of screening tests to detect AIS. The statement reports that accuracy of screening was highest (93.8% sensitivity and 99.2% specificity) when three separate tests were used (forward bend test, scoliometer measurement, and Moiré topography) and the screening accuracy decreased with 1 or 2 screening tests (1). The USPSTF found no studies related to direct harms from screening (i.e., psychological harms or harms associated with confirmatory radiography). Although it is not mentioned in the USPSTF statement, the AIS screening tests have also proved to be cost-effective in recently published studies which further advocates their use. Thilagaratnam et al. reviewed the Singapore’s existing school-based scoliosis screening from 1999 to 2001 and showed that direct (costs of man power, transport and computer system maintenance) and indirect costs (time cost for parent accompanying child for bracing, transport and other intangibles) of screening was around $450,000 per year, which was less than the total costs of surgery and follow up valued around $1,300,000 per year (7). Other studies show similar beneficial cost-effectiveness with screening and low absolute screening tests costs (8,9). Although the screening tests were highly accurate and cost-effective with minimal to no direct harm to the population as a whole, the recommendation statement was unable to confirm long-term health benefit of treating AIS after detection. In another words, there is adequate proof in our ability to accurately diagnose AIS, but there is inadequate literature on the clinical efficacy of AIS treatment in asymptomatic patients with Cobb angle <50° at diagnosis.
The unclear benefit of treating AIS stems from our conflicting understanding of the natural history of AIS progression. The early long-term idiopathic scoliosis studies inaccurately portrayed AIS progression leading to significant disability from back pain and cardiopulmonary dysfunction (10-12). These studies failed to separate patients with AIS and early onset scoliosis (EOS) and Weinsten et al. correctly separated these two entities and published a 50-year natural history study for 117 untreated AIS patients in 2003 (13). The study concluded that there is “little physical impairment other than back pain and cosmetic concern” for untreated AIS patients, which makes non-operative or operative treatment for AIS hard to justify for the spine surgeons (13). However, with a closer look into their data and discussion, we can tease out some other information that are hidden in between the lines. The paper failed to further emphasize the incidence of chronic pain in untreated AIS patients which was twice as often compared with the control subjects who were selected from high disability environments (i.e., hospital clinics). The pulmonary function results also showed patients with a Cobb angle of greater than 50° was associated with significantly increased odds of developing shortness of breath, which was not further discussed in the paper (13). Although there was no mortality secondary to untreated scoliosis, the apparent trend towards chronic back pain and pulmonary dysfunction for untreated AIS was apparent in Weinstein’s paper. The 2018 USPSTF recommendation remarks that “back pain is more common, but its effect on functioning or disability is unclear”, which is essentially asking for an arbitrary subjective score difference of back pain in untreated AIS patients and the control group. Such difference is undetermined in current literature, but the obvious fact that back pain leads to decreased quality of life is not rocket science and the need to quantify this may not be necessary. AIS treatment aims to increase quality of life for the patients and there is a large body of evidence pointing towards the increased benefit of handling the disease early on.
Typically, a successful screening tool prevents the worst case scenario for the patient from disease progression, which is pulmonary dysfunction, back pain, disability, psychological effects, cosmetic issues, and reduced quality of life for AIS (14,15). Non-operative management of AIS is initially offered to halt disease progression and prevent surgical intervention. Therefore, if we can surmise that non-operative management can have higher degrees of success in early stages of AIS, and ultimately prevent surgical management, we can make a good argument for having AIS screening as an effective tool for the medical community.
AIS treatment begins with non-operative management which basically entails bracing and physical therapy. The 2018 USPSTF recommendation statement agrees with the significant benefit associated with bracing when it is worn for at least 18 hours per day (1). Many recent high quality studies, including a randomized clinical trial and controlled clinical trials, showed clear clinical benefit and decreased curve progression for AIS patients using the brace (16-20). The efficacy of bracing treatment is hardly questioned in the statement and the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) clearly demonstrates the power of bracing by showing increased rate of treatment success in the intervention group (19). The SRS bracing cohort also reported on lower number of patients with curve past 45° at the time of follow up after bracing treatment (15). In addition to bracing therapy, tailored scoliosis-specific exercises showed Cobb angle reduction and increased quality of life compared to the control group performing generic exercises (21,22). The study participants in the bracing therapy had a Cobb angle of about 20° to 30°, and scoliosis-specific exercises were designed for patients with Cobb angle ranging from 10° to 25°, which implies that these two therapies were effective for patients with milder curves (1,21,22).
These studies help justify early scoliosis screening using the highly accurate aforementioned screening tests. Early screening leads to AIS patient referrals with minor curves, which is demonstrated in previous works. Lonstein et al. reported a decrease from 0.017% in 1974 to 0.004% in 1979 in operatively treated AIS patients in Minnesota after school scoliosis screening implementation (23). With early detection using the screening tests and subsequent non-operative treatment, the scoliosis curves decreased from 60° in 1971 to 42° in 1979 at the time of operation (23). This finding is further corroborated in recent study from Norway in 2012, which showed increased surgical frequency and higher curve magnitudes in initial office visits after termination of AIS screening (24). The AIS screening gives the opportunity for the patients and parents to seek effective care early and decrease the likelihood of curve progression and surgical management.
Beginning in 1984, the American Academy of Orthopaedic Surgeons (AAOS) and Scoliosis Research Society (SRS) began the push for early scoliosis screening with the understanding that AIS is a condition leading to decreased quality of life. In 2007, Pediatric Orthopaedic Society in North America (POSNA) and American Academy of Pediatrics (AAP) also recommended early detection of scoliosis. The most recent 2015 SRS/POSNA/AAOS/AAP position statement for AIS screening calls for screening examination for female at ages 10 and 12 years and male once at age 13 or 14 years (25). The statement encourages early detection of idiopathic scoliosis in adolescents with the aim to avoid surgical management. The main difference between the 2018 USPSTF and 2015 SRS/POSNA/AAOS/AAP statement derives from the interpretation of the natural history of untreated idiopathic scoliosis. Both agree on the high accuracy of screening tests and clinical efficacy of non-operative treatment using bracing therapy and scoliosis specific exercises. The 2015 SRS/POSNA/AAOS/AAP statement does not include studies on natural history of untreated AIS, but instead assumes that curve progression will lead to the point of surgery. The 2018 USPSTF statement found “no direct evidence on screening for AIS and health outcomes” and “inadequate evidence on the association between reduction in spinal curvature in adolescence and long term health outcomes in adulthood”, which is contrary to their initial description on the burden of the disease, which leads to “cosmetic deformity, reduced quality of life, disability, chronic back pain, social and psychological effects, functional limitations, and pulmonary disorders” (1). This is further proven in aforementioned Weinstein’s 50 year follow up and other works (13-15). There may be limited evidence on direct correlation between curve progression and negative health outcomes determined by subject outcome scores, but it is fair to say that there is a trend towards increased chronic back pain and pulmonary dysfunction with untreated AIS.
AIS screening remains controversial and the recent 2018 USPSTF recommendation statement reflects our current approach to screening in the US. There is no question that the existing screening tests are highly diagnostic and cost effective and non-operative management of scoliosis using bracing and scoliosis-specific therapy is clinically efficacious. According to the Wilson and Jungner’s classic screening criteria, the only criteria that remains unproven is the natural history of the disease, which is pointed out in the recent USPSTF statement. However, upon closer inspection of the data in recent studies, there is a clear trend towards decreased quality of life for patients with untreated AIS who continue to have chronic back pain, decreased pulmonary function, and psychological detriments throughout their lives. The 2015 SRS/POSNA/AAOS/AAP position statement targets the population with higher likelihood of developing symptomatic scoliosis and recommends screening for female at ages 10 and 12 years and male once at age 13 or 14 years, which will increase early detection and decrease false-positive referrals (25). The AIS screening in the right population allows early efficacious non-operative treatment for mild curves and prevent future surgical management and lower quality of life. The screening tests have minimal drawbacks with low absolute economic costs and potential for impressive benefits. The USPSTF recommendation changed from against AIS screening in 2004 to insufficient evidence for or against AIS screening in 2018. However, we may easily have a case for AIS screening already in 2018 with a different interpretation of existing data.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- US Preventive Services Task Force, Grossman DC, Curry SJ, et al. Screening for Adolescent Idiopathic Scoliosis. JAMA 2018;319:165. [Crossref] [PubMed]
- Wilson JM, Jungner YG. Principles and practice of mass screening for disease. Bol Oficina Sanit Panam 1968;65:281-393. [PubMed]
- Karimi P, Shahrokni A, Moradi S. Evidence for U.S. Preventive Services Task Force (USPSTF) Recommendations Against Routine Mammography for Females between 40-49 Years of Age. Asian Pac J Cancer Prev 2013;14:2137-9. [Crossref] [PubMed]
- Yong F, Wong HK, Chow KY. Prevalence of adolescent idiopathic scoliosis among female school children in Singapore. Ann Acad Med Singapore 2009;38:1056-63. [PubMed]
- Morais T, Bernier M, Turcotte F. Age- and sex-specific prevalence of scoliosis and the value of school screening programs. Am J Public Health 1985;75:1377-80. [Crossref] [PubMed]
- Altaf F, Drinkwater J, Phan K, et al. Systematic Review of School Scoliosis Screening. Spine Deform 2017;5:303-9. [Crossref] [PubMed]
- Thilagaratnam S. School-based screening for scoliosis: Is it cost-effective? Singapore Med J 2007;48:1012-7. [PubMed]
- Yawn BP, Yawn RA. The estimated cost of school scoliosis screening. Spine (Phila Pa 1976) 2000;25:2387-91. [Crossref] [PubMed]
- Lee CF, Fong DY, Cheung KM, et al. Costs of school scoliosis screening: A large, population-based study. Spine (Phila Pa 1976) 2010;35:2266-72. [Crossref] [PubMed]
- Dickson JH, Mirkovic S, Noble PC, et al. Results of operative treatment of idiopathic scoliosis in adults. J Bone Joint Surg Am 1995;77:513-23. [Crossref] [PubMed]
- Fowles JV, Drummond DS, L’Ecuyer S, et al. Untreated scoliosis in the adult. Clin Orthop Relat Res 1978.212-7. [PubMed]
- Ascani E, Bartolozzi P, Logroscino CA, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine (Phila Pa 1976) 1986;11:784-9. [Crossref] [PubMed]
- Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003;289:559-67. [Crossref] [PubMed]
- Dunn J, Henrikson NB, Morrison CC, et al. Screening for Adolescent Idiopathic Scoliosis: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2018;319:173-87. [Crossref] [PubMed]
- Dunn J, Henrikson NB, Morrison CC, et al. Screening for Adolescent Idiopathic Scoliosis: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US), 2018.
- Coillard C, Circo AB, Rivard CH. A prospective randomized controlled trial of the natural history of idiopathic scoliosis versus treatment with the SpineCor brace. Sosort Award 2011 winner. Eur J Phys Rehabil Med 2014;50:479-87. [PubMed]
- Wiemann JM, Shah SA, Price CT. Nighttime bracing versus observation for early adolescent idiopathic scoliosis. J Pediatr Orthop 2014;34:603-6. [PubMed]
- Weinstein SL, Dolan LA, Wright JG, et al. Effects of Bracing in Adolescents with Idiopathic Scoliosis. N Engl J Med 2013;369:1512-21. [Crossref] [PubMed]
- Weinstein SL, Dolan LA, Wright JG, et al. Design of the bracing in adolescent idiopathic scoliosis trial (BrAIST). Spine (Phila Pa 1976) 2013;38:1832-41. [Crossref] [PubMed]
- Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:823-7. [Crossref] [PubMed]
- Monticone M, Ambrosini E, Cazzaniga D, et al. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J 2014;23:1204-14. [Crossref] [PubMed]
- Negrini S, Zaina F, Romano M, et al. Specific exercises reduce brace prescription in adolescent idiopathic scoliosis: A prospective controlled cohort study with worst-case analysis. J Rehabil Med 2008;40:451-5. [Crossref] [PubMed]
- Lonstein JE, Bjorklund S, Wanninger MH, et al. Voluntary school screening for scoliosis in Minnesota. J Bone Joint Surg Am 1982;64:481-8. [Crossref] [PubMed]
- Adobor RD, Riise RB, Sørensen R, et al. Scoliosis detection, patient characteristics, referral patterns and treatment in the absence of a screening program in Norway. Scoliosis 2012;7:18. [Crossref] [PubMed]
- Hresko MT, Talwalkar V, Schwend R. Early detection of idiopathic scoliosis in adolescents. J Bone Joint Surg Am 2016;98:e67. [Crossref] [PubMed]


